Sunday Poster Session
Category: Esophagus
P0721 - The Importance of Performing Straight-Leg Testing in Post-Nissen Fundoplication Patients to Assess LES Integrity and Function
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Dharma Ayer, BS (she/her/hers)
Albany Medical Center
Albany, NY
Presenting Author(s)
Dharma Ayer, BS, Micheal Tadros, MD
Albany Medical Center, Albany, NY
Introduction: High-resolution manometry (HRM) is the standard diagnostic modality for characterizing esophageal motility and EGJ physiology. The Chicago Classification (CC) offers a systematic approach for interpreting HRM data. However, in patients with prior anti-reflux surgery such as Nissen fundoplication, anatomical alterations including wrap loosening, tightening, slipping or hernia recurrence may produce abnormal manometric findings. Straight leg testing has been studied to evaluate the integrity of the lower esophageal sphincter (LES). We present a case where straight leg testing was valuable in post-operative manometric evaluation.
Case Description/
Methods: A 57-year-old woman with a history of hiatal hernia repair four years ago presented with four months of worsening GERD symptoms including heartburn, regurgitation, and chronic cough. Upper endoscopy was performed which showed no gross mucosal lesions or visible hiatal hernia and confirmed previous Nissen fundoplication. Patient was referred for HRM testing which showed mildly elevated basal pressure. Residual pressure was slightly elevated at 16.9 (normal < 15), which is a finding expected post-fundoplication. Provocative maneuvers were performed, including straight leg testing to evaluate the integrity of the LES junction. This revealed a 2-3 cm separation between the LES and crural diaphragm, creating a double high-pressure zone consistent with a recurrent hiatal hernia.
Esophageal body function was preserved with a mean DCI of 3946 mmHg·s·cm. A barium swallow study confirmed a small type II paraesophageal hernia and marked spontaneous gastroesophageal reflux. The patient subsequently underwent robotic repair of the recurrent hiatal hernia with mesh placement and partial fundoplication, with resolution of her initial presenting symptoms.
Discussion: This case illustrates the diagnostic limitations of the CC in patients with altered post-surgical anatomy. In post-fundoplication patients, elevated residual pressure and findings suggestive of EGJOO diagnoses may not accurately reflect the underlying pathophysiology. The presence of a double high-pressure zone, indicated by separation of the LES and crural diaphragm, particularly on straight leg testing, may assist in diagnosing recurrent hiatal hernia.
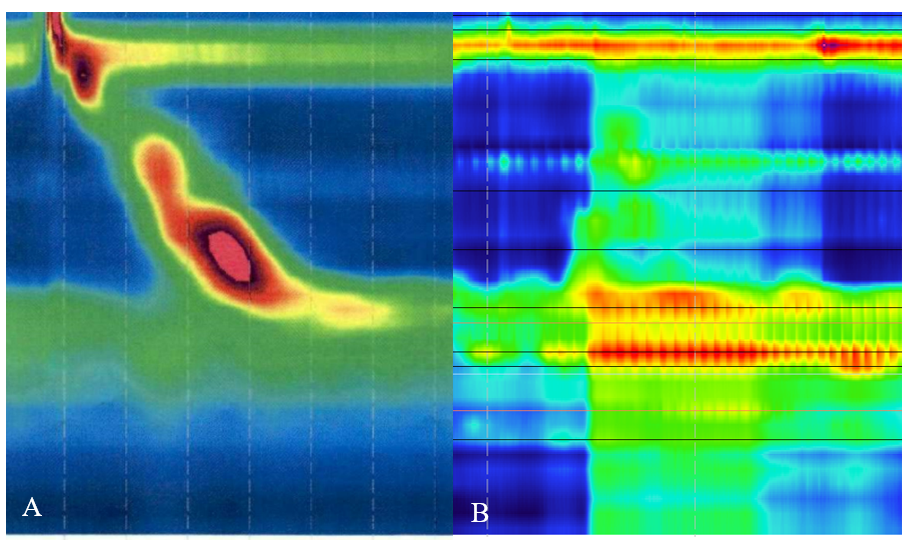
Figure: Figure 1: (A) High-resolution manometry (HRM) composite depicting baseline swallow. (B) HRM during straight leg testing showing a double high-pressure zone consistent with recurrent hiatal hernia.
Disclosures:
Dharma Ayer indicated no relevant financial relationships.
Micheal Tadros indicated no relevant financial relationships.
Dharma Ayer, BS, Micheal Tadros, MD. P0721 - The Importance of Performing Straight-Leg Testing in Post-Nissen Fundoplication Patients to Assess LES Integrity and Function, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Albany Medical Center, Albany, NY
Introduction: High-resolution manometry (HRM) is the standard diagnostic modality for characterizing esophageal motility and EGJ physiology. The Chicago Classification (CC) offers a systematic approach for interpreting HRM data. However, in patients with prior anti-reflux surgery such as Nissen fundoplication, anatomical alterations including wrap loosening, tightening, slipping or hernia recurrence may produce abnormal manometric findings. Straight leg testing has been studied to evaluate the integrity of the lower esophageal sphincter (LES). We present a case where straight leg testing was valuable in post-operative manometric evaluation.
Case Description/
Methods: A 57-year-old woman with a history of hiatal hernia repair four years ago presented with four months of worsening GERD symptoms including heartburn, regurgitation, and chronic cough. Upper endoscopy was performed which showed no gross mucosal lesions or visible hiatal hernia and confirmed previous Nissen fundoplication. Patient was referred for HRM testing which showed mildly elevated basal pressure. Residual pressure was slightly elevated at 16.9 (normal < 15), which is a finding expected post-fundoplication. Provocative maneuvers were performed, including straight leg testing to evaluate the integrity of the LES junction. This revealed a 2-3 cm separation between the LES and crural diaphragm, creating a double high-pressure zone consistent with a recurrent hiatal hernia.
Esophageal body function was preserved with a mean DCI of 3946 mmHg·s·cm. A barium swallow study confirmed a small type II paraesophageal hernia and marked spontaneous gastroesophageal reflux. The patient subsequently underwent robotic repair of the recurrent hiatal hernia with mesh placement and partial fundoplication, with resolution of her initial presenting symptoms.
Discussion: This case illustrates the diagnostic limitations of the CC in patients with altered post-surgical anatomy. In post-fundoplication patients, elevated residual pressure and findings suggestive of EGJOO diagnoses may not accurately reflect the underlying pathophysiology. The presence of a double high-pressure zone, indicated by separation of the LES and crural diaphragm, particularly on straight leg testing, may assist in diagnosing recurrent hiatal hernia.
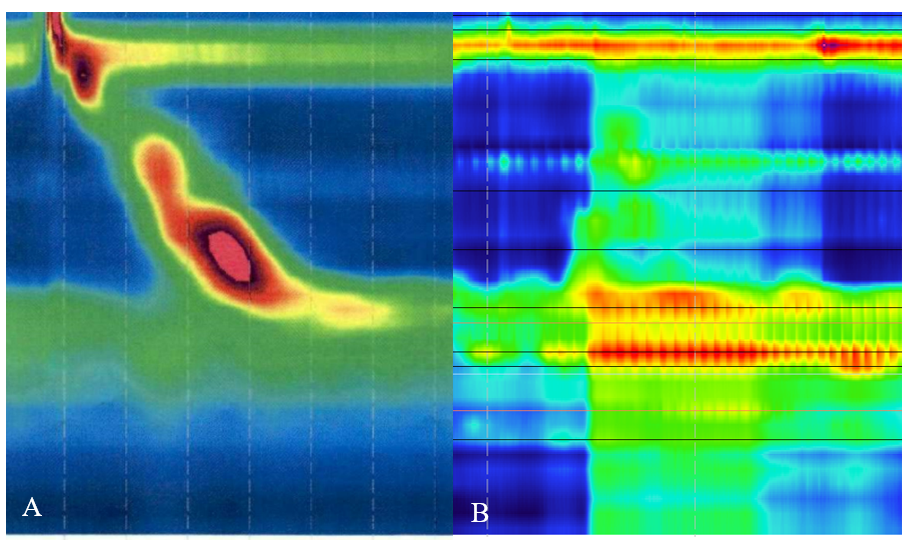
Figure: Figure 1: (A) High-resolution manometry (HRM) composite depicting baseline swallow. (B) HRM during straight leg testing showing a double high-pressure zone consistent with recurrent hiatal hernia.
Disclosures:
Dharma Ayer indicated no relevant financial relationships.
Micheal Tadros indicated no relevant financial relationships.
Dharma Ayer, BS, Micheal Tadros, MD. P0721 - The Importance of Performing Straight-Leg Testing in Post-Nissen Fundoplication Patients to Assess LES Integrity and Function, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
