Sunday Poster Session
Category: Esophagus
P0726 - When Myotomy Fails: A Case of Persistent Dysphagia in a Patient with Overlapping Esophageal Motor Disorders
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Bianca Thakkar, DO
University of Connecticut Health
Farmington, CT
Presenting Author(s)
Bianca Thakkar, DO1, Rachael Hagen, DO1, Amir Masoud, MD2
1University of Connecticut Health, Farmington, CT; 2Hartford Healthcare/Connecticut GI, Fairfield, CT
Introduction: Dysphagia remains a challenging clinical entity, particularly in patients with overlapping or evolving esophageal motor disorders and persistent symptoms despite therapeutic interventions. While peroral endoscopic myotomy (POEM) and Heller myotomy are effective for achalasia and certain non-achalasia motility disorders, a subset of patients experience treatment failure due to incomplete myotomy, disease progression, or anatomical distortion. This case highlights the need for comprehensive physiologic evaluation and multidisciplinary management in complex cases.
Case Description/
Methods: A 64-year-old woman with chronic dysphagia for over a decade presented with persistent symptoms despite extensive evaluation and intervention. Initial endoscopies were unremarkable. High-resolution manometry (HRM) initially showed jackhammer esophagus, leading to medical therapy and multiple dilations without lasting relief. She underwent POEM, which failed to improve symptoms. Over 50 subsequent endoscopic dilations provided only transient benefit. Repeat manometry demonstrated achalasia with absent peristalsis and a distal esophageal “ledge.” Barium swallow confirmed aperistalsis with no mechanical obstruction. One year post-POEM, she underwent Heller myotomy, Dor fundoplication, and gastrostomy tube placement. However, she continued to report dysphagia, with repeat imaging consistent with ongoing achalasia. Despite maximal interventions, she required scheduled dilations and is now referred for further evaluation by a specialized esophageal motility team.
Discussion: This case illustrates the complexity of diagnosing and managing refractory dysphagia, especially in the context of overlapping or evolving motility disorders. Earlier use of HRM, FLIP, and multidisciplinary review may have clarified the diagnosis and guided more targeted therapy, potentially reducing unnecessary interventions and morbidity. Repeated reassessment after major interventions is essential to determine the underlying cause of persistent symptoms—whether mechanical, functional, or related to end-stage esophageal disease. In the presented case, the extensive number of endoscopies and dilations with limited benefit suggests a need for earlier, more comprehensive physiologic assessment. Ultimately, earlier integration of advanced diagnostic tools and expert review may have prevented unnecessary procedures and improved quality of life.
References:
1. Fass R. UpToDate, June 12, 2024.
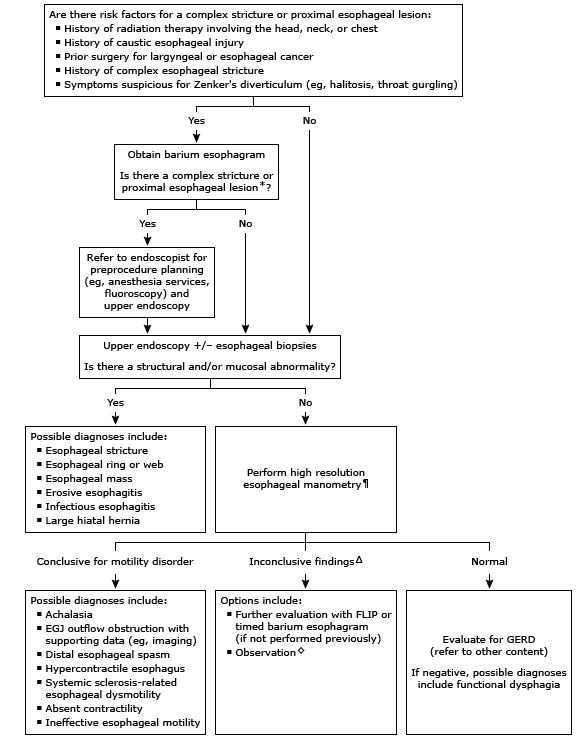
Figure: Figure 1. Algorithmic workup for Dysphagia: This flow chart outlines a structured approach to evaluating dysphagia, with key diagnostic steps—including EGD, barium swallow, and manometry, based on the nature (progressive vs. intermittent) and type (solids vs. liquids) of dysphagia to identify structural or motility-related etiologies [1].
Disclosures:
Bianca Thakkar indicated no relevant financial relationships.
Rachael Hagen indicated no relevant financial relationships.
Amir Masoud indicated no relevant financial relationships.
Bianca Thakkar, DO1, Rachael Hagen, DO1, Amir Masoud, MD2. P0726 - When Myotomy Fails: A Case of Persistent Dysphagia in a Patient with Overlapping Esophageal Motor Disorders, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health, Farmington, CT; 2Hartford Healthcare/Connecticut GI, Fairfield, CT
Introduction: Dysphagia remains a challenging clinical entity, particularly in patients with overlapping or evolving esophageal motor disorders and persistent symptoms despite therapeutic interventions. While peroral endoscopic myotomy (POEM) and Heller myotomy are effective for achalasia and certain non-achalasia motility disorders, a subset of patients experience treatment failure due to incomplete myotomy, disease progression, or anatomical distortion. This case highlights the need for comprehensive physiologic evaluation and multidisciplinary management in complex cases.
Case Description/
Methods: A 64-year-old woman with chronic dysphagia for over a decade presented with persistent symptoms despite extensive evaluation and intervention. Initial endoscopies were unremarkable. High-resolution manometry (HRM) initially showed jackhammer esophagus, leading to medical therapy and multiple dilations without lasting relief. She underwent POEM, which failed to improve symptoms. Over 50 subsequent endoscopic dilations provided only transient benefit. Repeat manometry demonstrated achalasia with absent peristalsis and a distal esophageal “ledge.” Barium swallow confirmed aperistalsis with no mechanical obstruction. One year post-POEM, she underwent Heller myotomy, Dor fundoplication, and gastrostomy tube placement. However, she continued to report dysphagia, with repeat imaging consistent with ongoing achalasia. Despite maximal interventions, she required scheduled dilations and is now referred for further evaluation by a specialized esophageal motility team.
Discussion: This case illustrates the complexity of diagnosing and managing refractory dysphagia, especially in the context of overlapping or evolving motility disorders. Earlier use of HRM, FLIP, and multidisciplinary review may have clarified the diagnosis and guided more targeted therapy, potentially reducing unnecessary interventions and morbidity. Repeated reassessment after major interventions is essential to determine the underlying cause of persistent symptoms—whether mechanical, functional, or related to end-stage esophageal disease. In the presented case, the extensive number of endoscopies and dilations with limited benefit suggests a need for earlier, more comprehensive physiologic assessment. Ultimately, earlier integration of advanced diagnostic tools and expert review may have prevented unnecessary procedures and improved quality of life.
References:
1. Fass R. UpToDate, June 12, 2024.
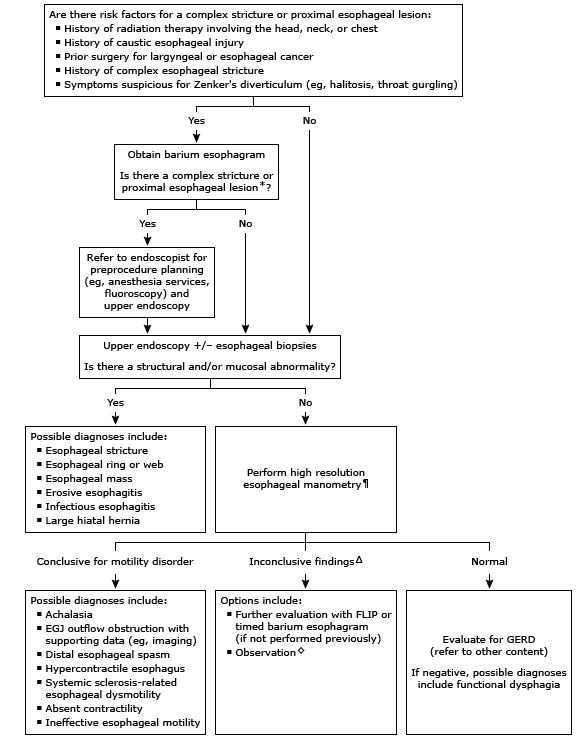
Figure: Figure 1. Algorithmic workup for Dysphagia: This flow chart outlines a structured approach to evaluating dysphagia, with key diagnostic steps—including EGD, barium swallow, and manometry, based on the nature (progressive vs. intermittent) and type (solids vs. liquids) of dysphagia to identify structural or motility-related etiologies [1].
Disclosures:
Bianca Thakkar indicated no relevant financial relationships.
Rachael Hagen indicated no relevant financial relationships.
Amir Masoud indicated no relevant financial relationships.
Bianca Thakkar, DO1, Rachael Hagen, DO1, Amir Masoud, MD2. P0726 - When Myotomy Fails: A Case of Persistent Dysphagia in a Patient with Overlapping Esophageal Motor Disorders, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
