Sunday Poster Session
Category: Esophagus
P0724 - A Rare Case of Dysphagia Aortica Presenting as Pseudoachalasia
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rishi Bolla, MD
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Rishi Bolla, MD, Ereny Demian, MD, Kevin Shah, MD, Rene Gomez-Esquivel, MD, John Jacobs, MD, FACG, Samuel Slone, MD
University of South Florida Morsani College of Medicine, Tampa, FL
Introduction: Dysphagia aortica is a condition characterized by esophageal obstruction due to extrinsic compression by the aorta. Its symptoms and imaging studies can mimic other causes of dysphagia, including achalasia. Here we present a case in which dysphagia aortica was diagnosed using endoscopic functional lumen imaging probe (FLIP) and endoscopic ultrasound (EUS).
Case Description/
Methods: An 82-year-old female with past medical history of kyphosis, prosthetic mitral valve, and diffuse atherosclerotic disease was referred to our institution for tertiary evaluation of chronic, progressive dysphagia with associated 60-pound weight loss. She had undergone esophagogastroduodenoscopy (EGD) previously which revealed dilated esophagus with food debris throughout, but no luminal obstruction.
Upon presentation, she underwent barium esophagram which showed a dilated esophagus concerning for achalasia. An EGD was performed which surprisingly revealed an area of external compression in the distal esophagus, just proximal to what was otherwise a widely patulous gastroesophageal junction (GEJ). Endoscopic FLIP was performed which showed normal distensibility index (DI) and minimum diameter of the GEJ. The area of suspected external compression showed DI 1.7mm2/mmHg and a minimum diameter of 11.6mm.
A computed tomography (CT) scan of the chest suggested esophageal compression by the aorta. Subsequent EUS revealed compression of the lower third of the esophagus by the aorta, confirming the diagnosis of dysphagia aortica. Given her age and poor functional status, the patient had a percutaneous gastrostomy tube placed for enteral nutrition pending evaluation for possible vascular intervention in future.
Discussion: There are few reported cases of dysphagia aortica in the literature, with some of the associated risk factors including older age, female sex, and history of kyphosis (1). Unlike in most cases of dysphagia aortica where patients have a clearly evident thoracic aortic aneurysm or tortuous aorta, our patient had an otherwise normal appearing aorta on CT imaging. (1, 2). Furthermore, she was symptomatic for nearly a year without a diagnosis resulting in severe protein-calorie malnutrition, which underscores the importance of recognizing this rare etiology of dysphagia.
References
1. Grimaldi S et al. Dysphagia aortica. Eur Surg. 2022;54(5):228-239.
2. Wilkinson JM et al. Diagnostic dilemmas in dysphagia aortica. European journal of cardio-thoracic surgery. 1997 Feb 1;11(2):222-7.
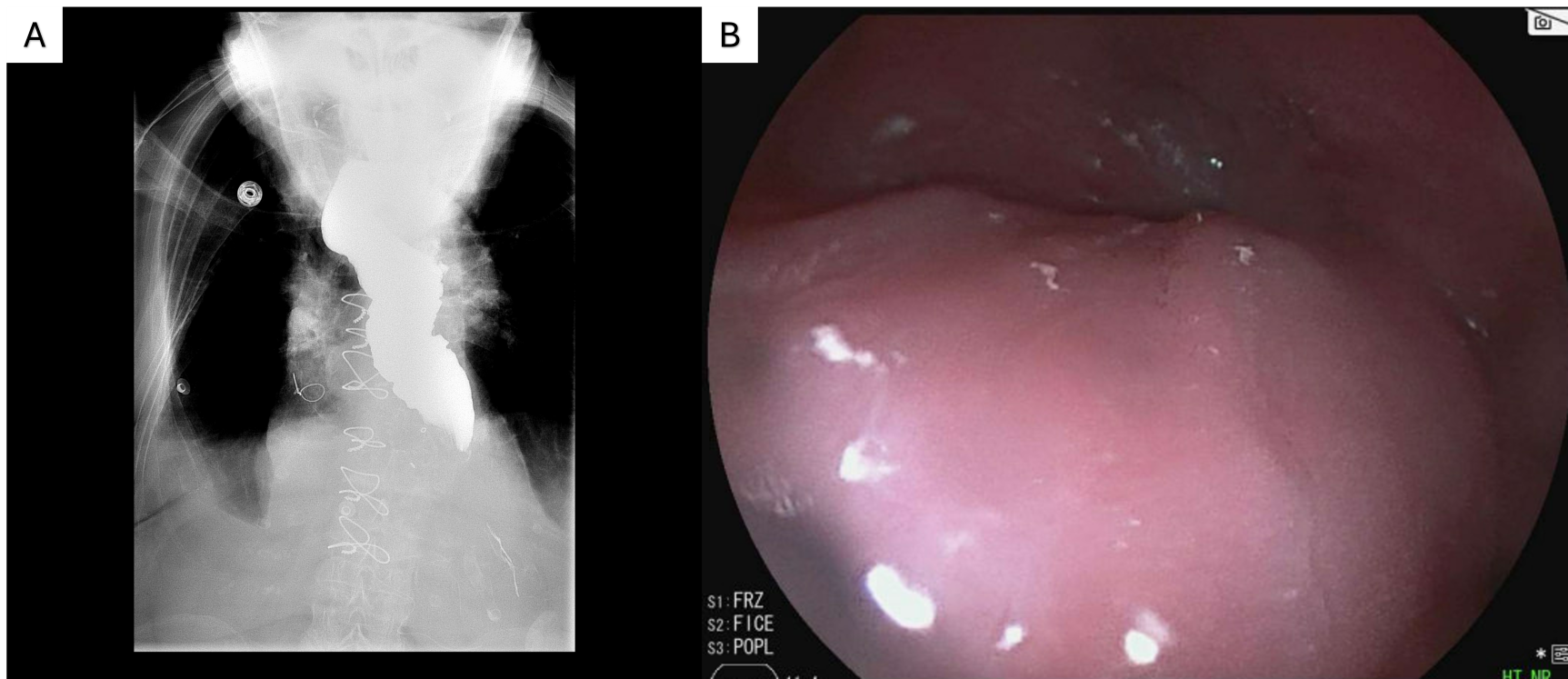
Figure: Figure 1: A) Barium esophagram showing dilated esophagus with delayed emptying, concerning for achalasia. B) EGD image of external compression of the distal esophagus.
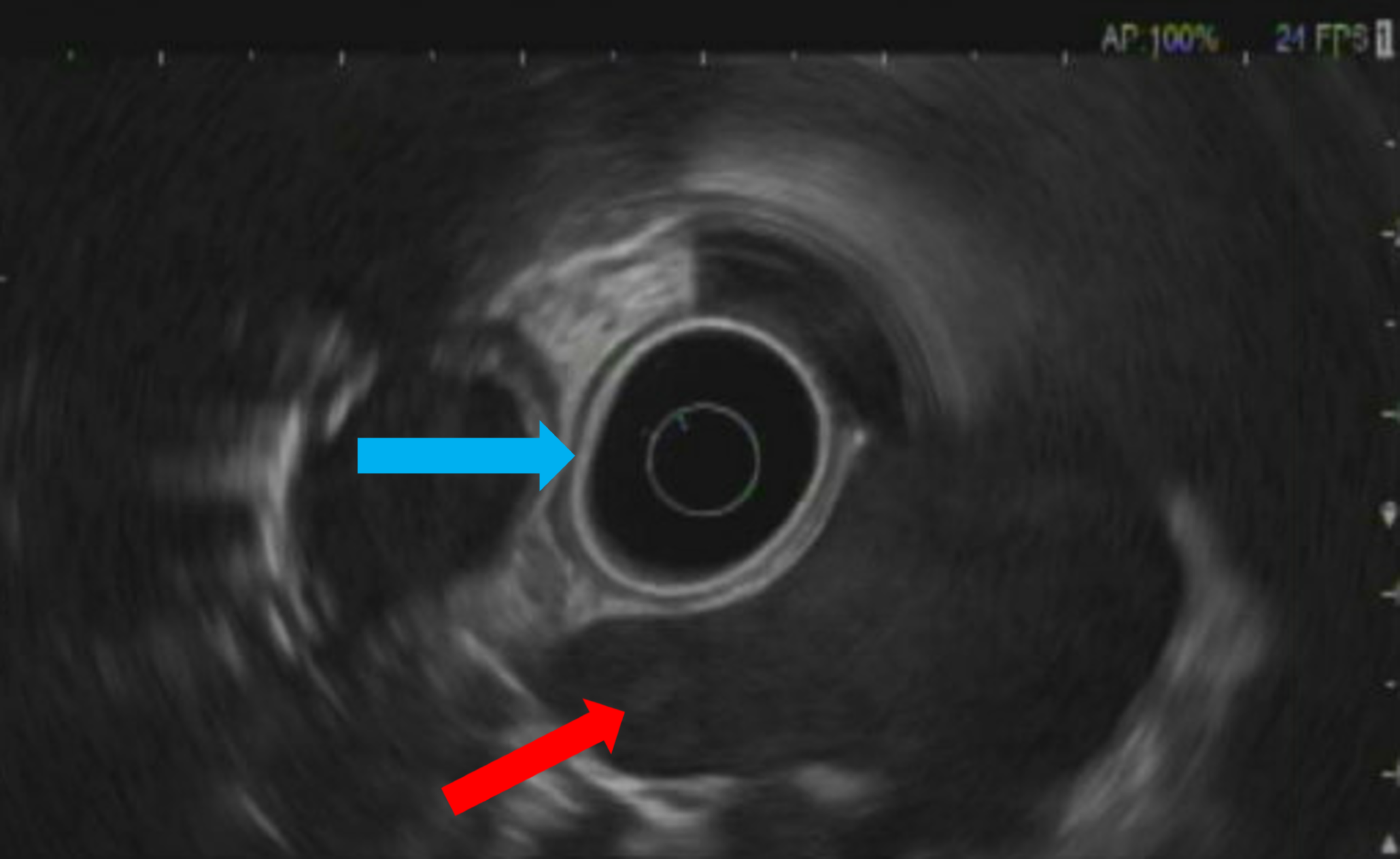
Figure: Figure 2: EUS showing aorta (red arrow) causing external compression of the esophagus (blue arrow).
Disclosures:
Rishi Bolla indicated no relevant financial relationships.
Ereny Demian indicated no relevant financial relationships.
Kevin Shah indicated no relevant financial relationships.
Rene Gomez-Esquivel indicated no relevant financial relationships.
John Jacobs: Medtronic – Advisory Committee/Board Member. Regeneron – Advisory Committee/Board Member, Speakers Bureau. Sanofi/Genzyme – Advisory Committee/Board Member, Speakers Bureau.
Samuel Slone indicated no relevant financial relationships.
Rishi Bolla, MD, Ereny Demian, MD, Kevin Shah, MD, Rene Gomez-Esquivel, MD, John Jacobs, MD, FACG, Samuel Slone, MD. P0724 - A Rare Case of Dysphagia Aortica Presenting as Pseudoachalasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of South Florida Morsani College of Medicine, Tampa, FL
Introduction: Dysphagia aortica is a condition characterized by esophageal obstruction due to extrinsic compression by the aorta. Its symptoms and imaging studies can mimic other causes of dysphagia, including achalasia. Here we present a case in which dysphagia aortica was diagnosed using endoscopic functional lumen imaging probe (FLIP) and endoscopic ultrasound (EUS).
Case Description/
Methods: An 82-year-old female with past medical history of kyphosis, prosthetic mitral valve, and diffuse atherosclerotic disease was referred to our institution for tertiary evaluation of chronic, progressive dysphagia with associated 60-pound weight loss. She had undergone esophagogastroduodenoscopy (EGD) previously which revealed dilated esophagus with food debris throughout, but no luminal obstruction.
Upon presentation, she underwent barium esophagram which showed a dilated esophagus concerning for achalasia. An EGD was performed which surprisingly revealed an area of external compression in the distal esophagus, just proximal to what was otherwise a widely patulous gastroesophageal junction (GEJ). Endoscopic FLIP was performed which showed normal distensibility index (DI) and minimum diameter of the GEJ. The area of suspected external compression showed DI 1.7mm2/mmHg and a minimum diameter of 11.6mm.
A computed tomography (CT) scan of the chest suggested esophageal compression by the aorta. Subsequent EUS revealed compression of the lower third of the esophagus by the aorta, confirming the diagnosis of dysphagia aortica. Given her age and poor functional status, the patient had a percutaneous gastrostomy tube placed for enteral nutrition pending evaluation for possible vascular intervention in future.
Discussion: There are few reported cases of dysphagia aortica in the literature, with some of the associated risk factors including older age, female sex, and history of kyphosis (1). Unlike in most cases of dysphagia aortica where patients have a clearly evident thoracic aortic aneurysm or tortuous aorta, our patient had an otherwise normal appearing aorta on CT imaging. (1, 2). Furthermore, she was symptomatic for nearly a year without a diagnosis resulting in severe protein-calorie malnutrition, which underscores the importance of recognizing this rare etiology of dysphagia.
References
1. Grimaldi S et al. Dysphagia aortica. Eur Surg. 2022;54(5):228-239.
2. Wilkinson JM et al. Diagnostic dilemmas in dysphagia aortica. European journal of cardio-thoracic surgery. 1997 Feb 1;11(2):222-7.
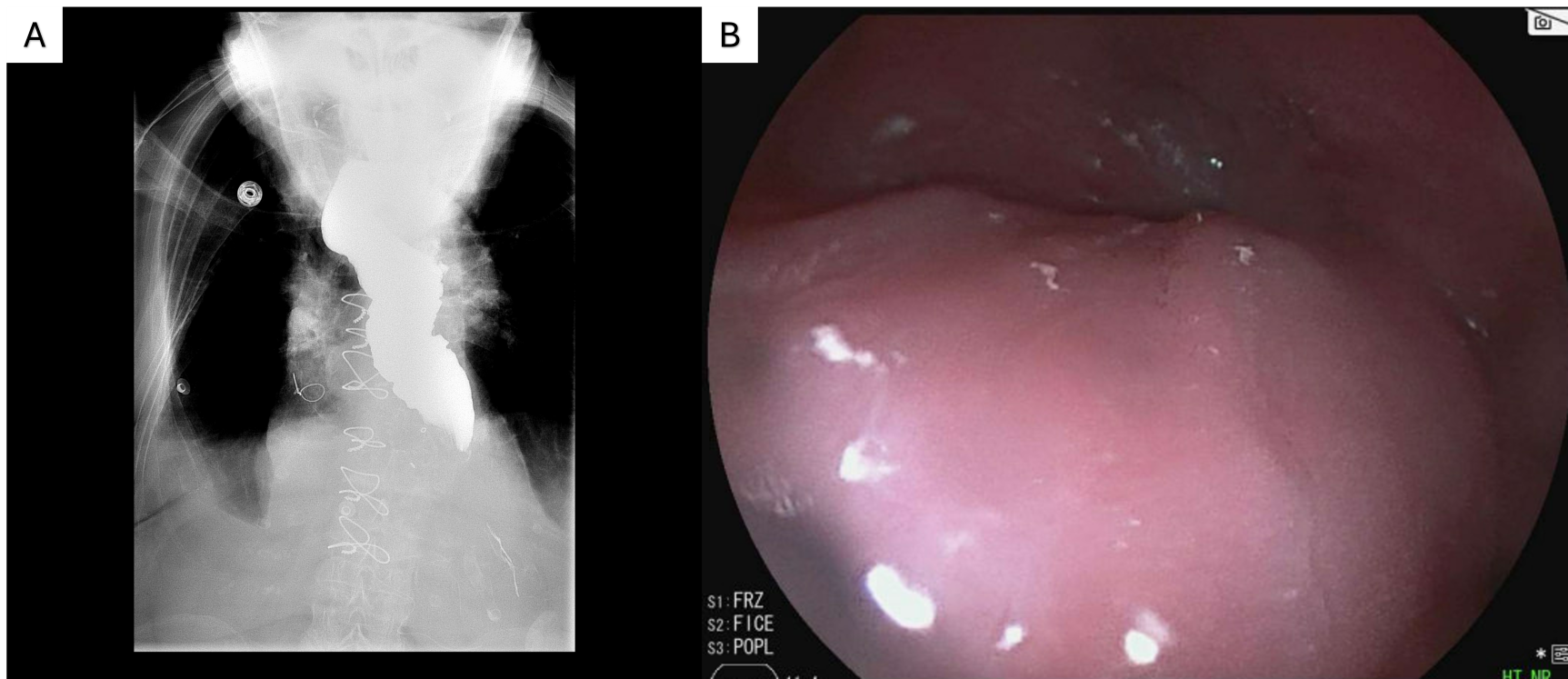
Figure: Figure 1: A) Barium esophagram showing dilated esophagus with delayed emptying, concerning for achalasia. B) EGD image of external compression of the distal esophagus.
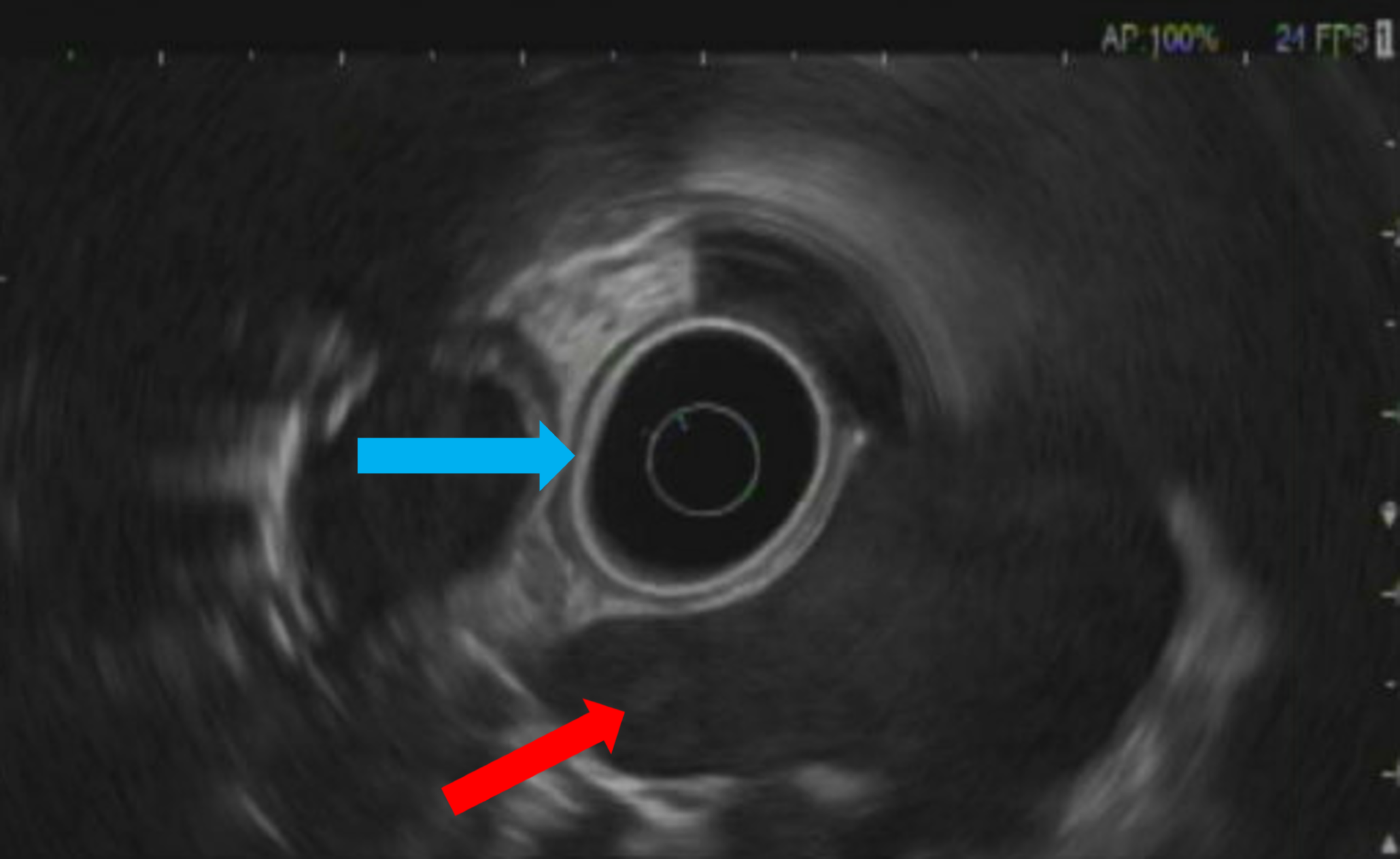
Figure: Figure 2: EUS showing aorta (red arrow) causing external compression of the esophagus (blue arrow).
Disclosures:
Rishi Bolla indicated no relevant financial relationships.
Ereny Demian indicated no relevant financial relationships.
Kevin Shah indicated no relevant financial relationships.
Rene Gomez-Esquivel indicated no relevant financial relationships.
John Jacobs: Medtronic – Advisory Committee/Board Member. Regeneron – Advisory Committee/Board Member, Speakers Bureau. Sanofi/Genzyme – Advisory Committee/Board Member, Speakers Bureau.
Samuel Slone indicated no relevant financial relationships.
Rishi Bolla, MD, Ereny Demian, MD, Kevin Shah, MD, Rene Gomez-Esquivel, MD, John Jacobs, MD, FACG, Samuel Slone, MD. P0724 - A Rare Case of Dysphagia Aortica Presenting as Pseudoachalasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
