Sunday Poster Session
Category: Esophagus
P0665 - Language Disparities in the Completion of Esophageal Testing for Dysphagia
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Jennifer Dimino, MD (she/her/hers)
Center for Neurointestinal Health, Massachusetts General Hospital
Miami, FL
Presenting Author(s)
Jennifer Dimino, MD1, Christopher Velez, MD2, Nir Bar, MD2, Braden Kuo, MD2
1Center for Neurointestinal Health, Massachusetts General Hospital, Miami, FL; 2Center for Neurointestinal Health, Massachusetts General Hospital, Boston, MA
Introduction: Dysphagia work up should invariably include an endoscopy. Patients with dysphagia often experience incomplete or delayed diagnostic evaluations. We hypothesized that testing completion and time to evaluation would vary by English or non-English language.
Methods: A research database from a large university hospital network including tertiary and community hospitals was used to obtain data from adult patients (age>18) who had a diagnosis of dysphagia in 2022 and the associated care pathways and workup through 2024. Patient demographics and diagnostic testing obtained through 2024 were analyzed retrospectively using deidentified data. We compared English and non-English speaking patients for test completion rates and average time to diagnostic tests.
Results: Among 3,897 patients with dysphagia and language data, 50.3% (1961) underwent upper endoscopy, while only 21.3% (405) had barium esophagram, 6.5% (176) underwent esophageal manometry, 4.3% (146) had pH testing, and 3.2% (67) underwent endoFLIP. Upper endoscopy completion was lower for non-English patients in comparison to English speaking patients (40.2% vs 51.1%, p< 0.001). Esophagram and esophageal manometry completion were similar (13.9% vs 10.1%, p >0.05 and 4.5% vs 5.3%, p >0.05, respectively). The average time to testing was not significantly different between groups with the exception of pH testing which showed a shorter wait for non-English patients when compared to English patients (40.8 days vs 94.7 days, p< 0.04).
Discussion: Our findings show that only half of patients with documented dysphagia underwent endoscopy to rule out structural disease. Moreover, language-based disparities exist where non-English speaking patients are less likely to undergo an upper endoscopy. Interestingly, English-speaking patients may experience greater delays in advanced esophageal testing such as pH testing, which may be impacted by referral bias and symptom severity. These discrepancies highlight the need to examine factors contributing to access and timing of care. Potential solutions may include navigation programs, increased access to specialized testing, and policy-level changes to reduce institutional barriers.
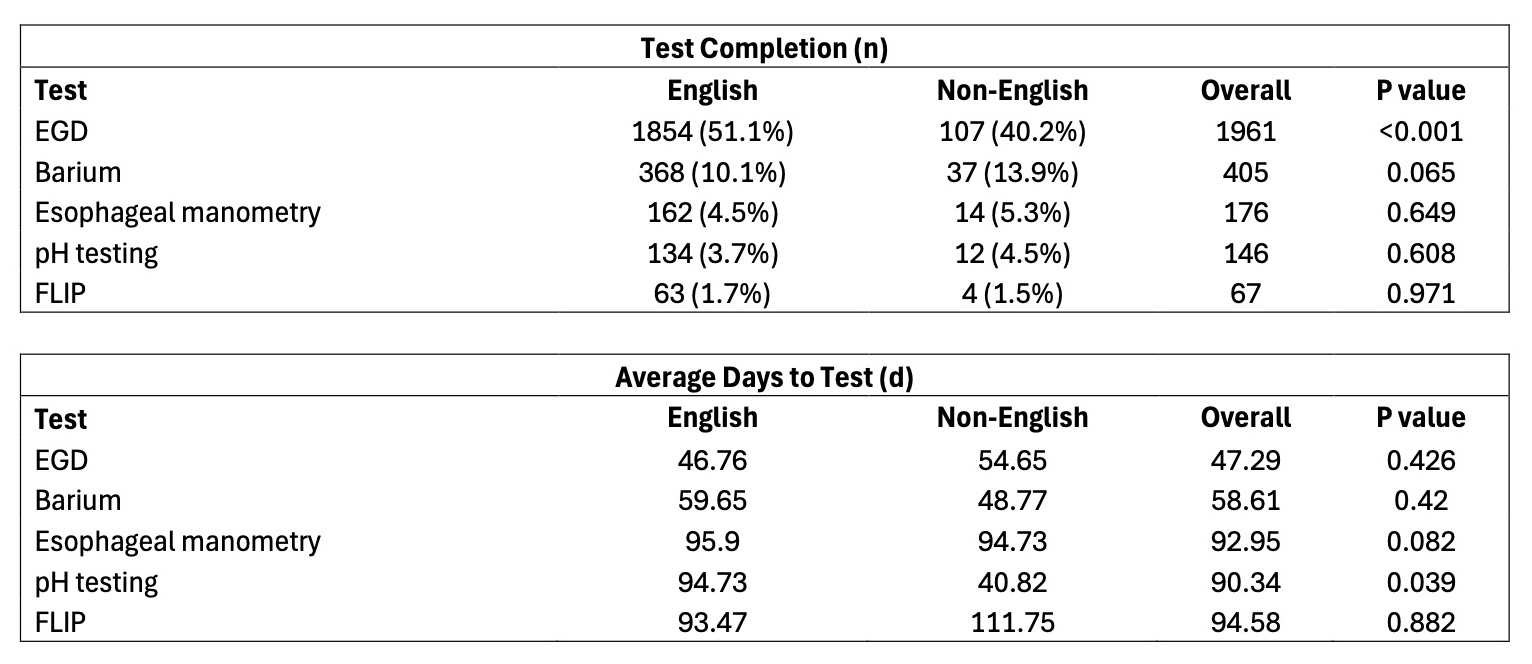
Figure: Patient Demographics
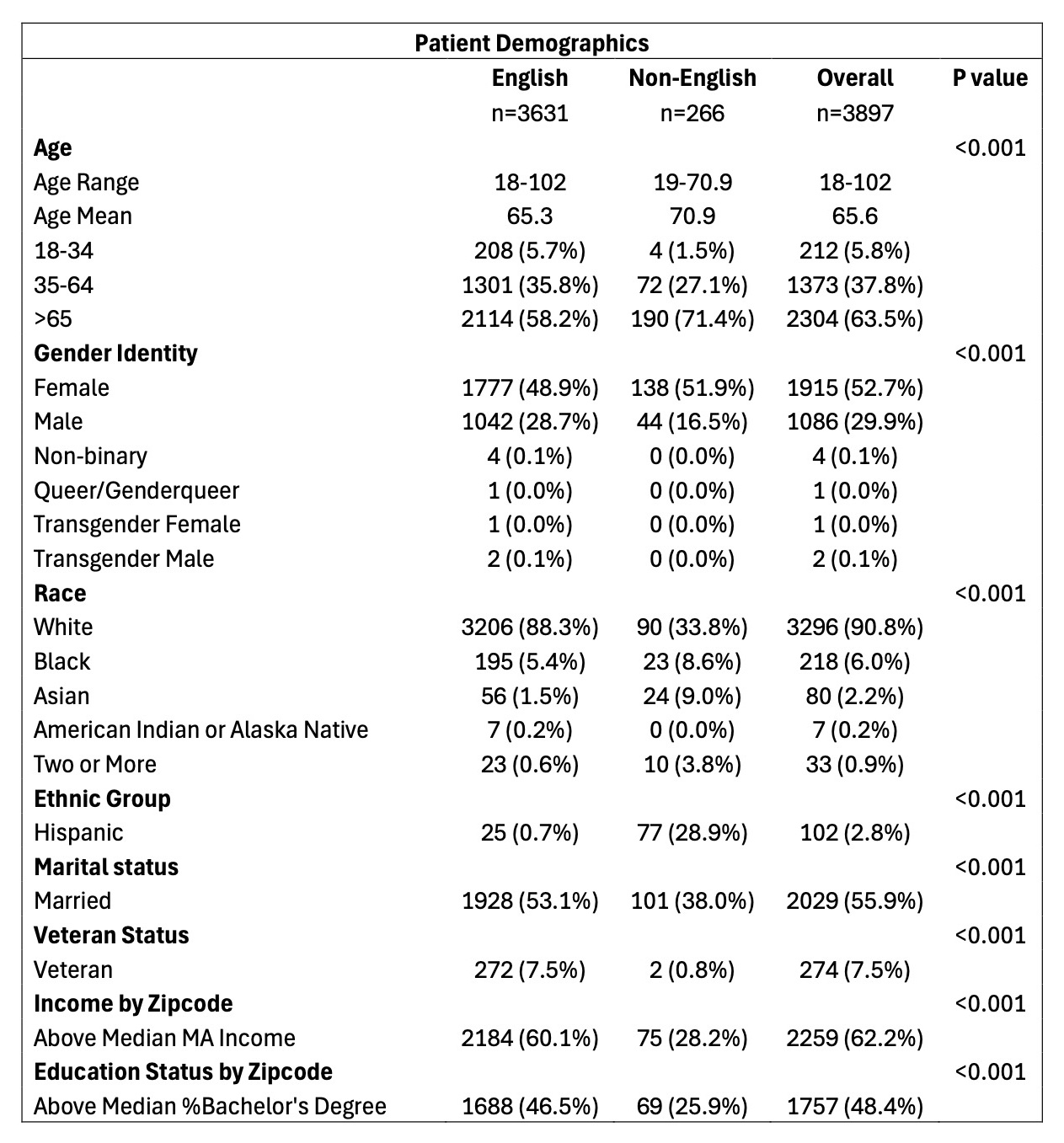
Figure: Test Completion and Average Days to Test
Disclosures:
Jennifer Dimino indicated no relevant financial relationships.
Christopher Velez indicated no relevant financial relationships.
Nir Bar indicated no relevant financial relationships.
Braden Kuo: Atmo – Consultant. Cindome – Consultant. ClinRx Pharma – Consultant. Evoke – Consultant. Genzynme – Consultant. GI Foundation – Consultant. Ironwood – Consultant. Medtronic – Consultant. Neurogastrx – Consultant. Novo – Consultant. Phathom – Consultant. Takeda – Consultant.
Jennifer Dimino, MD1, Christopher Velez, MD2, Nir Bar, MD2, Braden Kuo, MD2. P0665 - Language Disparities in the Completion of Esophageal Testing for Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Center for Neurointestinal Health, Massachusetts General Hospital, Miami, FL; 2Center for Neurointestinal Health, Massachusetts General Hospital, Boston, MA
Introduction: Dysphagia work up should invariably include an endoscopy. Patients with dysphagia often experience incomplete or delayed diagnostic evaluations. We hypothesized that testing completion and time to evaluation would vary by English or non-English language.
Methods: A research database from a large university hospital network including tertiary and community hospitals was used to obtain data from adult patients (age>18) who had a diagnosis of dysphagia in 2022 and the associated care pathways and workup through 2024. Patient demographics and diagnostic testing obtained through 2024 were analyzed retrospectively using deidentified data. We compared English and non-English speaking patients for test completion rates and average time to diagnostic tests.
Results: Among 3,897 patients with dysphagia and language data, 50.3% (1961) underwent upper endoscopy, while only 21.3% (405) had barium esophagram, 6.5% (176) underwent esophageal manometry, 4.3% (146) had pH testing, and 3.2% (67) underwent endoFLIP. Upper endoscopy completion was lower for non-English patients in comparison to English speaking patients (40.2% vs 51.1%, p< 0.001). Esophagram and esophageal manometry completion were similar (13.9% vs 10.1%, p >0.05 and 4.5% vs 5.3%, p >0.05, respectively). The average time to testing was not significantly different between groups with the exception of pH testing which showed a shorter wait for non-English patients when compared to English patients (40.8 days vs 94.7 days, p< 0.04).
Discussion: Our findings show that only half of patients with documented dysphagia underwent endoscopy to rule out structural disease. Moreover, language-based disparities exist where non-English speaking patients are less likely to undergo an upper endoscopy. Interestingly, English-speaking patients may experience greater delays in advanced esophageal testing such as pH testing, which may be impacted by referral bias and symptom severity. These discrepancies highlight the need to examine factors contributing to access and timing of care. Potential solutions may include navigation programs, increased access to specialized testing, and policy-level changes to reduce institutional barriers.
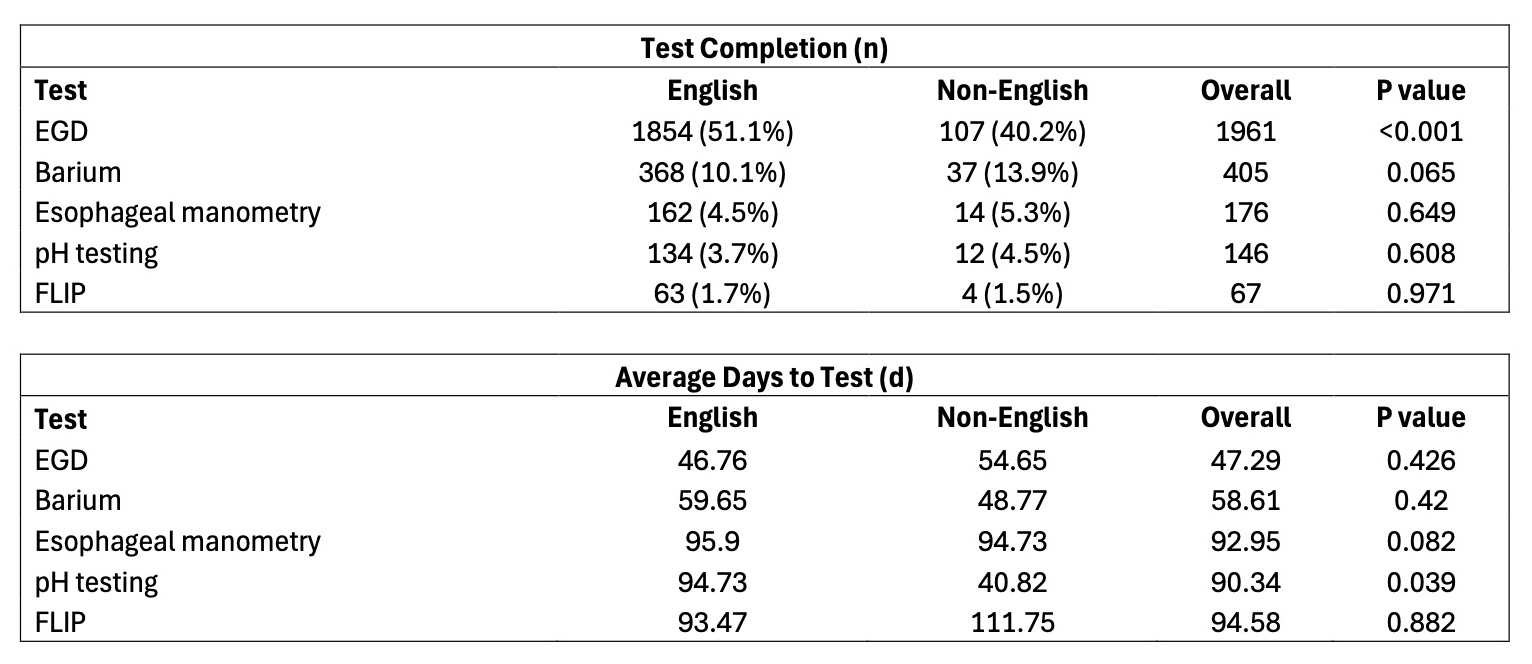
Figure: Patient Demographics
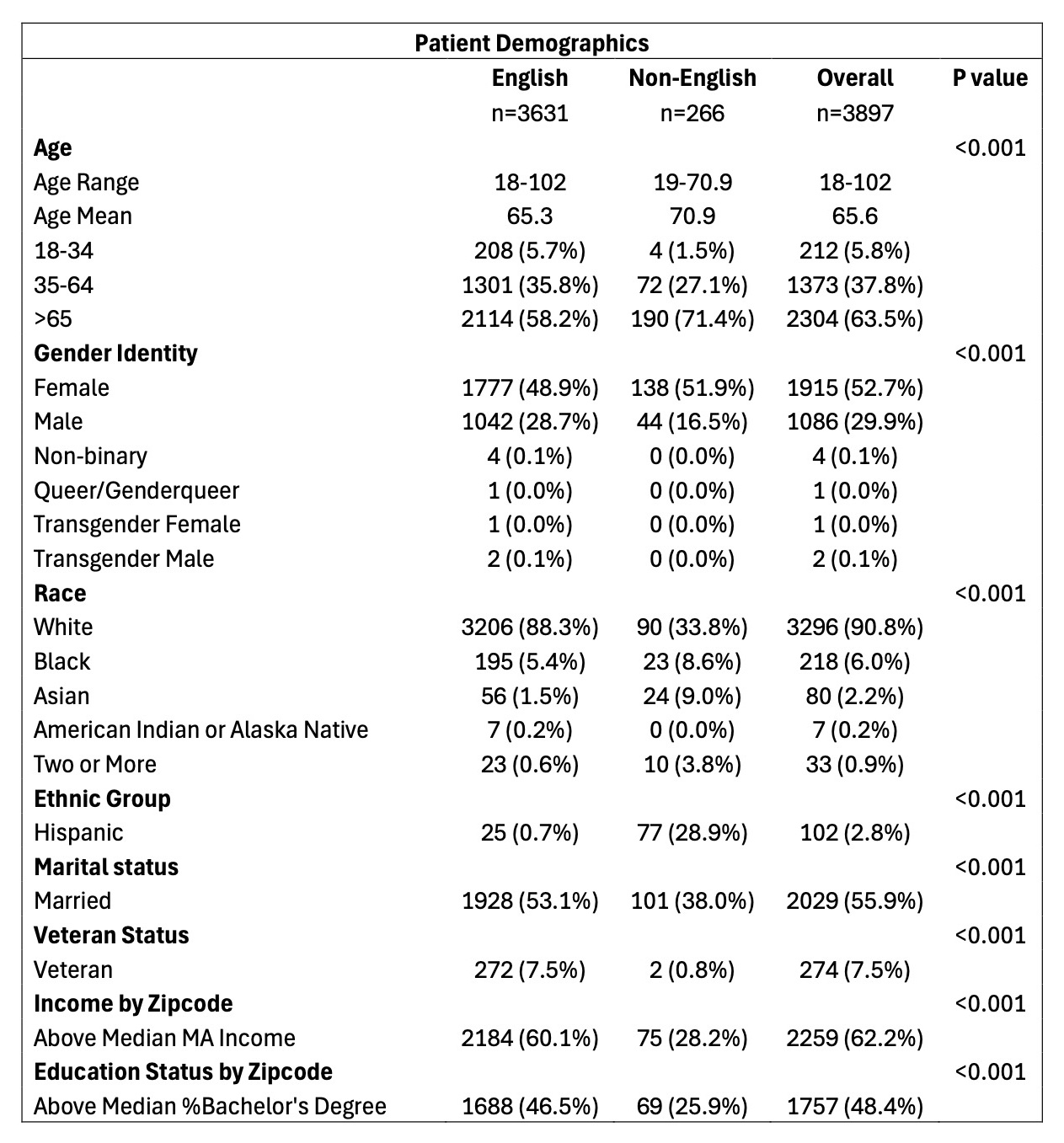
Figure: Test Completion and Average Days to Test
Disclosures:
Jennifer Dimino indicated no relevant financial relationships.
Christopher Velez indicated no relevant financial relationships.
Nir Bar indicated no relevant financial relationships.
Braden Kuo: Atmo – Consultant. Cindome – Consultant. ClinRx Pharma – Consultant. Evoke – Consultant. Genzynme – Consultant. GI Foundation – Consultant. Ironwood – Consultant. Medtronic – Consultant. Neurogastrx – Consultant. Novo – Consultant. Phathom – Consultant. Takeda – Consultant.
Jennifer Dimino, MD1, Christopher Velez, MD2, Nir Bar, MD2, Braden Kuo, MD2. P0665 - Language Disparities in the Completion of Esophageal Testing for Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

