Sunday Poster Session
Category: Esophagus
P0683 - Acute Esophageal Necrosis in Critical Illness: A Case Series on Pathophysiology, Endoscopic Findings, and Outcomes
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Abel Sanchez, MD, MSc (he/him/his)
Hospital Roosevelt / Gastri-k
Guatemala City, San Marcos, Guatemala
Presenting Author(s)
Jorge Pacheco, 1, Ninoska Meléndez, 1, Kenia Santos, 2, Abel Sanchez, MD, MSc3
11. Gastroenterology and Endoscopy Unit, Hospital Roosevelt Guatemala, Guatemala City, Quetzaltenango, Guatemala; 2Gastroenterogy Unit, Hospital Roosevelt, Guatemala City, Chimaltenango, Guatemala; 3Hospital Roosevelt / Gastri-k, Guatemala City, San Marcos, Guatemala
Introduction: Acute esophageal necrosis (AEN), commonly termed "black esophagus," is a rare but severe gastrointestinal condition characterized by diffuse esophageal mucosal ischemia, often precipitated by shock states, metabolic disorders, and systemic infections. The pathophysiology involves hypoperfusion, mucosal barrier dysfunction, and oxidative stress, leading to necrosis and ulceration. Gastrointestinal bleeding is a frequent complication. This case series highlights patients presenting with AEN in distinct clinical settings
Case Description/
Methods: Case 1: A 70-year-old male with heart failure, pneumonia, and acute-on-chronic kidney disease developed staphylococcus aureus catheter-associated bacteremia, resulting in septic shock. During hospitalization, he presented with coffee-ground emesis and melena. EGD revealed blackish mucosa extending from 22 cm to 36 cm from the dental arch, with grayish and erythematous regions, suggestive of ischemic necrosis. Treatment with proton pump inhibitor (PPI) infusion, vasopressors, and antibiotics led to clinical improvement. The patient recovered and was discharged
Case 2: A 67-year-old female with type 2 diabetes mellitus, acute myocardial infarction, and cardiogenic shock was admitted with dyspnea, chest pain, and fluid overload. During hospitalization, she developed melena and acute anemia, prompting EGD, which revealed necrosis, fibrosis, erosions, and mucosal bleeding from the middle to distal esophageal third, consistent with AEN. Conservative management was pursued.
Case 3: A 62-year-old female in intensive care with septic shock secondary to hospital-acquired pneumonia and moderate acute respiratory distress syndrome (ARDS) was mechanically ventilated and remained refractory to vasoactive amines. During hospitalization, she developed hematemesis, prompting EGD, which revealed ulcerations covered in fibrin, extensive mucosal discoloration affecting 75% of the esophageal circumference. These findings confirmed AEN
Discussion: AEN is an underrecognized clinical entity with high morbidity, often linked to circulatory shock and metabolic derangements. Early endoscopic assessment plays a critical role in diagnosis, guiding therapeutic decisions and prognosis. While PPIs and supportive care remain the mainstay of treatment, follow-up endoscopy may be warranted in severe cases to monitor resolution. This case series highlights the importance of recognizing AEN in critically ill patients, emphasizing its multifactorial nature and the role of timely intervention
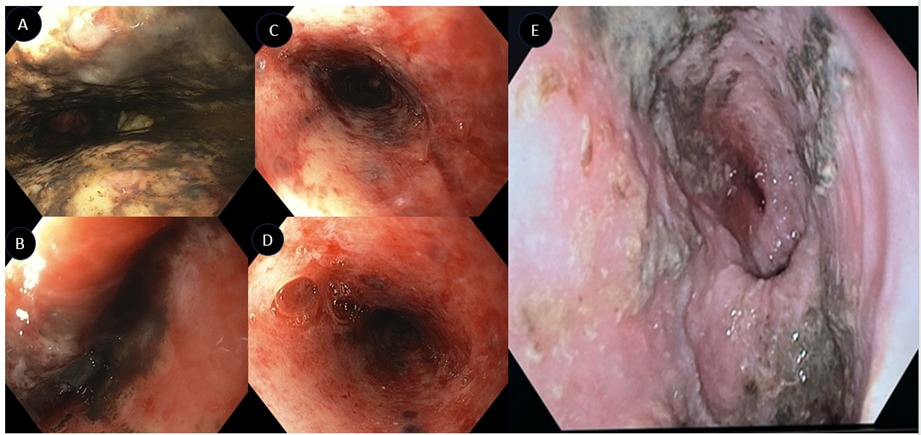
Figure: Figure 1. A, B: Circumferential black discoloration of the esophageal mucosa, affecting the distal third of the esophagus; C, D: friable mucosa with ulcerations, bleeding and sloughing, indicating severe ischemic injury, with visible necrotic areas throughout the esophagus. E: edema, fibrin and necrotic areas of the distal esophageal mucosa
Disclosures:
Jorge Pacheco indicated no relevant financial relationships.
Ninoska Meléndez indicated no relevant financial relationships.
Kenia Santos indicated no relevant financial relationships.
Abel Sanchez indicated no relevant financial relationships.
Jorge Pacheco, 1, Ninoska Meléndez, 1, Kenia Santos, 2, Abel Sanchez, MD, MSc3. P0683 - Acute Esophageal Necrosis in Critical Illness: A Case Series on Pathophysiology, Endoscopic Findings, and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
11. Gastroenterology and Endoscopy Unit, Hospital Roosevelt Guatemala, Guatemala City, Quetzaltenango, Guatemala; 2Gastroenterogy Unit, Hospital Roosevelt, Guatemala City, Chimaltenango, Guatemala; 3Hospital Roosevelt / Gastri-k, Guatemala City, San Marcos, Guatemala
Introduction: Acute esophageal necrosis (AEN), commonly termed "black esophagus," is a rare but severe gastrointestinal condition characterized by diffuse esophageal mucosal ischemia, often precipitated by shock states, metabolic disorders, and systemic infections. The pathophysiology involves hypoperfusion, mucosal barrier dysfunction, and oxidative stress, leading to necrosis and ulceration. Gastrointestinal bleeding is a frequent complication. This case series highlights patients presenting with AEN in distinct clinical settings
Case Description/
Methods: Case 1: A 70-year-old male with heart failure, pneumonia, and acute-on-chronic kidney disease developed staphylococcus aureus catheter-associated bacteremia, resulting in septic shock. During hospitalization, he presented with coffee-ground emesis and melena. EGD revealed blackish mucosa extending from 22 cm to 36 cm from the dental arch, with grayish and erythematous regions, suggestive of ischemic necrosis. Treatment with proton pump inhibitor (PPI) infusion, vasopressors, and antibiotics led to clinical improvement. The patient recovered and was discharged
Case 2: A 67-year-old female with type 2 diabetes mellitus, acute myocardial infarction, and cardiogenic shock was admitted with dyspnea, chest pain, and fluid overload. During hospitalization, she developed melena and acute anemia, prompting EGD, which revealed necrosis, fibrosis, erosions, and mucosal bleeding from the middle to distal esophageal third, consistent with AEN. Conservative management was pursued.
Case 3: A 62-year-old female in intensive care with septic shock secondary to hospital-acquired pneumonia and moderate acute respiratory distress syndrome (ARDS) was mechanically ventilated and remained refractory to vasoactive amines. During hospitalization, she developed hematemesis, prompting EGD, which revealed ulcerations covered in fibrin, extensive mucosal discoloration affecting 75% of the esophageal circumference. These findings confirmed AEN
Discussion: AEN is an underrecognized clinical entity with high morbidity, often linked to circulatory shock and metabolic derangements. Early endoscopic assessment plays a critical role in diagnosis, guiding therapeutic decisions and prognosis. While PPIs and supportive care remain the mainstay of treatment, follow-up endoscopy may be warranted in severe cases to monitor resolution. This case series highlights the importance of recognizing AEN in critically ill patients, emphasizing its multifactorial nature and the role of timely intervention
Figure: Figure 1. A, B: Circumferential black discoloration of the esophageal mucosa, affecting the distal third of the esophagus; C, D: friable mucosa with ulcerations, bleeding and sloughing, indicating severe ischemic injury, with visible necrotic areas throughout the esophagus. E: edema, fibrin and necrotic areas of the distal esophageal mucosa
Disclosures:
Jorge Pacheco indicated no relevant financial relationships.
Ninoska Meléndez indicated no relevant financial relationships.
Kenia Santos indicated no relevant financial relationships.
Abel Sanchez indicated no relevant financial relationships.
Jorge Pacheco, 1, Ninoska Meléndez, 1, Kenia Santos, 2, Abel Sanchez, MD, MSc3. P0683 - Acute Esophageal Necrosis in Critical Illness: A Case Series on Pathophysiology, Endoscopic Findings, and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
