Sunday Poster Session
Category: Esophagus
P0662 - Geographic and Risk Factor Disparities in Stomach and Esophageal Cancer Burden Across the US: Findings From GBD 2021
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rithish Nimmagadda, MBBS (he/him/his)
One Brooklyn Health-Interfaith Medical Center
Brooklyn, NY
Presenting Author(s)
Rithish Nimmagadda, MBBS1, Sameer Majety, MBBS2, Nayanika Tummala, MD3, Naga Praneeth Vakkalagadda, MD4, Pragathi Munnangi, MD5, Hemanth Kamadi, MBBS6, Swathi Cherukuri, MBBS7, Krishna Sai Kiran Sakalabaktula, MBBS8
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2School of Medicine, Xiamen University., Kakinada, Andhra Pradesh, India; 3St. Mary's General Hospital, New York Medical College, Poughkeepsie, NY; 4University of Alabama at Birmingham Heersink School of Medicine, Montgomery, AL; 5BronxCare Health System, New York City, NY; 6School of Medicine, Xiamen University, China, Kakinada, Andhra Pradesh, India; 7Narayana Medical College, Nellore, Andhra Pradesh, India; 8Government General Hospital Kakinada, Kakinada, Andhra Pradesh, India
Introduction: Stomach and esophageal cancers remain significant contributors to cancer burden in the U.S., but their epidemiologic contours differ. This study uses GBD 2021 data to compare incidence, prevalence, and risk factor-attributable DALYs for these malignancies across states and age groups.
Methods: We used age-standardized incidence and prevalence rates to assess interstate variation. Gross case numbers were analyzed across age groups to identify high-burden subpopulations. For risk factor (RF) analysis, age-standardized DALY rates attributable to specific RFs were used.
Results: Stomach cancer incidence showed considerable geographic variation, with the Pacific and Southern States (Hawaii: 7.88, Louisiana: 6.70, Mississippi: 6.05) having the highest rates, and Mountain/Northern States (Idaho: 3.82, Vermont: 3.96, Utah: 4.03) the lowest. Prevalence patterns closely mirrored incidence. The highest DALYs and prevalence occurred in the 65–74 age group for both sexes, though peak incidence was at 65–74 in males and 85+ in females.
Esophageal cancer showed a different pattern. Incidence was highest in the District of Columbia (5.73), Maine (5.64), and West Virginia (5.35), and lowest in Utah (3.16), California (3.17), and Hawaii (3.50). Males aged 65–74 bore the heaviest burden with 6,635 incident cases and 131,288 DALYs. For females, the highest incidence and DALYs were also seen at 65–74, while deaths peaked at 75–84.
Risk factor analysis uncovered distinct etiologies. Stomach cancer was primarily driven by habitual exposures such as smoking (DALY 13.09 in Mississippi) and high-sodium diets (8.24 in Hawaii). Esophageal cancer was linked to smoking (63.29 in West Virginia), alcohol use (30.03 in D.C.), low vegetable intake, and chewing tobacco—particularly in Appalachian and Northeastern states.
Discussion: Stomach cancer shows a coastal-southern pattern with dietary and tobacco RFs; esophageal cancer clusters in Appalachia/Northeast with multifactorial lifestyle drivers. The 65–74 age group consistently bears the heaviest load. Preventive strategies should include targeted smoking cessation in Appalachia, salt-reduction campaigns in the South, alcohol moderation in high-use states, and national initiatives to boost vegetable intake. State-level interventions must align with regional RF patterns to reduce this dual cancer burden.
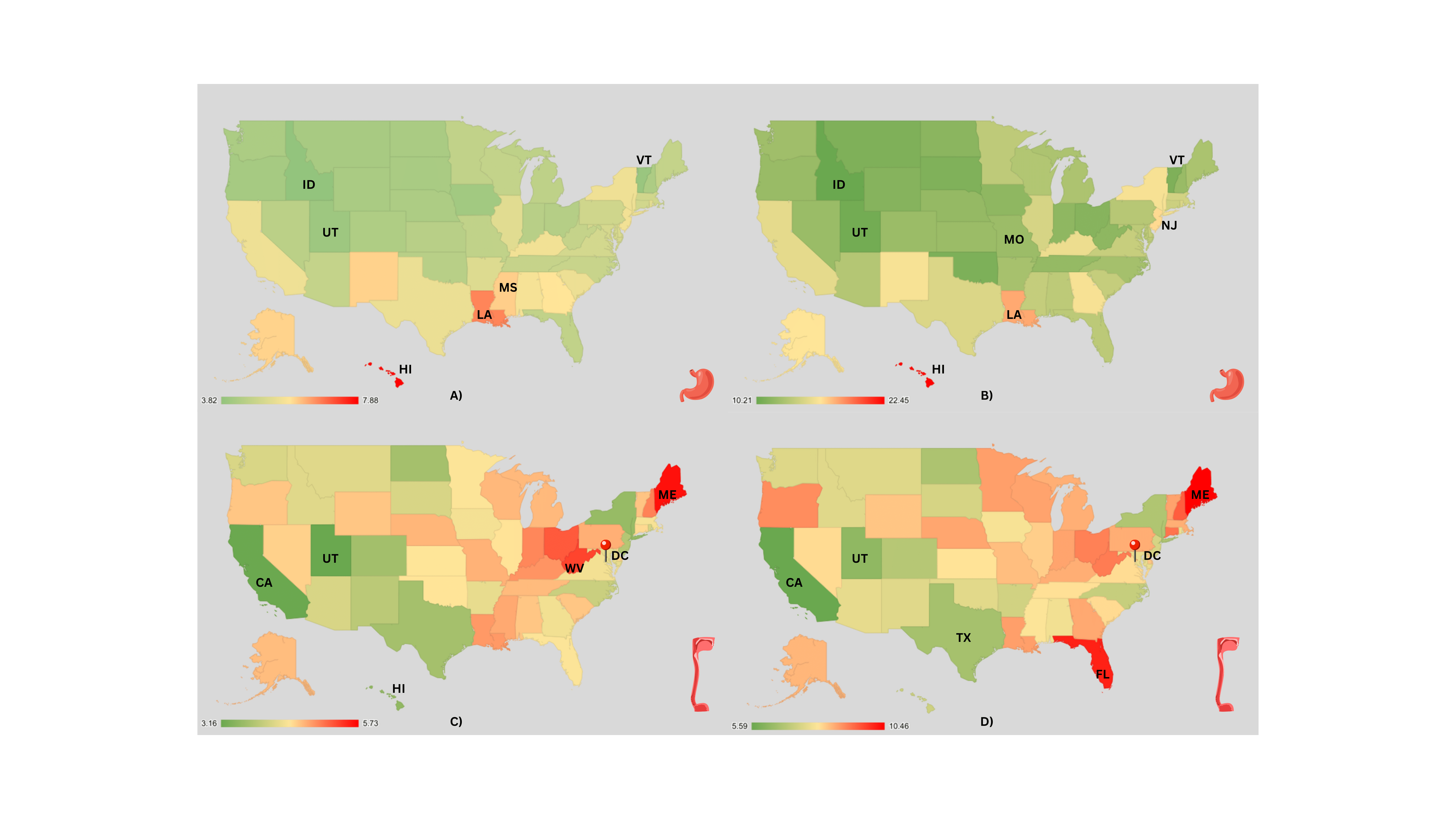
Figure: Figure1: Geographic distribution of age-standardized incidence and prevalence rates (per 100,000 population) of stomach and esophageal cancers across U.S. states based on GBD 2021 data.
A) Stomach cancer incidence; B) Stomach cancer prevalence; C) Esophageal cancer incidence; D) Esophageal cancer prevalence.
Hotspots for stomach cancer include Hawaii, Louisiana, and Mississippi, while esophageal cancer clusters in the District of Columbia, Maine, and West Virginia. States with lowest burdens are consistently Utah, Idaho, and California.
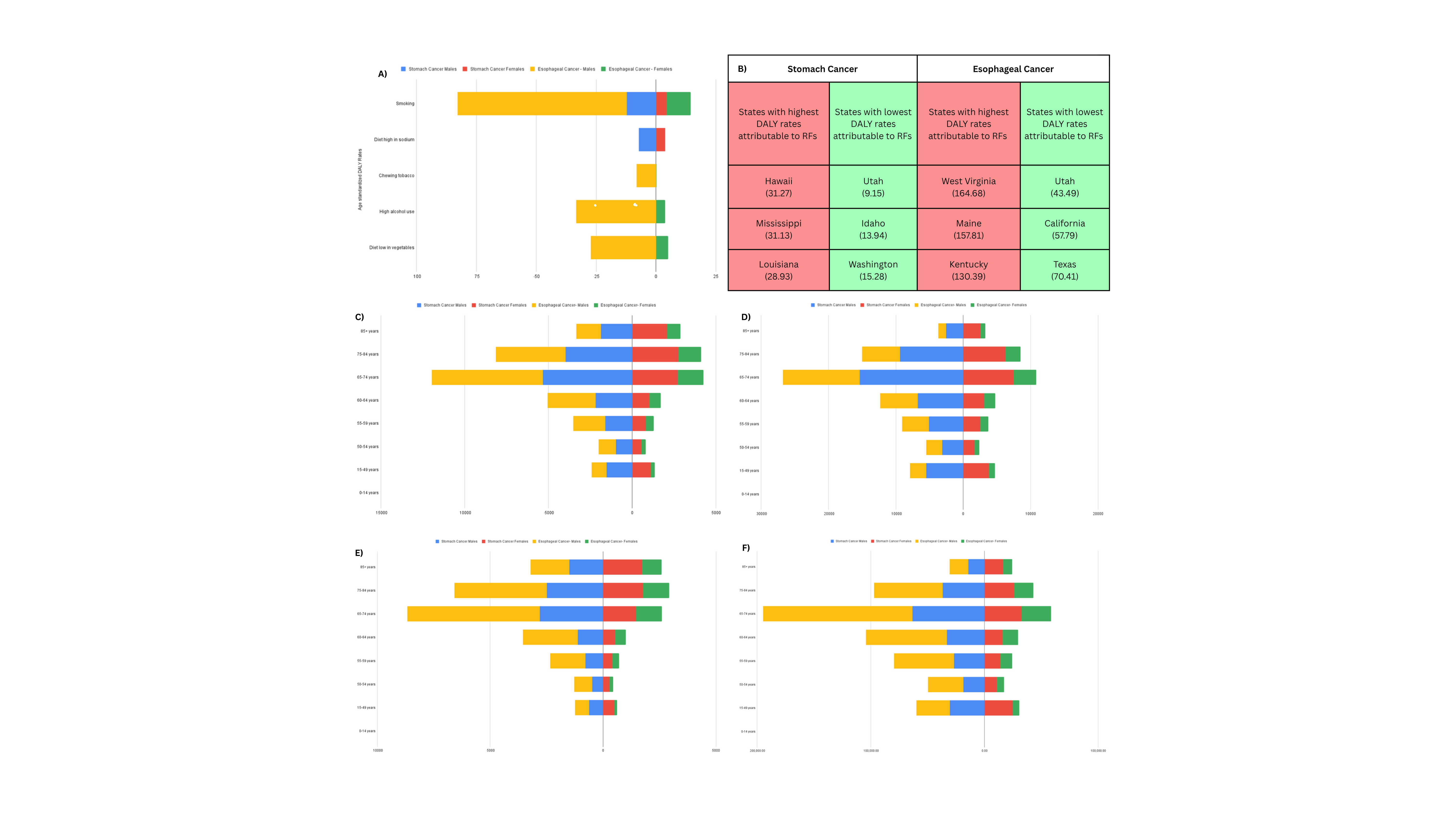
Figure: Figure 2: Comparative analysis of stomach and esophageal cancer burden in the U.S. based on GBD 2021 data.
A) Age-standardized DALY rates attributable to specific risk factors (RFs) by cancer type and gender.
B) U.S. states with the highest and lowest total DALY rates attributable to modifiable RFs for stomach and esophageal cancer.
C) Age group-wise distribution of incident cases by cancer type and gender.
D) Age group-wise prevalence numbers.
E) Age group-wise mortality counts.
F) Age group-wise total DALYs.
The 65–74 years age group consistently bears the highest burden across incidence, mortality, and DALYs for both cancers. Distinct RF patterns are observed, with smoking and high-sodium diets dominating for stomach cancer, and smoking, alcohol use, and chewing tobacco driving esophageal cancer burden.
Disclosures:
Rithish Nimmagadda indicated no relevant financial relationships.
Sameer Majety indicated no relevant financial relationships.
Nayanika Tummala indicated no relevant financial relationships.
Naga Praneeth Vakkalagadda indicated no relevant financial relationships.
Pragathi Munnangi indicated no relevant financial relationships.
Hemanth Kamadi indicated no relevant financial relationships.
Swathi Cherukuri indicated no relevant financial relationships.
Krishna Sai Kiran Sakalabaktula indicated no relevant financial relationships.
Rithish Nimmagadda, MBBS1, Sameer Majety, MBBS2, Nayanika Tummala, MD3, Naga Praneeth Vakkalagadda, MD4, Pragathi Munnangi, MD5, Hemanth Kamadi, MBBS6, Swathi Cherukuri, MBBS7, Krishna Sai Kiran Sakalabaktula, MBBS8. P0662 - Geographic and Risk Factor Disparities in Stomach and Esophageal Cancer Burden Across the US: Findings From GBD 2021, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2School of Medicine, Xiamen University., Kakinada, Andhra Pradesh, India; 3St. Mary's General Hospital, New York Medical College, Poughkeepsie, NY; 4University of Alabama at Birmingham Heersink School of Medicine, Montgomery, AL; 5BronxCare Health System, New York City, NY; 6School of Medicine, Xiamen University, China, Kakinada, Andhra Pradesh, India; 7Narayana Medical College, Nellore, Andhra Pradesh, India; 8Government General Hospital Kakinada, Kakinada, Andhra Pradesh, India
Introduction: Stomach and esophageal cancers remain significant contributors to cancer burden in the U.S., but their epidemiologic contours differ. This study uses GBD 2021 data to compare incidence, prevalence, and risk factor-attributable DALYs for these malignancies across states and age groups.
Methods: We used age-standardized incidence and prevalence rates to assess interstate variation. Gross case numbers were analyzed across age groups to identify high-burden subpopulations. For risk factor (RF) analysis, age-standardized DALY rates attributable to specific RFs were used.
Results: Stomach cancer incidence showed considerable geographic variation, with the Pacific and Southern States (Hawaii: 7.88, Louisiana: 6.70, Mississippi: 6.05) having the highest rates, and Mountain/Northern States (Idaho: 3.82, Vermont: 3.96, Utah: 4.03) the lowest. Prevalence patterns closely mirrored incidence. The highest DALYs and prevalence occurred in the 65–74 age group for both sexes, though peak incidence was at 65–74 in males and 85+ in females.
Esophageal cancer showed a different pattern. Incidence was highest in the District of Columbia (5.73), Maine (5.64), and West Virginia (5.35), and lowest in Utah (3.16), California (3.17), and Hawaii (3.50). Males aged 65–74 bore the heaviest burden with 6,635 incident cases and 131,288 DALYs. For females, the highest incidence and DALYs were also seen at 65–74, while deaths peaked at 75–84.
Risk factor analysis uncovered distinct etiologies. Stomach cancer was primarily driven by habitual exposures such as smoking (DALY 13.09 in Mississippi) and high-sodium diets (8.24 in Hawaii). Esophageal cancer was linked to smoking (63.29 in West Virginia), alcohol use (30.03 in D.C.), low vegetable intake, and chewing tobacco—particularly in Appalachian and Northeastern states.
Discussion: Stomach cancer shows a coastal-southern pattern with dietary and tobacco RFs; esophageal cancer clusters in Appalachia/Northeast with multifactorial lifestyle drivers. The 65–74 age group consistently bears the heaviest load. Preventive strategies should include targeted smoking cessation in Appalachia, salt-reduction campaigns in the South, alcohol moderation in high-use states, and national initiatives to boost vegetable intake. State-level interventions must align with regional RF patterns to reduce this dual cancer burden.
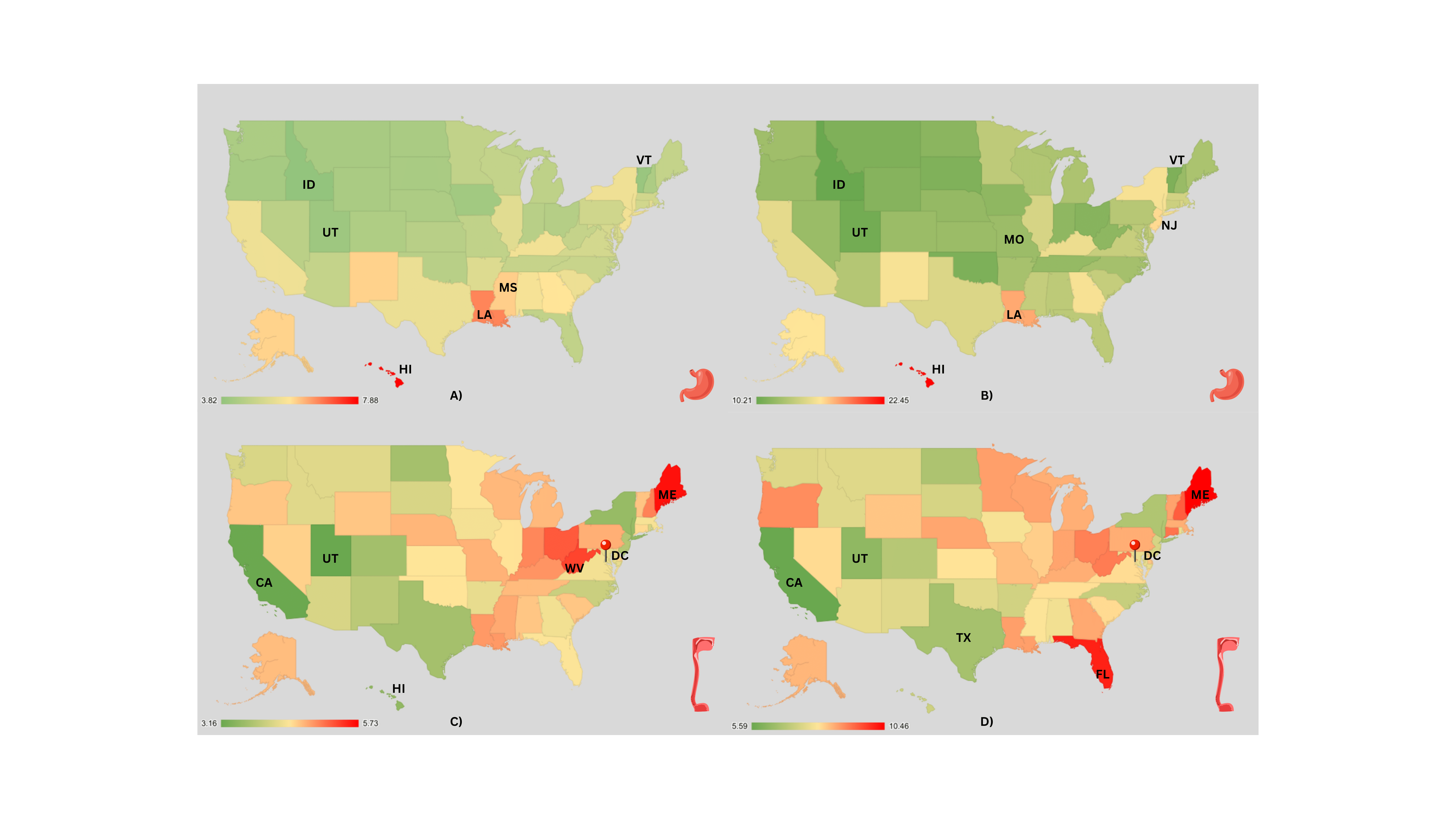
Figure: Figure1: Geographic distribution of age-standardized incidence and prevalence rates (per 100,000 population) of stomach and esophageal cancers across U.S. states based on GBD 2021 data.
A) Stomach cancer incidence; B) Stomach cancer prevalence; C) Esophageal cancer incidence; D) Esophageal cancer prevalence.
Hotspots for stomach cancer include Hawaii, Louisiana, and Mississippi, while esophageal cancer clusters in the District of Columbia, Maine, and West Virginia. States with lowest burdens are consistently Utah, Idaho, and California.
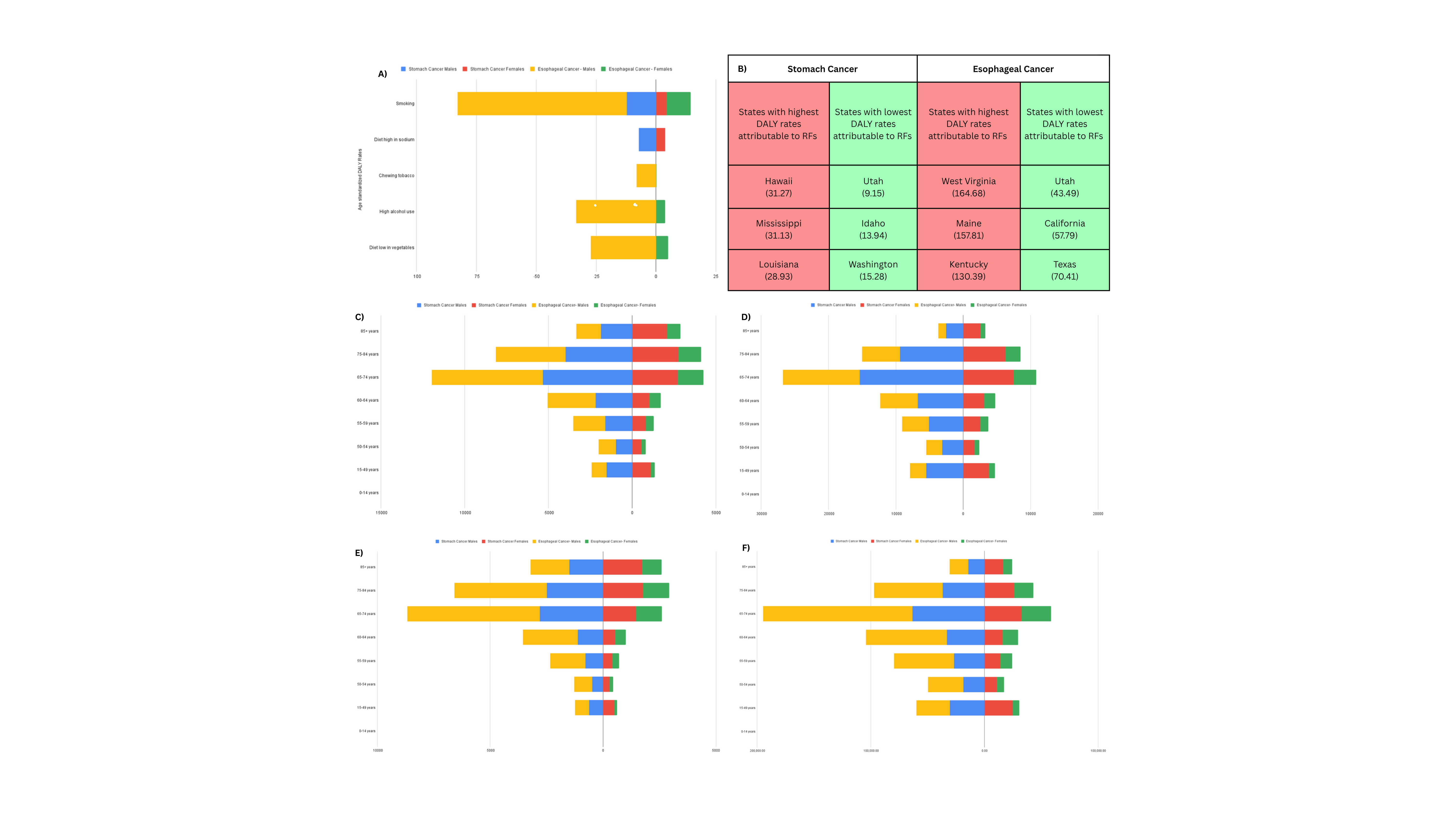
Figure: Figure 2: Comparative analysis of stomach and esophageal cancer burden in the U.S. based on GBD 2021 data.
A) Age-standardized DALY rates attributable to specific risk factors (RFs) by cancer type and gender.
B) U.S. states with the highest and lowest total DALY rates attributable to modifiable RFs for stomach and esophageal cancer.
C) Age group-wise distribution of incident cases by cancer type and gender.
D) Age group-wise prevalence numbers.
E) Age group-wise mortality counts.
F) Age group-wise total DALYs.
The 65–74 years age group consistently bears the highest burden across incidence, mortality, and DALYs for both cancers. Distinct RF patterns are observed, with smoking and high-sodium diets dominating for stomach cancer, and smoking, alcohol use, and chewing tobacco driving esophageal cancer burden.
Disclosures:
Rithish Nimmagadda indicated no relevant financial relationships.
Sameer Majety indicated no relevant financial relationships.
Nayanika Tummala indicated no relevant financial relationships.
Naga Praneeth Vakkalagadda indicated no relevant financial relationships.
Pragathi Munnangi indicated no relevant financial relationships.
Hemanth Kamadi indicated no relevant financial relationships.
Swathi Cherukuri indicated no relevant financial relationships.
Krishna Sai Kiran Sakalabaktula indicated no relevant financial relationships.
Rithish Nimmagadda, MBBS1, Sameer Majety, MBBS2, Nayanika Tummala, MD3, Naga Praneeth Vakkalagadda, MD4, Pragathi Munnangi, MD5, Hemanth Kamadi, MBBS6, Swathi Cherukuri, MBBS7, Krishna Sai Kiran Sakalabaktula, MBBS8. P0662 - Geographic and Risk Factor Disparities in Stomach and Esophageal Cancer Burden Across the US: Findings From GBD 2021, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
