Sunday Poster Session
Category: Esophagus
P0745 - Black Esophagus in Pancreatic Cancer-Associated Necrotizing Pancreatitis: A Case Report and Review of the Literature
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Jeffrey Li
University of California Los Angeles David Geffen School of Medicine
Alameda, CA
Presenting Author(s)
Jeffrey Li, 1, Preetha Iyengar, MD2, Guy A. Weiss, MD2
1University of California Los Angeles David Geffen School of Medicine, Alameda, CA; 2University of California Los Angeles Medical Center, Los Angeles, CA
Introduction: Acute esophageal necrosis (AEN) is a rare condition marked by circumferential black discoloration of the esophageal mucosa, typically seen in shock or critical illness. While pancreatitis and malignancy have been separately linked to AEN, their co-occurrence has not been previously reported. We present a fatal case of AEN associated with necrotizing pancreatitis and newly diagnosed metastatic pancreatic adenocarcinoma.
Case Description/
Methods: A 75-year-old male with recurrent idiopathic acute pancreatitis presented with abdominal pain, ascites, and diffuse lymphadenopathy. Lipase was elevated at 259 U/L (ref. 9-63 U/L). Computed tomography showed a lobulated, hypodense pancreatic mass with fat stranding, concerning for necrotizing pancreatitis. Magnetic resonance cholangiopancreatography showed pancreatic ductal dilation without gallstones. Cytology from ascitic fluid and lymph node biopsy confirmed metastatic adenocarcinoma. On hospital day 4, the patient developed coffee-ground emesis. Upper endoscopy revealed diffuse black discoloration and ischemic changes throughout the esophagus consistent with AEN (Figure 1). Conservative management included intravenous pantoprazole (8 mg/h), fluid resuscitation, and avoidance of nasogastric tubes and NSAIDs. He developed sepsis with multiorgan failure within 24 hours and died. No autopsy was performed.
Discussion: AEN is rare, seen in 0.01-0.28% of upper endoscopies with a 30-day mortality rate of 20-30%, and is thought to result from severe ischemic or chemical injury. While most cases are associated with hypovolemia or gastric outlet obstruction, malignancy and pancreatitis are less common. Malignancy is present in 10–29% of AEN cases; however, pancreatic cancer is rare, with only three published cases. One review reported pancreatitis in 4.5% of AEN cases. A separate review of 319 patients with AEN found benign pancreatic disease in 6.9%, with four necrotizing pancreatitis cases—three alcohol-related, one gallstone-related. Our case uniquely describes AEN secondary to pancreatic cancer-associated necrotizing pancreatitis. Although our patient had a Ranson score of 4, typically associated with 15% mortality, his rapid decline after AEN onset suggests it may signal irreversible decompensation not captured by initial severity indices. This case underscores the importance of early endoscopy for GI bleeding in critically ill patients and suggests AEN may serve as a prognostic marker with implications for management and goals-of-care discussions.
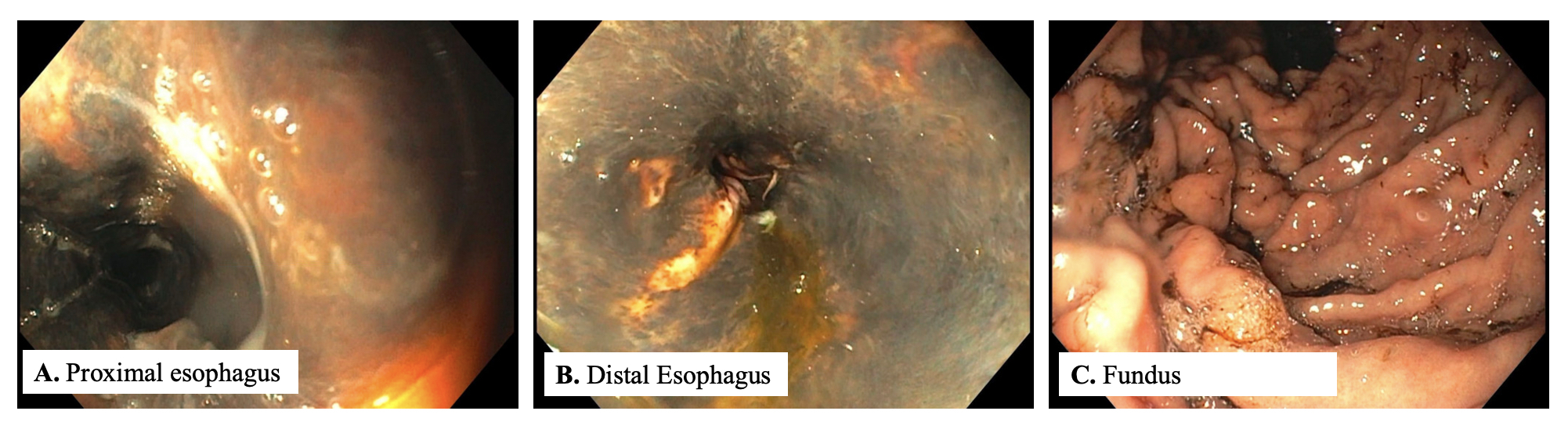
Figure: Figure 1.
Esophagogastroduodenoscopy showing mucosal friability, dark pigmentation, and ischemic changes extending from the proximal (A) to distal esophagus (B), consistent with acute esophageal necrosis. Gastric body and fundus (C) were well-visualized with small gastric erosions and hematin, but no ischemic changes.
Disclosures:
Jeffrey Li indicated no relevant financial relationships.
Preetha Iyengar indicated no relevant financial relationships.
Guy Weiss: Guidepoint – Consultant. Regeneron – Consultant.
Jeffrey Li, 1, Preetha Iyengar, MD2, Guy A. Weiss, MD2. P0745 - Black Esophagus in Pancreatic Cancer-Associated Necrotizing Pancreatitis: A Case Report and Review of the Literature, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Los Angeles David Geffen School of Medicine, Alameda, CA; 2University of California Los Angeles Medical Center, Los Angeles, CA
Introduction: Acute esophageal necrosis (AEN) is a rare condition marked by circumferential black discoloration of the esophageal mucosa, typically seen in shock or critical illness. While pancreatitis and malignancy have been separately linked to AEN, their co-occurrence has not been previously reported. We present a fatal case of AEN associated with necrotizing pancreatitis and newly diagnosed metastatic pancreatic adenocarcinoma.
Case Description/
Methods: A 75-year-old male with recurrent idiopathic acute pancreatitis presented with abdominal pain, ascites, and diffuse lymphadenopathy. Lipase was elevated at 259 U/L (ref. 9-63 U/L). Computed tomography showed a lobulated, hypodense pancreatic mass with fat stranding, concerning for necrotizing pancreatitis. Magnetic resonance cholangiopancreatography showed pancreatic ductal dilation without gallstones. Cytology from ascitic fluid and lymph node biopsy confirmed metastatic adenocarcinoma. On hospital day 4, the patient developed coffee-ground emesis. Upper endoscopy revealed diffuse black discoloration and ischemic changes throughout the esophagus consistent with AEN (Figure 1). Conservative management included intravenous pantoprazole (8 mg/h), fluid resuscitation, and avoidance of nasogastric tubes and NSAIDs. He developed sepsis with multiorgan failure within 24 hours and died. No autopsy was performed.
Discussion: AEN is rare, seen in 0.01-0.28% of upper endoscopies with a 30-day mortality rate of 20-30%, and is thought to result from severe ischemic or chemical injury. While most cases are associated with hypovolemia or gastric outlet obstruction, malignancy and pancreatitis are less common. Malignancy is present in 10–29% of AEN cases; however, pancreatic cancer is rare, with only three published cases. One review reported pancreatitis in 4.5% of AEN cases. A separate review of 319 patients with AEN found benign pancreatic disease in 6.9%, with four necrotizing pancreatitis cases—three alcohol-related, one gallstone-related. Our case uniquely describes AEN secondary to pancreatic cancer-associated necrotizing pancreatitis. Although our patient had a Ranson score of 4, typically associated with 15% mortality, his rapid decline after AEN onset suggests it may signal irreversible decompensation not captured by initial severity indices. This case underscores the importance of early endoscopy for GI bleeding in critically ill patients and suggests AEN may serve as a prognostic marker with implications for management and goals-of-care discussions.
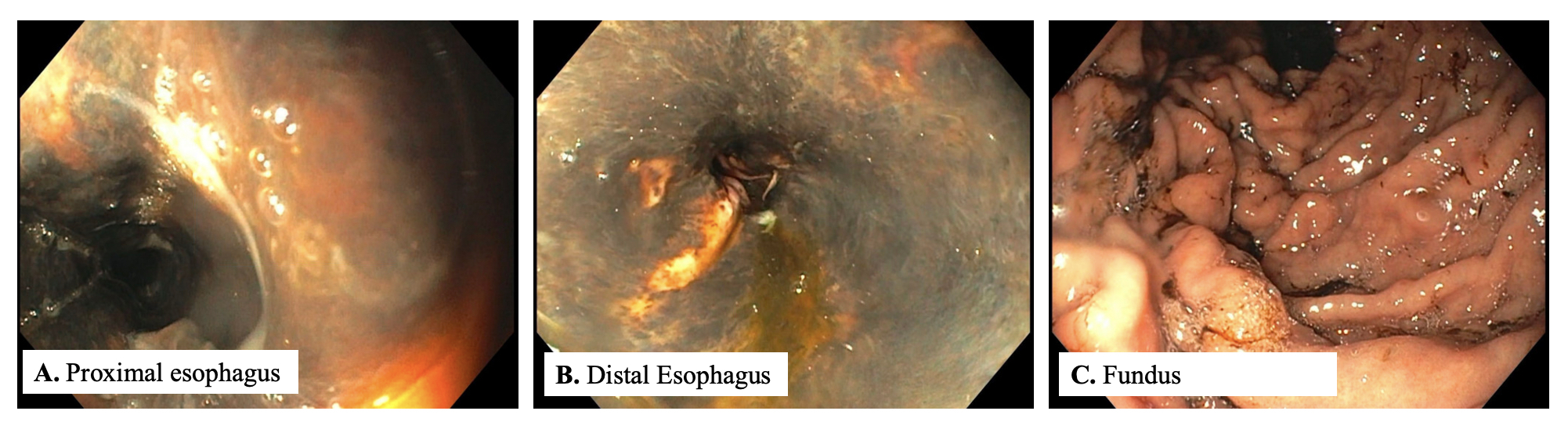
Figure: Figure 1.
Esophagogastroduodenoscopy showing mucosal friability, dark pigmentation, and ischemic changes extending from the proximal (A) to distal esophagus (B), consistent with acute esophageal necrosis. Gastric body and fundus (C) were well-visualized with small gastric erosions and hematin, but no ischemic changes.
Disclosures:
Jeffrey Li indicated no relevant financial relationships.
Preetha Iyengar indicated no relevant financial relationships.
Guy Weiss: Guidepoint – Consultant. Regeneron – Consultant.
Jeffrey Li, 1, Preetha Iyengar, MD2, Guy A. Weiss, MD2. P0745 - Black Esophagus in Pancreatic Cancer-Associated Necrotizing Pancreatitis: A Case Report and Review of the Literature, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
