Sunday Poster Session
Category: Esophagus
P0668 - Racial Disparities in Hospitalization Outcomes Among Patients With Eosinophilic Esophagitis in the United States
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ritik Goyal, MBBS
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Ritik M. Goyal, MBBS1, Bhavik Bansal, MBBS2, Sameer Rao, MBBS1, Kranthi Mandava, MD1, Narinderjeet Kaur, MD, MS3, Muhammad Hassaan Arif Maan, MBBS1, Menna-Allah Elaskandrany, DO4, Ahmed Al-Khazraji, MD1
1Rutgers New Jersey Medical School, Newark, NJ; 2University of Texas Southwestern Medical Center, Dallas, TX; 3SUNY Downstate Health Sciences University, Brooklyn, NY; 4Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: Eosinophilic esophagitis (EoE) is a chronic, allergen-mediated, inflammatory condition of the esophagus with increasing prevalence. It typically manifests as feeding difficulties and abdominal pain in children, and as dysphagia or food impaction in adults. If left untreated, EoE may lead to complications such as strictures, fibrosis, perforation, and food impaction. Current treatment guidelines recommend esophageal dilation for fibrostenotic disease. This study aims to examine racial disparities in healthcare utilization and clinical outcomes among hospitalized patients with EoE.
Methods: We performed a retrospective analysis using the National Inpatient Sample (NIS) 2016-2022. Hospitalized patients with EoE were identified using relevant ICD-10 codes. Weighted logistic regression was used for clinical outcomes, including the use of esophageal dilation, sepsis, pneumonia, malnutrition, vitamin deficiency, esophageal perforation, ulcers, and strictures. Weighted linear regression was performed for length of stay (LOS) and total hospital charges. All analyses incorporated survey weights to produce nationally representative estimates and adjusted for age, sex, comorbidities, and insurance status. Statistical significance was defined as p< 0.05.
Results: A total of 2,767 patients were identified, representing 13,835 weighted hospitalizations with a median age of 22 years (IQR: 12-43). Among them, 10,190 (73.6%) were White, 1,545 (11.2%) Black, 1,240 (9.0%) Hispanic, and 860 (6.2%) of other races. The LOS was significantly higher in non-White patients compared to White patients (β = 0.51; 95% CI: 0.03–0.98; p=0.038). Similarly, total hospital charges were greater in non-Whites (β = $7,098; 95% CI: $3,110–$10,927; p < 0.001). Non-White patients were also less likely to undergo esophageal dilation (OR = 0.57; 95% CI: 0.35–0.94; p = 0.029). There were no significant differences in rates of EoE-related complications, including in-hospital sepsis, pneumonia, malnutrition, vitamin deficiency, or esophageal perforation, ulcers, and strictures.
Discussion: Our findings highlight significant racial disparities in the management and healthcare utilization of patients hospitalized with eosinophilic esophagitis. Despite these differences in care delivery, complication rates remained similar across racial groups. These results underscore the need for targeted interventions to address potential inequities in the diagnosis and management of EoE and promote more equitable healthcare practices.
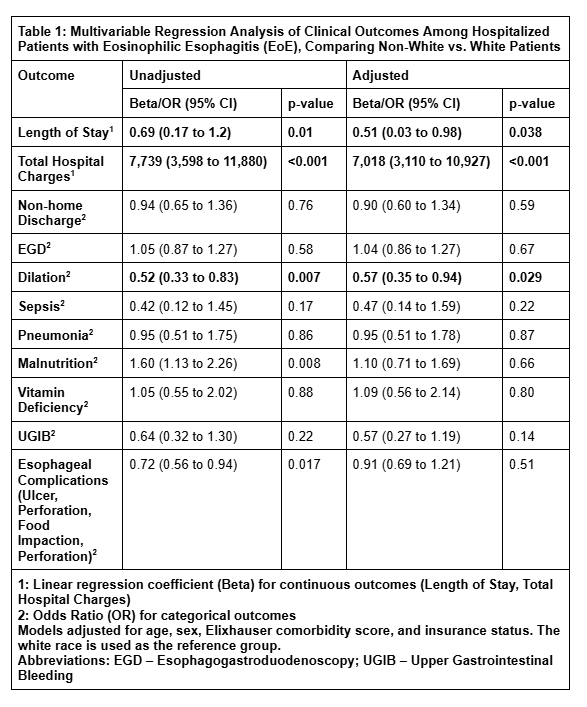
Figure: Table 1: Multivariable Regression Analysis of Clinical Outcomes Among Hospitalized Patients with Eosinophilic Esophagitis (EoE), Comparing Non-White vs. White Patients
Disclosures:
Ritik M. Goyal indicated no relevant financial relationships.
Bhavik Bansal indicated no relevant financial relationships.
Sameer Rao indicated no relevant financial relationships.
Kranthi Mandava indicated no relevant financial relationships.
Narinderjeet Kaur indicated no relevant financial relationships.
Muhammad Hassaan Arif Maan indicated no relevant financial relationships.
Menna-Allah Elaskandrany indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Ritik M. Goyal, MBBS1, Bhavik Bansal, MBBS2, Sameer Rao, MBBS1, Kranthi Mandava, MD1, Narinderjeet Kaur, MD, MS3, Muhammad Hassaan Arif Maan, MBBS1, Menna-Allah Elaskandrany, DO4, Ahmed Al-Khazraji, MD1. P0668 - Racial Disparities in Hospitalization Outcomes Among Patients With Eosinophilic Esophagitis in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2University of Texas Southwestern Medical Center, Dallas, TX; 3SUNY Downstate Health Sciences University, Brooklyn, NY; 4Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: Eosinophilic esophagitis (EoE) is a chronic, allergen-mediated, inflammatory condition of the esophagus with increasing prevalence. It typically manifests as feeding difficulties and abdominal pain in children, and as dysphagia or food impaction in adults. If left untreated, EoE may lead to complications such as strictures, fibrosis, perforation, and food impaction. Current treatment guidelines recommend esophageal dilation for fibrostenotic disease. This study aims to examine racial disparities in healthcare utilization and clinical outcomes among hospitalized patients with EoE.
Methods: We performed a retrospective analysis using the National Inpatient Sample (NIS) 2016-2022. Hospitalized patients with EoE were identified using relevant ICD-10 codes. Weighted logistic regression was used for clinical outcomes, including the use of esophageal dilation, sepsis, pneumonia, malnutrition, vitamin deficiency, esophageal perforation, ulcers, and strictures. Weighted linear regression was performed for length of stay (LOS) and total hospital charges. All analyses incorporated survey weights to produce nationally representative estimates and adjusted for age, sex, comorbidities, and insurance status. Statistical significance was defined as p< 0.05.
Results: A total of 2,767 patients were identified, representing 13,835 weighted hospitalizations with a median age of 22 years (IQR: 12-43). Among them, 10,190 (73.6%) were White, 1,545 (11.2%) Black, 1,240 (9.0%) Hispanic, and 860 (6.2%) of other races. The LOS was significantly higher in non-White patients compared to White patients (β = 0.51; 95% CI: 0.03–0.98; p=0.038). Similarly, total hospital charges were greater in non-Whites (β = $7,098; 95% CI: $3,110–$10,927; p < 0.001). Non-White patients were also less likely to undergo esophageal dilation (OR = 0.57; 95% CI: 0.35–0.94; p = 0.029). There were no significant differences in rates of EoE-related complications, including in-hospital sepsis, pneumonia, malnutrition, vitamin deficiency, or esophageal perforation, ulcers, and strictures.
Discussion: Our findings highlight significant racial disparities in the management and healthcare utilization of patients hospitalized with eosinophilic esophagitis. Despite these differences in care delivery, complication rates remained similar across racial groups. These results underscore the need for targeted interventions to address potential inequities in the diagnosis and management of EoE and promote more equitable healthcare practices.
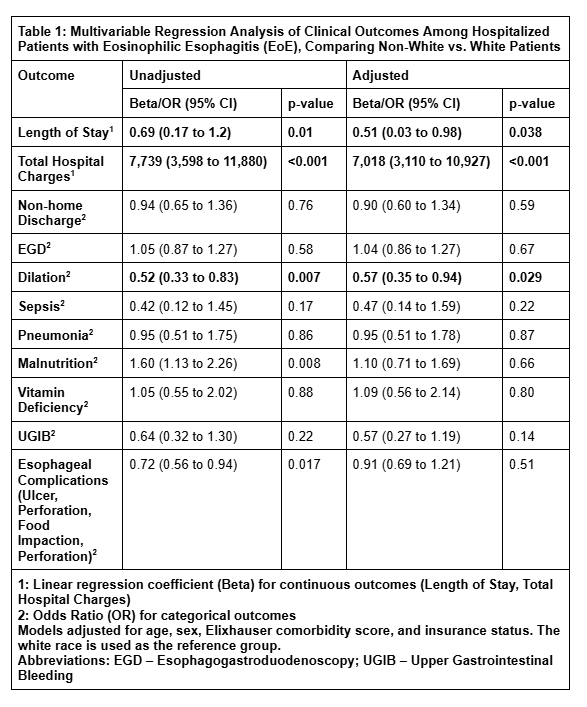
Figure: Table 1: Multivariable Regression Analysis of Clinical Outcomes Among Hospitalized Patients with Eosinophilic Esophagitis (EoE), Comparing Non-White vs. White Patients
Disclosures:
Ritik M. Goyal indicated no relevant financial relationships.
Bhavik Bansal indicated no relevant financial relationships.
Sameer Rao indicated no relevant financial relationships.
Kranthi Mandava indicated no relevant financial relationships.
Narinderjeet Kaur indicated no relevant financial relationships.
Muhammad Hassaan Arif Maan indicated no relevant financial relationships.
Menna-Allah Elaskandrany indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Ritik M. Goyal, MBBS1, Bhavik Bansal, MBBS2, Sameer Rao, MBBS1, Kranthi Mandava, MD1, Narinderjeet Kaur, MD, MS3, Muhammad Hassaan Arif Maan, MBBS1, Menna-Allah Elaskandrany, DO4, Ahmed Al-Khazraji, MD1. P0668 - Racial Disparities in Hospitalization Outcomes Among Patients With Eosinophilic Esophagitis in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
