Sunday Poster Session
Category: Esophagus
P0713 - When the Esophagus Turns on Itself: A Rare Case of Esophageal Intussusception
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Kazi Haque, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Kazi MD Tasnif. Haque, MD1, Jacob Reitnauer, 2, Nina Quirk, MD, MS3, Iyad Al-Bustami, MD, MPH4, Mariam Rizvi, MD2, George Ishac, MD2, Kevin Yu, MD4, Kumar Pallav, MD4
1University of Texas Health Science Center, Houston, TX; 2University of Texas at Houston, Houston, TX; 3University of Texas Health Sciences Center in Houston, Houston, TX; 4University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Though more common in children, esophageal intussusception (EI) is a rare condition in which the esophagus/stomach invaginates into itself, causing acute obstruction. Here, we discuss a case of EI in an adult, emphasizing its unique presentation and management.
Case Description/
Methods: A 54 y/o woman with metastatic distal esophageal cancer, and a recent G-tube placement one week prior to admission presents for vomiting, poor oral intake, and midsternal/epigastric pressure. CT Chest Imaging revealed a 2.8 cm portion of the distal esophagus (intussusceptum) seen telescoping into the proximal stomach (intussuscipiens), with the malignant tumor serving as the lead point at the apex of the invaginating segment (Figures A-B). The gastroenterology team performed an EGD which revealed no evidence of necrosis, ischemia, nor ongoing EI, suggesting that the issue had resolved (Figures C-D). This quick resolution shifted treatment focus to symptom management. Within the next few days, her symptoms resolved, and she was able to tolerate oral intake. Her improvement allowed for an appropriate discharge with a structured enteral feeding plan.
Discussion: Unlike small bowel or colonic intussusception where the bowels are not fixed to the peritoneum, the esophagus is fixed in the mediastinum, decreasing the likelihood for intussusception. While EI is not too well known, the proposed mechanism behind EI is strikingly similar to intussusception seen with a tumor/polypoid lesion serving as the lead point. Predisposing factors include anatomical alterations (cancer, hiatal hernia or prior esophageal surgery), increased intra-abdominal pressure, and poor fixation of the stomach. Presentations may include acute esophageal obstruction, respiratory distress, or upper gastrointestinal symptoms. Demonstrating an invaginated segment through imaging (esophagram, CT, or endoscopy) supports the diagnosis of EI. Treatment depends on symptom severity, with conservative management (observation and supportive care with naogastric decompression and IV fluids) attempted in select cases while endoscopic or surgical intervention is required when obstruction, perforation or ischemia exists. Fortunately, our patient had resolution of her intussusception quickly, thus her symptoms improved. Awareness of EI is essential for timely diagnosis and intervention. Early recognition and appropriate management help prevent complications and ensure the best possible prognosis.
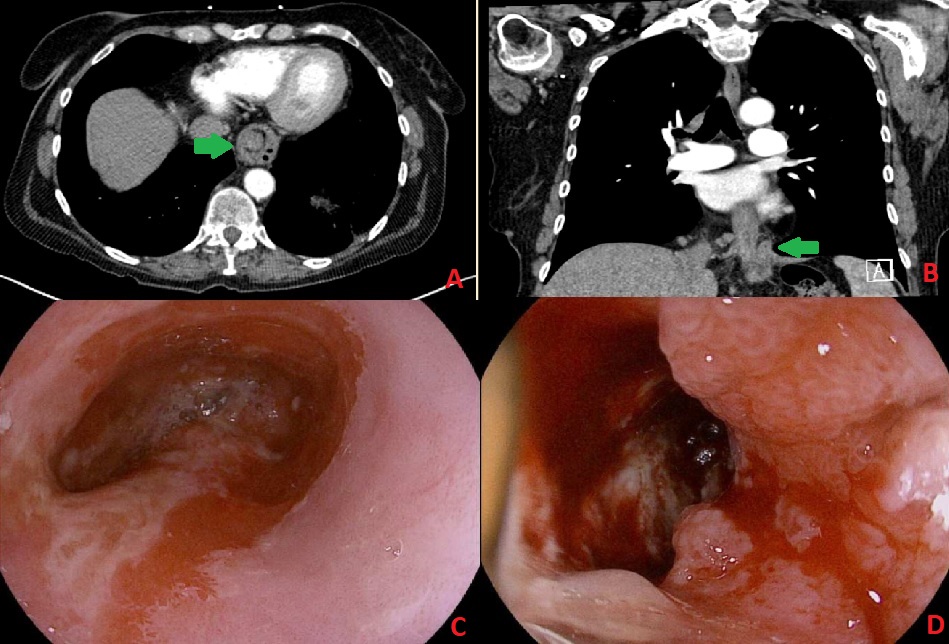
Figure: Figure 1 A-D:
a) Axial slice of CT Chest Scan depicting concentric rings and esophageal intussusception. Green Arrow points towards the intussusception.
b) Coronal slice of CT Chest Scan depicting 2.8 cm portion of distal esophagus intussuscepted into the stomach. Green Arrow points towards the intussusception.
c) Initial endoscopic apperance that corresponds to the intussuscepted portion seen on CT Scan.
d) Esophageal Mass that likely served as the lead point for the intussusception
Disclosures:
Kazi Haque indicated no relevant financial relationships.
Jacob Reitnauer indicated no relevant financial relationships.
Nina Quirk indicated no relevant financial relationships.
Iyad Al-Bustami indicated no relevant financial relationships.
Mariam Rizvi indicated no relevant financial relationships.
George Ishac indicated no relevant financial relationships.
Kevin Yu indicated no relevant financial relationships.
Kumar Pallav indicated no relevant financial relationships.
Kazi MD Tasnif. Haque, MD1, Jacob Reitnauer, 2, Nina Quirk, MD, MS3, Iyad Al-Bustami, MD, MPH4, Mariam Rizvi, MD2, George Ishac, MD2, Kevin Yu, MD4, Kumar Pallav, MD4. P0713 - When the Esophagus Turns on Itself: A Rare Case of Esophageal Intussusception, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Health Science Center, Houston, TX; 2University of Texas at Houston, Houston, TX; 3University of Texas Health Sciences Center in Houston, Houston, TX; 4University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Though more common in children, esophageal intussusception (EI) is a rare condition in which the esophagus/stomach invaginates into itself, causing acute obstruction. Here, we discuss a case of EI in an adult, emphasizing its unique presentation and management.
Case Description/
Methods: A 54 y/o woman with metastatic distal esophageal cancer, and a recent G-tube placement one week prior to admission presents for vomiting, poor oral intake, and midsternal/epigastric pressure. CT Chest Imaging revealed a 2.8 cm portion of the distal esophagus (intussusceptum) seen telescoping into the proximal stomach (intussuscipiens), with the malignant tumor serving as the lead point at the apex of the invaginating segment (Figures A-B). The gastroenterology team performed an EGD which revealed no evidence of necrosis, ischemia, nor ongoing EI, suggesting that the issue had resolved (Figures C-D). This quick resolution shifted treatment focus to symptom management. Within the next few days, her symptoms resolved, and she was able to tolerate oral intake. Her improvement allowed for an appropriate discharge with a structured enteral feeding plan.
Discussion: Unlike small bowel or colonic intussusception where the bowels are not fixed to the peritoneum, the esophagus is fixed in the mediastinum, decreasing the likelihood for intussusception. While EI is not too well known, the proposed mechanism behind EI is strikingly similar to intussusception seen with a tumor/polypoid lesion serving as the lead point. Predisposing factors include anatomical alterations (cancer, hiatal hernia or prior esophageal surgery), increased intra-abdominal pressure, and poor fixation of the stomach. Presentations may include acute esophageal obstruction, respiratory distress, or upper gastrointestinal symptoms. Demonstrating an invaginated segment through imaging (esophagram, CT, or endoscopy) supports the diagnosis of EI. Treatment depends on symptom severity, with conservative management (observation and supportive care with naogastric decompression and IV fluids) attempted in select cases while endoscopic or surgical intervention is required when obstruction, perforation or ischemia exists. Fortunately, our patient had resolution of her intussusception quickly, thus her symptoms improved. Awareness of EI is essential for timely diagnosis and intervention. Early recognition and appropriate management help prevent complications and ensure the best possible prognosis.
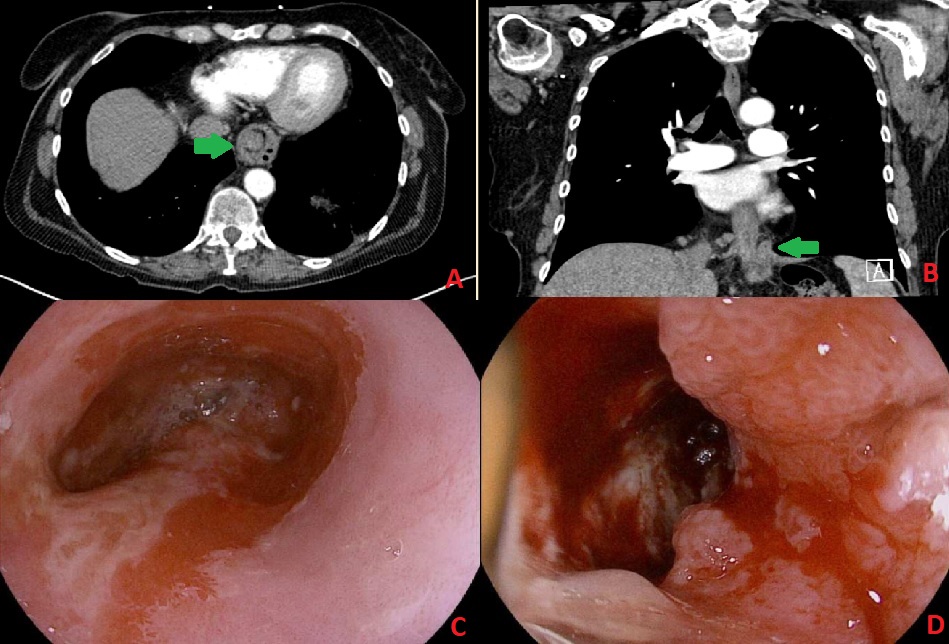
Figure: Figure 1 A-D:
a) Axial slice of CT Chest Scan depicting concentric rings and esophageal intussusception. Green Arrow points towards the intussusception.
b) Coronal slice of CT Chest Scan depicting 2.8 cm portion of distal esophagus intussuscepted into the stomach. Green Arrow points towards the intussusception.
c) Initial endoscopic apperance that corresponds to the intussuscepted portion seen on CT Scan.
d) Esophageal Mass that likely served as the lead point for the intussusception
Disclosures:
Kazi Haque indicated no relevant financial relationships.
Jacob Reitnauer indicated no relevant financial relationships.
Nina Quirk indicated no relevant financial relationships.
Iyad Al-Bustami indicated no relevant financial relationships.
Mariam Rizvi indicated no relevant financial relationships.
George Ishac indicated no relevant financial relationships.
Kevin Yu indicated no relevant financial relationships.
Kumar Pallav indicated no relevant financial relationships.
Kazi MD Tasnif. Haque, MD1, Jacob Reitnauer, 2, Nina Quirk, MD, MS3, Iyad Al-Bustami, MD, MPH4, Mariam Rizvi, MD2, George Ishac, MD2, Kevin Yu, MD4, Kumar Pallav, MD4. P0713 - When the Esophagus Turns on Itself: A Rare Case of Esophageal Intussusception, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

