Sunday Poster Session
Category: Esophagus
P0729 - Megaesophagus Causing Respiratory Failure: Diagnosis of Achalasia via EndoFLIP
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Sarah Rahni, DO, MBA
Westchester Medical Center
Valhalla, NY
Presenting Author(s)
Sarah Rahni, DO, MBA, Wei Tang, MD, Maxwell Charlat, MD, Naveena Sunkara, MD, Beth Schorr-Lesnick, MD, FACG
Westchester Medical Center, Valhalla, NY
Introduction: Achalasia is characterized by impaired relaxation of the lower esophageal sphincter and aperistalsis of the distal 2/3 of the esophagus. It can progress to esophageal dilation and megaesophagus (diameter >6 cm) in ~ 10% of patients. This can cause severe dysphagia, regurgitation, chest pain, and weight loss. Management depends on classifying achalasia into one of 3 phenotypes and thereafter assessing patient candidacy for surgical or endoscopic intervention. We present a case of a patient with cough and weight loss, who was found to have megaesophagus causing recurrent aspiration and acute respiratory failure, later diagnosed with type I achalasia on EndoFLIP.
Case Description/
Methods: A 69-year-old with achalasia presented with 2 days of dyspnea and 3 weeks of productive cough. He lost 15 pounds in 4 months after starting Tirzepatide. His achalasia was diagnosed 30 years earlier with manometry, but he was unsure of which subtype, and it was unsuccessfully treated with one attempt at balloon dilatation. On arrival, the patient was in respiratory distress: tachypneic to 28, hypoxic to 91%, and confused. He was intubated; a CT angiogram ruled out pulmonary embolism but showed a right lower lobe mucus plug and a fluid-filled and massively dilated esophagus to >7 cm. Endoscopy was performed which revealed a dilated fluid filled esophagus with retained food. An endoscopic PEG-J was then placed to prevent further aspiration. He was extubated and planned for outpatient follow up for further achalasia evaluation and management, however he returned 1 month later with G-J dislodgement, and underwent EGD with EndoFLIP which revealed at 60 ml the distensibility index was 1.3-1.5 mm2/mmHg [normal >2] and the diameter was 6.8-7.2 mm. [normal >16 mm]. No peristalsis was visualized. At 70 ml the diameter was 10.5-11.1 mm. The patient was diagnosed with type I achalasia and planned for Heller myotomy.
Discussion: Esophageal pathology should be considered in patients with unexplained respiratory symptoms. His weight loss was attributed solely to Tirzepatide, however, it could have been exacerbated by achalasia. Type I achalasia was diagnosed solely on EndoFLIP and patient is planned for appropriate treatment based on subtype, raising the question of whether manometry is truly necessary for diagnosis when EndoFLIP is available. More studies need to be performed to elucidate this. Timely interventions for achalasia can prevent progression of disease and therefore reduce morbidity and improve outcomes.
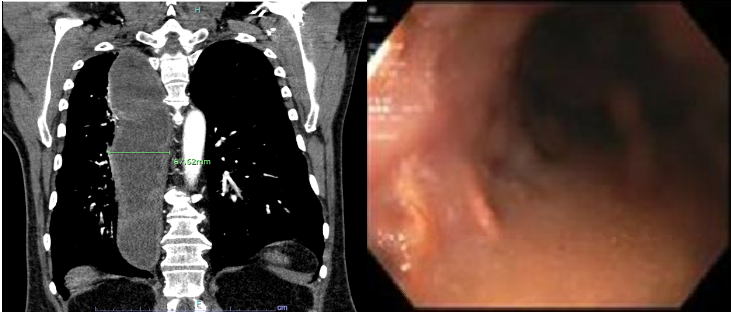
Figure: CT demonstrating megaesophagus [left], EGD showing dilated fluid-filled esophagus [right]
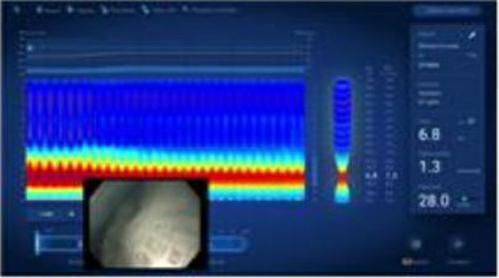
Figure: EndoFLIP at 60 mL with DI 1.3-1.5 mm2/mmHg, diameter 6.8-7.2 cm
Disclosures:
Sarah Rahni indicated no relevant financial relationships.
Wei Tang indicated no relevant financial relationships.
Maxwell Charlat indicated no relevant financial relationships.
Naveena Sunkara indicated no relevant financial relationships.
Beth Schorr-Lesnick indicated no relevant financial relationships.
Sarah Rahni, DO, MBA, Wei Tang, MD, Maxwell Charlat, MD, Naveena Sunkara, MD, Beth Schorr-Lesnick, MD, FACG. P0729 - Megaesophagus Causing Respiratory Failure: Diagnosis of Achalasia via EndoFLIP, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Westchester Medical Center, Valhalla, NY
Introduction: Achalasia is characterized by impaired relaxation of the lower esophageal sphincter and aperistalsis of the distal 2/3 of the esophagus. It can progress to esophageal dilation and megaesophagus (diameter >6 cm) in ~ 10% of patients. This can cause severe dysphagia, regurgitation, chest pain, and weight loss. Management depends on classifying achalasia into one of 3 phenotypes and thereafter assessing patient candidacy for surgical or endoscopic intervention. We present a case of a patient with cough and weight loss, who was found to have megaesophagus causing recurrent aspiration and acute respiratory failure, later diagnosed with type I achalasia on EndoFLIP.
Case Description/
Methods: A 69-year-old with achalasia presented with 2 days of dyspnea and 3 weeks of productive cough. He lost 15 pounds in 4 months after starting Tirzepatide. His achalasia was diagnosed 30 years earlier with manometry, but he was unsure of which subtype, and it was unsuccessfully treated with one attempt at balloon dilatation. On arrival, the patient was in respiratory distress: tachypneic to 28, hypoxic to 91%, and confused. He was intubated; a CT angiogram ruled out pulmonary embolism but showed a right lower lobe mucus plug and a fluid-filled and massively dilated esophagus to >7 cm. Endoscopy was performed which revealed a dilated fluid filled esophagus with retained food. An endoscopic PEG-J was then placed to prevent further aspiration. He was extubated and planned for outpatient follow up for further achalasia evaluation and management, however he returned 1 month later with G-J dislodgement, and underwent EGD with EndoFLIP which revealed at 60 ml the distensibility index was 1.3-1.5 mm2/mmHg [normal >2] and the diameter was 6.8-7.2 mm. [normal >16 mm]. No peristalsis was visualized. At 70 ml the diameter was 10.5-11.1 mm. The patient was diagnosed with type I achalasia and planned for Heller myotomy.
Discussion: Esophageal pathology should be considered in patients with unexplained respiratory symptoms. His weight loss was attributed solely to Tirzepatide, however, it could have been exacerbated by achalasia. Type I achalasia was diagnosed solely on EndoFLIP and patient is planned for appropriate treatment based on subtype, raising the question of whether manometry is truly necessary for diagnosis when EndoFLIP is available. More studies need to be performed to elucidate this. Timely interventions for achalasia can prevent progression of disease and therefore reduce morbidity and improve outcomes.
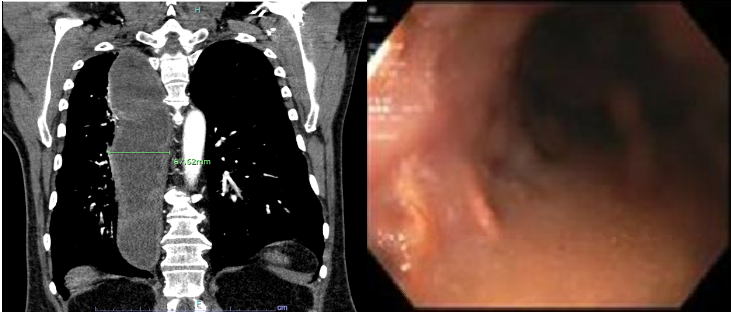
Figure: CT demonstrating megaesophagus [left], EGD showing dilated fluid-filled esophagus [right]
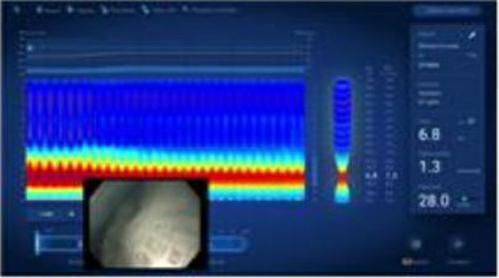
Figure: EndoFLIP at 60 mL with DI 1.3-1.5 mm2/mmHg, diameter 6.8-7.2 cm
Disclosures:
Sarah Rahni indicated no relevant financial relationships.
Wei Tang indicated no relevant financial relationships.
Maxwell Charlat indicated no relevant financial relationships.
Naveena Sunkara indicated no relevant financial relationships.
Beth Schorr-Lesnick indicated no relevant financial relationships.
Sarah Rahni, DO, MBA, Wei Tang, MD, Maxwell Charlat, MD, Naveena Sunkara, MD, Beth Schorr-Lesnick, MD, FACG. P0729 - Megaesophagus Causing Respiratory Failure: Diagnosis of Achalasia via EndoFLIP, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
