Sunday Poster Session
Category: Esophagus
P0708 - Heart, Lungs, Stomach, and Colon With Stool in the Same CT Cut: An Interesting Picture
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Lauren Ferguson, BS
Wright State University Boonshoft School of Medicine
Eaton, OH
Presenting Author(s)
Lauren Ferguson, BS1, Ammar Ahmad, MD2, Rawan Aljaras, MD3, Drew Triplett, MD3
1Wright State University Boonshoft School of Medicine, Eaton, OH; 2Wright State University Boonshoft School of Medicine, Tipp City, OH; 3Wright State University Boonshoft School of Medicine, Dayton, OH
Introduction: Paraoesophageal hernias are a subtype of hiatal hernias and comprise about 5% of all hiatal hernias. Hiatal hernias are classified into four types (I to IV) based on anatomical variations, with types II, III, and IV categorized as paraoesophageal hernias. These hernias are characterized by herniation of the stomach and additional organs, such as the colon, into the thoracic cavity. Prevalence of hiatal hernias increases with age, likely resulting from age-related weakening of the diaphragm. Patients can present asymptomatically or report vague complaints such as heartburn, dysphagia, epigastric pain, nausea, vomiting, or chest pain.
Case Description/
Methods: Our patient is a 78-year-old male who presented with chest pain, nausea, and vomiting. Esophagogastroduodenoscopy (EGD) done 2 years prior to presentation showed a 6 cm large hiatal hernia with Cameron erosions. At the time, paraoesophageal hernia repair was delayed due to the patient’s history of MI and PEs. Repair was never completed. CT imaging done on admission and showed a large intrathoracic hiatal hernia with stool containing colon extending through the diaphragmatic defect (Figures A and B). EGD confirmed a large type IV hiatal hernia with sliding paraoesophageal component. The patient was referred to surgery outpatient for hernia repair.
Discussion: Delays in treatment for patients with paraoesophageal hiatal hernias can result in progression of a stable condition and serious complications in the future, necessitating higher risk intervention and negatively affecting patient outcomes. In our case, progressive worsening of the diaphragmatic defect led to herniation of the stomach and colon and has put the patient at an increased risk for complications.
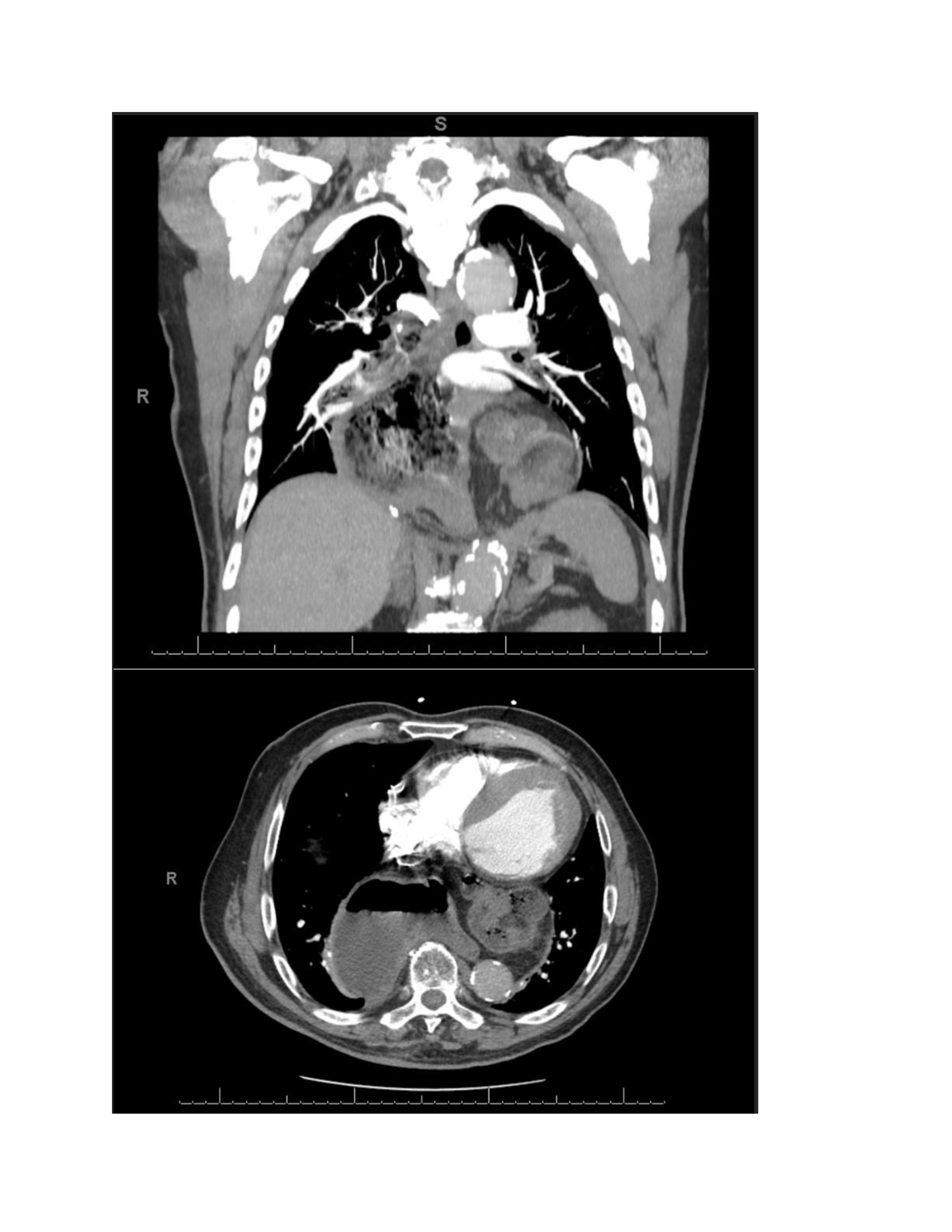
Figure: Figures A and B: CT imaging of the abdomen demonstrating a large intrathoracic hiatal hernia with herniation of the colon into the thoracic cavity
Disclosures:
Lauren Ferguson indicated no relevant financial relationships.
Ammar Ahmad indicated no relevant financial relationships.
Rawan Aljaras indicated no relevant financial relationships.
Drew Triplett indicated no relevant financial relationships.
Lauren Ferguson, BS1, Ammar Ahmad, MD2, Rawan Aljaras, MD3, Drew Triplett, MD3. P0708 - Heart, Lungs, Stomach, and Colon With Stool in the Same CT Cut: An Interesting Picture, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wright State University Boonshoft School of Medicine, Eaton, OH; 2Wright State University Boonshoft School of Medicine, Tipp City, OH; 3Wright State University Boonshoft School of Medicine, Dayton, OH
Introduction: Paraoesophageal hernias are a subtype of hiatal hernias and comprise about 5% of all hiatal hernias. Hiatal hernias are classified into four types (I to IV) based on anatomical variations, with types II, III, and IV categorized as paraoesophageal hernias. These hernias are characterized by herniation of the stomach and additional organs, such as the colon, into the thoracic cavity. Prevalence of hiatal hernias increases with age, likely resulting from age-related weakening of the diaphragm. Patients can present asymptomatically or report vague complaints such as heartburn, dysphagia, epigastric pain, nausea, vomiting, or chest pain.
Case Description/
Methods: Our patient is a 78-year-old male who presented with chest pain, nausea, and vomiting. Esophagogastroduodenoscopy (EGD) done 2 years prior to presentation showed a 6 cm large hiatal hernia with Cameron erosions. At the time, paraoesophageal hernia repair was delayed due to the patient’s history of MI and PEs. Repair was never completed. CT imaging done on admission and showed a large intrathoracic hiatal hernia with stool containing colon extending through the diaphragmatic defect (Figures A and B). EGD confirmed a large type IV hiatal hernia with sliding paraoesophageal component. The patient was referred to surgery outpatient for hernia repair.
Discussion: Delays in treatment for patients with paraoesophageal hiatal hernias can result in progression of a stable condition and serious complications in the future, necessitating higher risk intervention and negatively affecting patient outcomes. In our case, progressive worsening of the diaphragmatic defect led to herniation of the stomach and colon and has put the patient at an increased risk for complications.
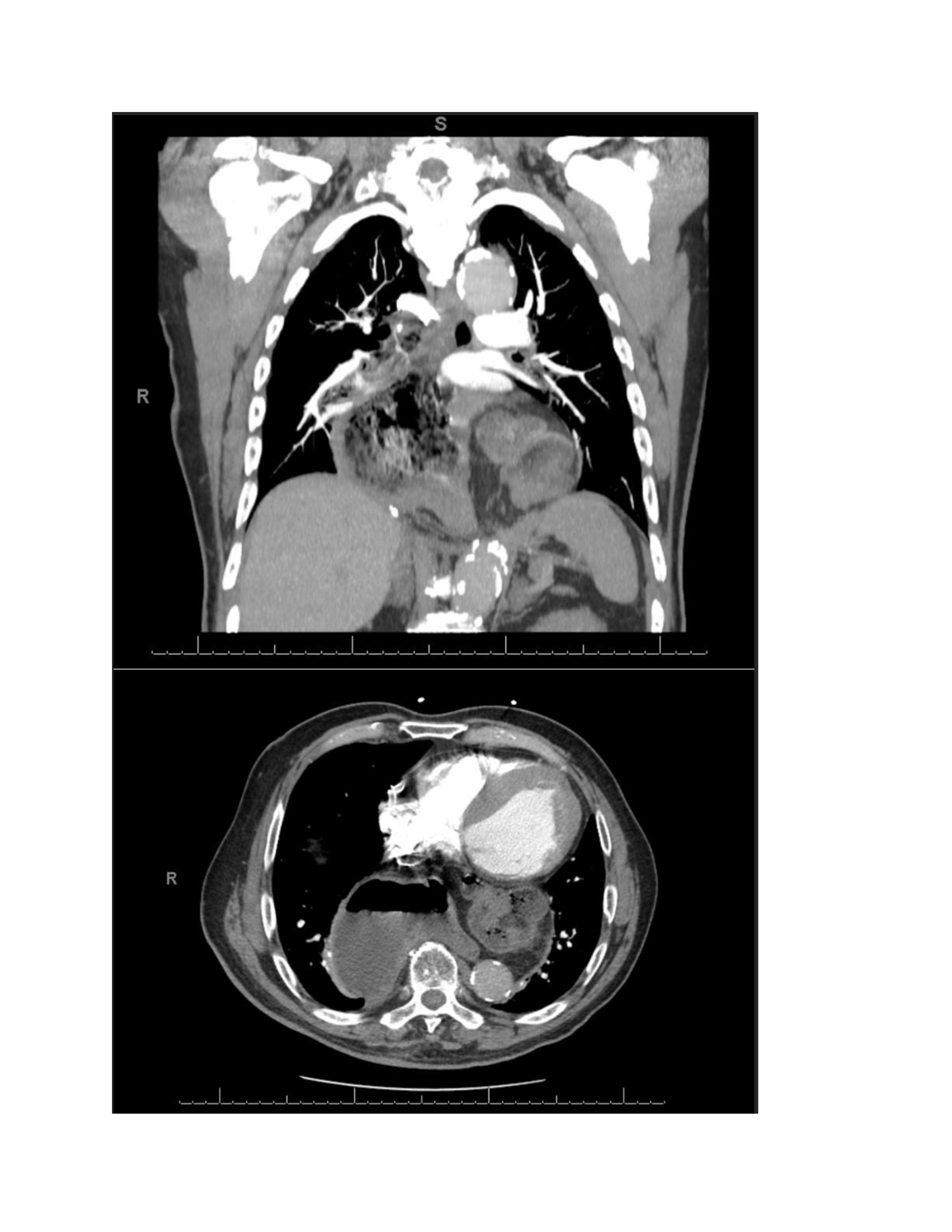
Figure: Figures A and B: CT imaging of the abdomen demonstrating a large intrathoracic hiatal hernia with herniation of the colon into the thoracic cavity
Disclosures:
Lauren Ferguson indicated no relevant financial relationships.
Ammar Ahmad indicated no relevant financial relationships.
Rawan Aljaras indicated no relevant financial relationships.
Drew Triplett indicated no relevant financial relationships.
Lauren Ferguson, BS1, Ammar Ahmad, MD2, Rawan Aljaras, MD3, Drew Triplett, MD3. P0708 - Heart, Lungs, Stomach, and Colon With Stool in the Same CT Cut: An Interesting Picture, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
