Sunday Poster Session
Category: Esophagus
P0656 - Comparative Efficacy and Safety of Radiofrequency Ablation vs Cryoablation for Dysplastic Barrett’s Esophagus: A Systematic Review and Meta-Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Pragathi Munnangi, MD (she/her/hers)
BronxCare Health System
New York City, NY
Presenting Author(s)
Karthik Chintharala, MBBS1, Pragathi Munnangi, MD2, Rithish Nimmagadda, MBBS3, Naga Praneeth Vakkalagadda, MD4, Bhargav Koyani, MD5, Vineeth Potluri, MD6
1NRI Academy of Medical Sciences, Vijayawada, Andhra Pradesh, India; 2BronxCare Health System, New York City, NY; 3One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 4University of Alabama at Birmingham Heersink School of Medicine, Montgomery, AL; 5Ascension Saint Francis Hospital, Evanston, IL; 6Cleveland Clinic, Cleveland, OH
Introduction: Barrett’s esophagus (BE), a premalignant condition, arising from chronic gastroesophageal reflux disease (GERD), carries a substantial risk of progression to esophageal adenocarcinoma. Endoscopic ablative therapies, including Radiofrequency ablation (RFA) and Cryoablation, are widely used to eradicate dysplastic BE. Although both modalities are routinely used, their comparative efficacy and safety profiles remain subjects of ongoing investigation.
Methods: We performed a systematic review and meta-analysis in accordance with PRISMA guidelines. A thorough literature search was conducted across PubMed, Embase, Scopus, and the Cochrane Library up to May 2025. Studies were eligible if they directly compared Radiofrequency ablation (RFA) and Cryoablation in adult patients diagnosed with dysplastic Barrett’s esophagus. Primary outcomes assessed were complete eradication of dysplasia (CE-D) and complete eradication of intestinal metaplasia (CE-IM). Secondary outcomes included recurrence, adverse events, and post-procedural stricture formation. A random-effects model was used to calculate pooled effect sizes. Heterogeneity was assessed using the I² statistic.
Results: A total of 3,114 patients across 12 studies were analyzed in our meta-analysis to compare efficacy and safety of Radiofrequency ablation with Cryoablation in Barrett's Esophagus. Radiofrequency ablation showed a slight advantage over Cryoablation in achieving CE-D (RR 1.05; 95% CI 1.01–1.08; p=0.0072; I²=0%) and CE-IM (RR 1.06; 95% CI 1.00–1.11; p=0.0329; I²=0%), and Complete eradication of intestinal metaplasia (CE-IM) (RR 1.06; 95% CI 1.00–1.11; p=0.0329; I²=0%) which are statistically significant. However, RFA was associated with a significantly higher risk of post-procedural stricture formation (RR 2.41; 95% CI 1.65–3.51; p< 0.0001; I²=0%). All analysis showed no heterogeneity, supporting that these findings are consistent among the studies.
Discussion: Radiofrequency ablation offers marginally higher dysplasia and intestinal metaplasia eradication rates compared to cryoablation but at the cost of a significantly increased risk of strictures. Treatment choice should be individualized based on patient characteristics and procedural risk profiles.
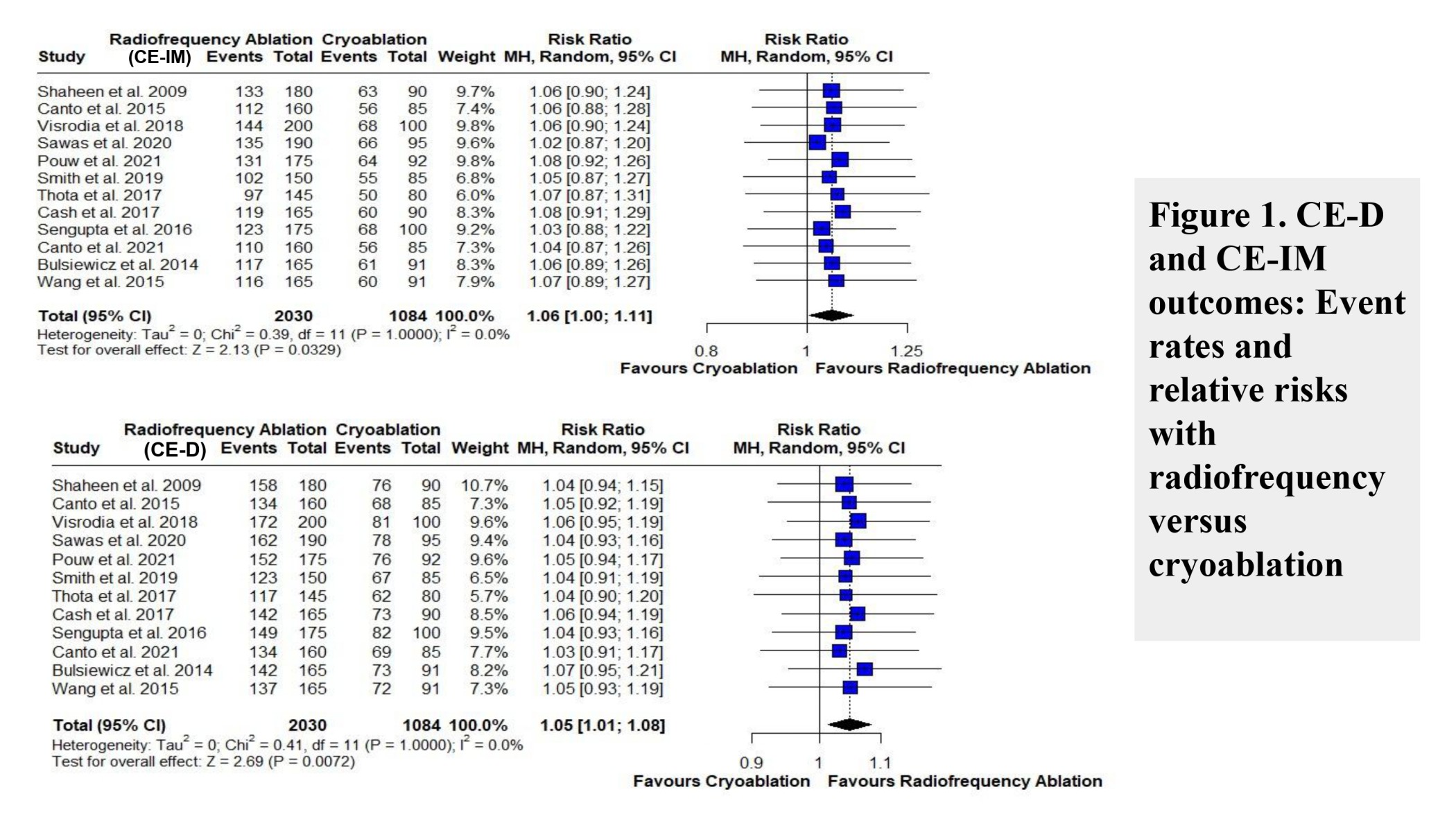
Figure: Figure 1. CE-D and CE-IM outcomes: Event rates and relative risks with radiofrequency versus cryoablation
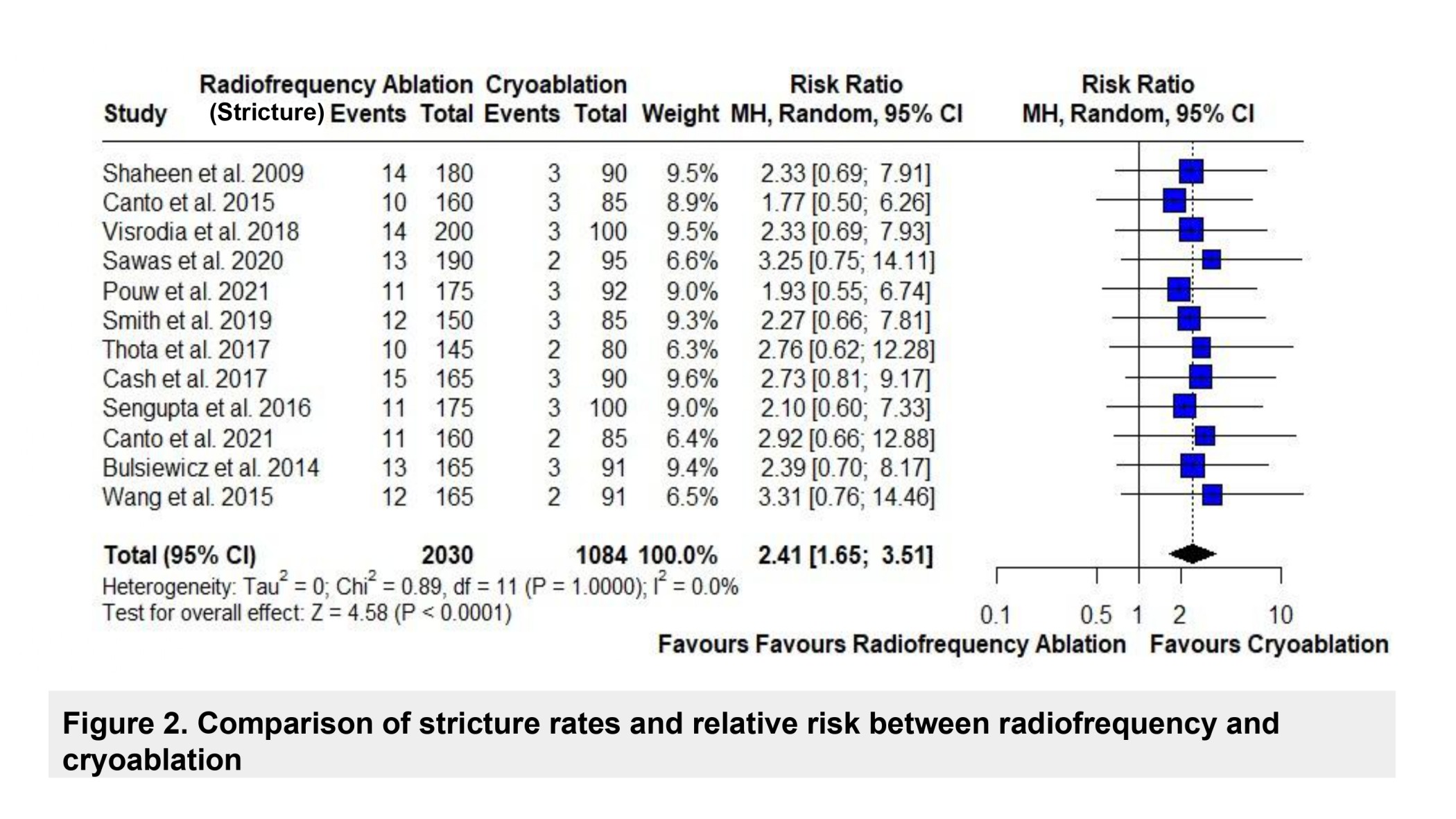
Figure: Figure 2. Comparison of stricture rates and relative risk between radiofrequency and cryoablation
Disclosures:
Karthik Chintharala indicated no relevant financial relationships.
Pragathi Munnangi indicated no relevant financial relationships.
Rithish Nimmagadda indicated no relevant financial relationships.
Naga Praneeth Vakkalagadda indicated no relevant financial relationships.
Bhargav Koyani indicated no relevant financial relationships.
Vineeth Potluri indicated no relevant financial relationships.
Karthik Chintharala, MBBS1, Pragathi Munnangi, MD2, Rithish Nimmagadda, MBBS3, Naga Praneeth Vakkalagadda, MD4, Bhargav Koyani, MD5, Vineeth Potluri, MD6. P0656 - Comparative Efficacy and Safety of Radiofrequency Ablation vs Cryoablation for Dysplastic Barrett’s Esophagus: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NRI Academy of Medical Sciences, Vijayawada, Andhra Pradesh, India; 2BronxCare Health System, New York City, NY; 3One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 4University of Alabama at Birmingham Heersink School of Medicine, Montgomery, AL; 5Ascension Saint Francis Hospital, Evanston, IL; 6Cleveland Clinic, Cleveland, OH
Introduction: Barrett’s esophagus (BE), a premalignant condition, arising from chronic gastroesophageal reflux disease (GERD), carries a substantial risk of progression to esophageal adenocarcinoma. Endoscopic ablative therapies, including Radiofrequency ablation (RFA) and Cryoablation, are widely used to eradicate dysplastic BE. Although both modalities are routinely used, their comparative efficacy and safety profiles remain subjects of ongoing investigation.
Methods: We performed a systematic review and meta-analysis in accordance with PRISMA guidelines. A thorough literature search was conducted across PubMed, Embase, Scopus, and the Cochrane Library up to May 2025. Studies were eligible if they directly compared Radiofrequency ablation (RFA) and Cryoablation in adult patients diagnosed with dysplastic Barrett’s esophagus. Primary outcomes assessed were complete eradication of dysplasia (CE-D) and complete eradication of intestinal metaplasia (CE-IM). Secondary outcomes included recurrence, adverse events, and post-procedural stricture formation. A random-effects model was used to calculate pooled effect sizes. Heterogeneity was assessed using the I² statistic.
Results: A total of 3,114 patients across 12 studies were analyzed in our meta-analysis to compare efficacy and safety of Radiofrequency ablation with Cryoablation in Barrett's Esophagus. Radiofrequency ablation showed a slight advantage over Cryoablation in achieving CE-D (RR 1.05; 95% CI 1.01–1.08; p=0.0072; I²=0%) and CE-IM (RR 1.06; 95% CI 1.00–1.11; p=0.0329; I²=0%), and Complete eradication of intestinal metaplasia (CE-IM) (RR 1.06; 95% CI 1.00–1.11; p=0.0329; I²=0%) which are statistically significant. However, RFA was associated with a significantly higher risk of post-procedural stricture formation (RR 2.41; 95% CI 1.65–3.51; p< 0.0001; I²=0%). All analysis showed no heterogeneity, supporting that these findings are consistent among the studies.
Discussion: Radiofrequency ablation offers marginally higher dysplasia and intestinal metaplasia eradication rates compared to cryoablation but at the cost of a significantly increased risk of strictures. Treatment choice should be individualized based on patient characteristics and procedural risk profiles.
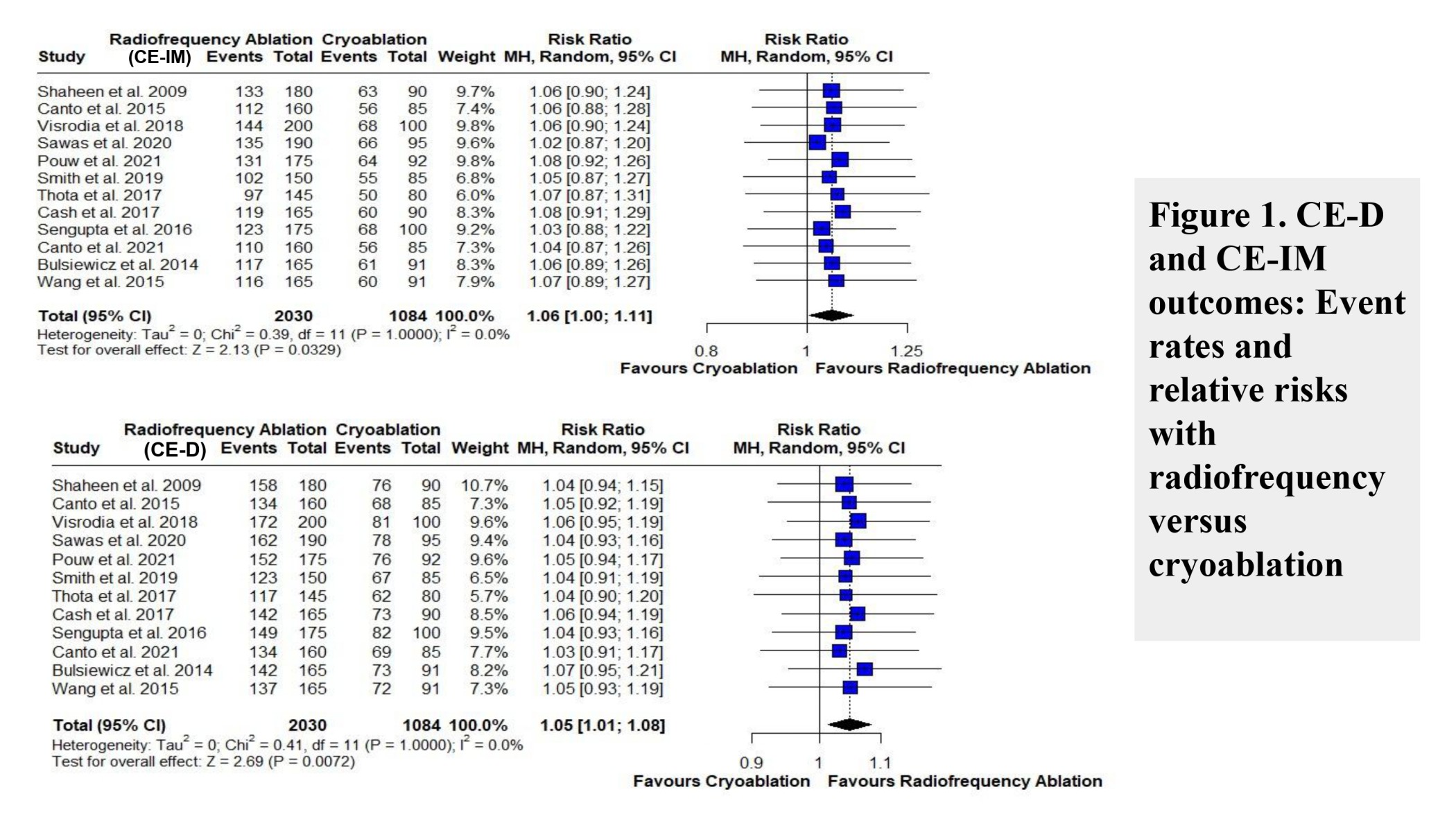
Figure: Figure 1. CE-D and CE-IM outcomes: Event rates and relative risks with radiofrequency versus cryoablation
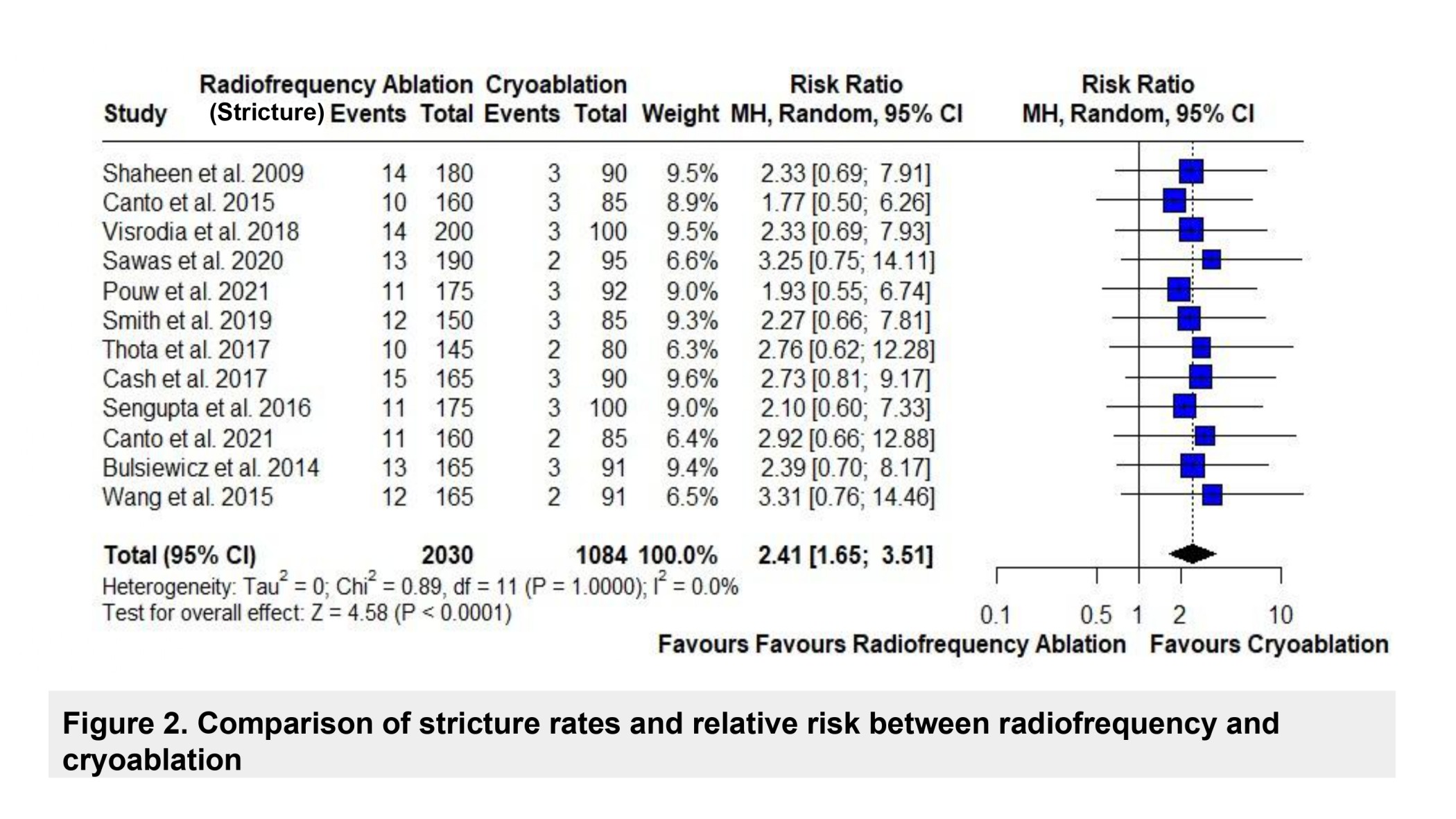
Figure: Figure 2. Comparison of stricture rates and relative risk between radiofrequency and cryoablation
Disclosures:
Karthik Chintharala indicated no relevant financial relationships.
Pragathi Munnangi indicated no relevant financial relationships.
Rithish Nimmagadda indicated no relevant financial relationships.
Naga Praneeth Vakkalagadda indicated no relevant financial relationships.
Bhargav Koyani indicated no relevant financial relationships.
Vineeth Potluri indicated no relevant financial relationships.
Karthik Chintharala, MBBS1, Pragathi Munnangi, MD2, Rithish Nimmagadda, MBBS3, Naga Praneeth Vakkalagadda, MD4, Bhargav Koyani, MD5, Vineeth Potluri, MD6. P0656 - Comparative Efficacy and Safety of Radiofrequency Ablation vs Cryoablation for Dysplastic Barrett’s Esophagus: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
