Sunday Poster Session
Category: Esophagus
P0706 - Acute Esophageal Necrosis: From Ischemia to Insight
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Daniel Stenberg, DO
University of Washington Medical Center
Seattle, WA
Presenting Author(s)
Daniel Stenberg, DO, Kaitlyn Carlson, MD, Gorav Kalra, MD
University of Washington Medical Center, Seattle, WA
Introduction: Acute esophageal necrosis, AEN, has an estimated prevalence of .01 to 0.28 and is characterized by diffuse, circumferential black-appearing esophageal mucosa. There are a handful of proposed etiologies that notably exclude toxic ingestion. AEN carries a mortality rate as high as 35% in some reports with up to 70% developing clinically significant upper GI bleeding.
This condition typically affects the distal esophagus, due to relative hypovascularity. Ischemia is proposed to be an inciting event. Literature suggests several associated causes including broad spectrum antibiotic use, infection, hyperglycemia, diabetic ketoacidosis (DKA) etc. In a manner akin to the Knudson two-hit hypothesis, there is often an inciting event which renders the mucosa vulnerable to severe topical injury.
Case Description/
Methods: A 49-year-old male with a history of diabetes presented to the hospital after several days of worsening emesis evolved into hematemesis. Initial blood glucose was 1,272. He was tachycardic and labs were concerning for acidosis at 7.15 on venous blood gas. He was treated in critical care with insulin and fluids. As he improved, the dysphonia, dysphagia and odynophagia persisted, thus prompting an EGD, which showed circumferential necrosis extending from the upper esophagus to the GE junction (Fig. 1). He was made NPO while cross sectional imaging was obtained and showed esophageal thickening and edema (Fig. 2). Otolaryngology evaluated his persistent dysphonia and noted ulcerative lesions with edema, though fully mobile vocal folds. The patient was fluid resuscitated and on total peripheral nutrition until a negative swallow study where after he started a clear liquid diet. He subsequently recovered and discharged home.
Discussion: Hyperglycemia, particularly in the setting of DKA, may lead to AEN via a reduced blood volume state due to osmotic diuresis. The diuresis results in a state of hypoperfusion and impaired gastric motility exacerbates reflux; the two hits. Management can be varied but volume expansion and gastric acid suppression may help avoid further damage to esophageal mucosa. Oral intake should be strictly avoided for at least 24 hours. There is a risk for significant hemorrhage, so nasogastric tubes are not recommended and treatment with submucosal epinephrine is occasionally warranted. Many cases are resolved with supportive care.
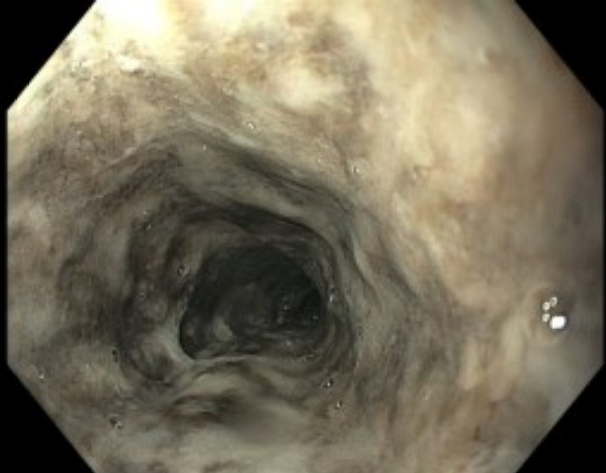
Figure: Circumferential necrosis from upper esophagus to gastroesophageal junction.
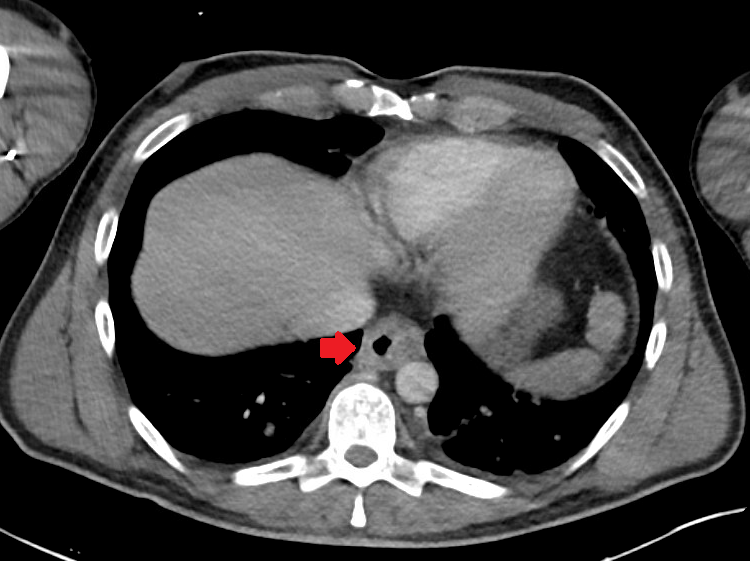
Figure: Esophageal thickening and edema
Disclosures:
Daniel Stenberg indicated no relevant financial relationships.
Kaitlyn Carlson indicated no relevant financial relationships.
Gorav Kalra indicated no relevant financial relationships.
Daniel Stenberg, DO, Kaitlyn Carlson, MD, Gorav Kalra, MD. P0706 - Acute Esophageal Necrosis: From Ischemia to Insight, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Washington Medical Center, Seattle, WA
Introduction: Acute esophageal necrosis, AEN, has an estimated prevalence of .01 to 0.28 and is characterized by diffuse, circumferential black-appearing esophageal mucosa. There are a handful of proposed etiologies that notably exclude toxic ingestion. AEN carries a mortality rate as high as 35% in some reports with up to 70% developing clinically significant upper GI bleeding.
This condition typically affects the distal esophagus, due to relative hypovascularity. Ischemia is proposed to be an inciting event. Literature suggests several associated causes including broad spectrum antibiotic use, infection, hyperglycemia, diabetic ketoacidosis (DKA) etc. In a manner akin to the Knudson two-hit hypothesis, there is often an inciting event which renders the mucosa vulnerable to severe topical injury.
Case Description/
Methods: A 49-year-old male with a history of diabetes presented to the hospital after several days of worsening emesis evolved into hematemesis. Initial blood glucose was 1,272. He was tachycardic and labs were concerning for acidosis at 7.15 on venous blood gas. He was treated in critical care with insulin and fluids. As he improved, the dysphonia, dysphagia and odynophagia persisted, thus prompting an EGD, which showed circumferential necrosis extending from the upper esophagus to the GE junction (Fig. 1). He was made NPO while cross sectional imaging was obtained and showed esophageal thickening and edema (Fig. 2). Otolaryngology evaluated his persistent dysphonia and noted ulcerative lesions with edema, though fully mobile vocal folds. The patient was fluid resuscitated and on total peripheral nutrition until a negative swallow study where after he started a clear liquid diet. He subsequently recovered and discharged home.
Discussion: Hyperglycemia, particularly in the setting of DKA, may lead to AEN via a reduced blood volume state due to osmotic diuresis. The diuresis results in a state of hypoperfusion and impaired gastric motility exacerbates reflux; the two hits. Management can be varied but volume expansion and gastric acid suppression may help avoid further damage to esophageal mucosa. Oral intake should be strictly avoided for at least 24 hours. There is a risk for significant hemorrhage, so nasogastric tubes are not recommended and treatment with submucosal epinephrine is occasionally warranted. Many cases are resolved with supportive care.
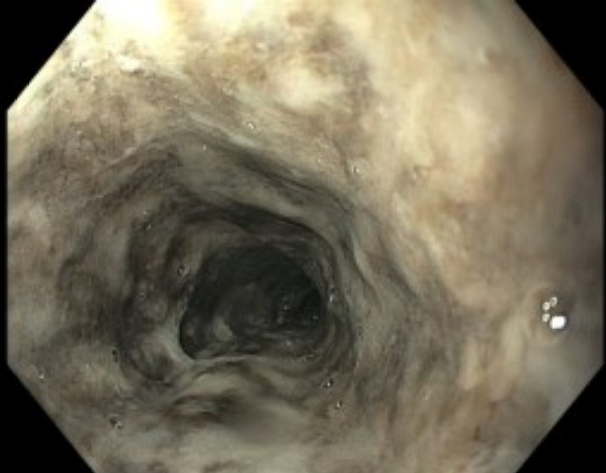
Figure: Circumferential necrosis from upper esophagus to gastroesophageal junction.
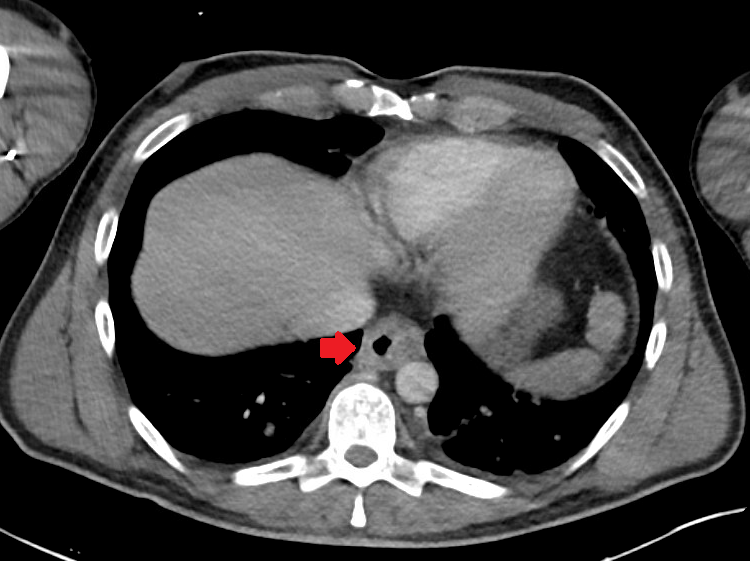
Figure: Esophageal thickening and edema
Disclosures:
Daniel Stenberg indicated no relevant financial relationships.
Kaitlyn Carlson indicated no relevant financial relationships.
Gorav Kalra indicated no relevant financial relationships.
Daniel Stenberg, DO, Kaitlyn Carlson, MD, Gorav Kalra, MD. P0706 - Acute Esophageal Necrosis: From Ischemia to Insight, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
