Sunday Poster Session
Category: Esophagus
P0752 - Endoluminal Vacuum Therapy for Esophageal Perforation in a Critically Ill Patient With Granulomatosis With Polyangiitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JB
John Bruckbauer, MD, MPH (he/him/his)
Medical College of Wisconsin
Wauwatosa, WI
Presenting Author(s)
John Bruckbauer, MD, MPH, Talia Malik, MD, Matthew Peller, MD
Medical College of Wisconsin, Wauwatosa, WI
Introduction: Esophageal perforation demands prompt intervention due to its risk of life-threatening mediastinal infections. Endoluminal vacuum therapy (EVT) is an increasingly recognized and invaluable tool in the management of this complication. EVT applies negative pressure therapy directly to the site of perforation. This is accomplished through endoscopic placement of a porous sponge affixed to a transnasal tube. We present a case of esophageal perforation in a critically ill patient with newly diagnosed granulomatosis with polyangiitis (GPA).
Case Description/
Methods: A 52-year-old female with hypertension and hypothyroidism presented with dyspnea and cola-colored urine. She was diagnosed with pulmonary embolism and acute kidney injury requiring hemodialysis. Renal biopsy revealed ANCA-associated vasculitis. She developed hemoptysis requiring intubation, with bronchoscopy confirming diffuse alveolar hemorrhage. CT revealed an incidental esophageal perforation with a large mediastinal fluid collection, prompting transfer to our institution for surgical intervention. The cause of perforation was unclear, with the differential including nasogastric tube trauma, spontaneous rupture from coughing (Boerhaave syndrome), or as a direct result of her underlying vasculitis. Given the patient’s critical state and need for high dose corticosteroids, she was deemed a poor surgical candidate. Thus, gastroenterology was consulted. Esophagogastroduodenoscopy revealed a 3 cm esophageal perforation communicating with a 6 cm mediastinal cavity. EVT was initiated with nine sponge exchanges over 40 days. Nutrition was given by total parenteral nutrition followed by percutaneous gastrostomy tube. Eight-week follow-up CT esophagram demonstrated a small residual diverticulum with resolution of the mediastinal cavity and the patient’s diet was advanced to solids without difficulty (figure 1).
Discussion: The successful application of EVT in this medically complex patient demonstrates the increasing role for definitive endoscopic management of esophageal perforations. EVT works by achieving source control, promoting debridement/decontamination of the cavity, and expediting healing through improved reperfusion, which stenting alone cannot achieve. A drawback of EVT is its time and resource demands, averaging 4-9 sponge exchanges for closure. Although data is limited by small sample sizes, EVT is generally well-tolerated with minimal complications and a success rate of greater than 90%.
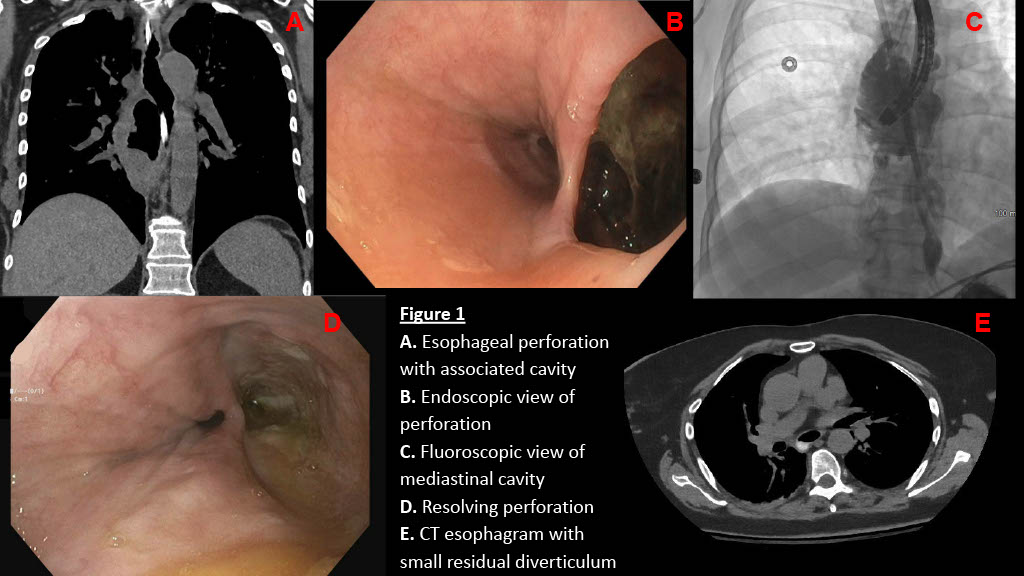
Figure: Endoscopic and radiographic findings, before and after endoluminal vacuum therapy
Disclosures:
John Bruckbauer indicated no relevant financial relationships.
Talia Malik indicated no relevant financial relationships.
Matthew Peller indicated no relevant financial relationships.
John Bruckbauer, MD, MPH, Talia Malik, MD, Matthew Peller, MD. P0752 - Endoluminal Vacuum Therapy for Esophageal Perforation in a Critically Ill Patient With Granulomatosis With Polyangiitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Medical College of Wisconsin, Wauwatosa, WI
Introduction: Esophageal perforation demands prompt intervention due to its risk of life-threatening mediastinal infections. Endoluminal vacuum therapy (EVT) is an increasingly recognized and invaluable tool in the management of this complication. EVT applies negative pressure therapy directly to the site of perforation. This is accomplished through endoscopic placement of a porous sponge affixed to a transnasal tube. We present a case of esophageal perforation in a critically ill patient with newly diagnosed granulomatosis with polyangiitis (GPA).
Case Description/
Methods: A 52-year-old female with hypertension and hypothyroidism presented with dyspnea and cola-colored urine. She was diagnosed with pulmonary embolism and acute kidney injury requiring hemodialysis. Renal biopsy revealed ANCA-associated vasculitis. She developed hemoptysis requiring intubation, with bronchoscopy confirming diffuse alveolar hemorrhage. CT revealed an incidental esophageal perforation with a large mediastinal fluid collection, prompting transfer to our institution for surgical intervention. The cause of perforation was unclear, with the differential including nasogastric tube trauma, spontaneous rupture from coughing (Boerhaave syndrome), or as a direct result of her underlying vasculitis. Given the patient’s critical state and need for high dose corticosteroids, she was deemed a poor surgical candidate. Thus, gastroenterology was consulted. Esophagogastroduodenoscopy revealed a 3 cm esophageal perforation communicating with a 6 cm mediastinal cavity. EVT was initiated with nine sponge exchanges over 40 days. Nutrition was given by total parenteral nutrition followed by percutaneous gastrostomy tube. Eight-week follow-up CT esophagram demonstrated a small residual diverticulum with resolution of the mediastinal cavity and the patient’s diet was advanced to solids without difficulty (figure 1).
Discussion: The successful application of EVT in this medically complex patient demonstrates the increasing role for definitive endoscopic management of esophageal perforations. EVT works by achieving source control, promoting debridement/decontamination of the cavity, and expediting healing through improved reperfusion, which stenting alone cannot achieve. A drawback of EVT is its time and resource demands, averaging 4-9 sponge exchanges for closure. Although data is limited by small sample sizes, EVT is generally well-tolerated with minimal complications and a success rate of greater than 90%.
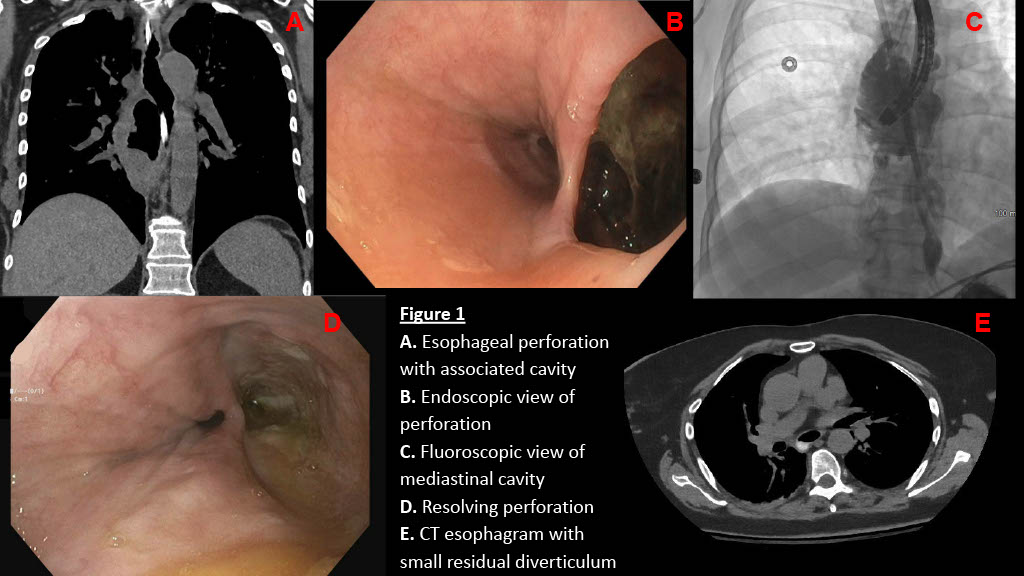
Figure: Endoscopic and radiographic findings, before and after endoluminal vacuum therapy
Disclosures:
John Bruckbauer indicated no relevant financial relationships.
Talia Malik indicated no relevant financial relationships.
Matthew Peller indicated no relevant financial relationships.
John Bruckbauer, MD, MPH, Talia Malik, MD, Matthew Peller, MD. P0752 - Endoluminal Vacuum Therapy for Esophageal Perforation in a Critically Ill Patient With Granulomatosis With Polyangiitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
