Sunday Poster Session
Category: Esophagus
P0655 - Optimizing Proton Pump Inhibitor Use at a Safety-Net Provider Hospital
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rohan Ahuja, MD
University of Texas at Houston
Houston, TX
Presenting Author(s)
Rohan Ahuja, MD1, George Ishac, MD1, Faraz Jafri, MD1, Kazi Haque, MD2, Fehintola Soetan, MD1, Jason Lin, MD1, Mariam Rizvi, MD1, Mohammad Adil Qasim, PharmD1, Rukma Govindu, MD1
1University of Texas at Houston, Houston, TX; 2University of Texas Health Science Center, Houston, TX
Introduction: In 2022, the American Gastroenterology Association (AGA) released a clinical practice update regarding de-prescribing proton pump inhibitors (PPI). Anywhere from 7-15% patients use PPIs at any time. Patients over 70 have an estimated prevalence of 40% for PPI use. PPI use in the long term has been associated with several adverse effects including chronic kidney disease, electrolyte imbalances, and dementia. These associations are from observational studies and no direct causality can be created between the two groups. Nonetheless, the long-term safety of PPI use is brought into question and further evaluation is needed. In this study, we sought to evaluate this at LBJ hospital in Houston to evaluate the extent of PPI overprescription and apply interventions to reduce overprescription.
Methods: Patients discharged from LBJ Hospital from 7/1/2024 to 12/31/2024 were included in the study. IRB approval was obtained. Baseline characteristics were collected along with data surrounding the PPI prescription, type, duration, dose, and indication. Follow-up data was also collected including any esophagogastroduodenoscopies (EGD), adverse events, or reactions. PHI was protected using a linking log and all information was securely stored on one device with an encrypted file.
Results: Of the 260 patients discharged with PPIs, 73 (28.0%) of those patients did not have an appropriate indication. Notably, 155 (59.6%) patients did not have an appropriate duration for PPI. Most commonly, patients were given a 90 day prescription though the average prescription length for patients was 122 days. The most common diagnosis associated happened to be GERD with 61 patients having the diagnosis code. 103 (39.6%) patients did not have provider follow-up on the proton pump inhibitor for discontinuation or adjustment. 73 (28.0%) underwent EGD near time of diagnosis with 28 (10.8%) patients having esophagitis, ulcers, erosions, or Barretts that would warrant therapy. However, only 2 patients qualified for prolonged treatment.
Discussion: We were able to demonstrate a significant portion of patients who both had an inadequate diagnosis associated with prescription as well as those with an inappropriate duration of prescription. This is likely due to the limited access to follow up at the institution as well as a mechanism of the default prescription. Additionally, discussion of reflux is often ignored in hospitalization where not as much time is able to be dedicated to thorough prescription monitoring.
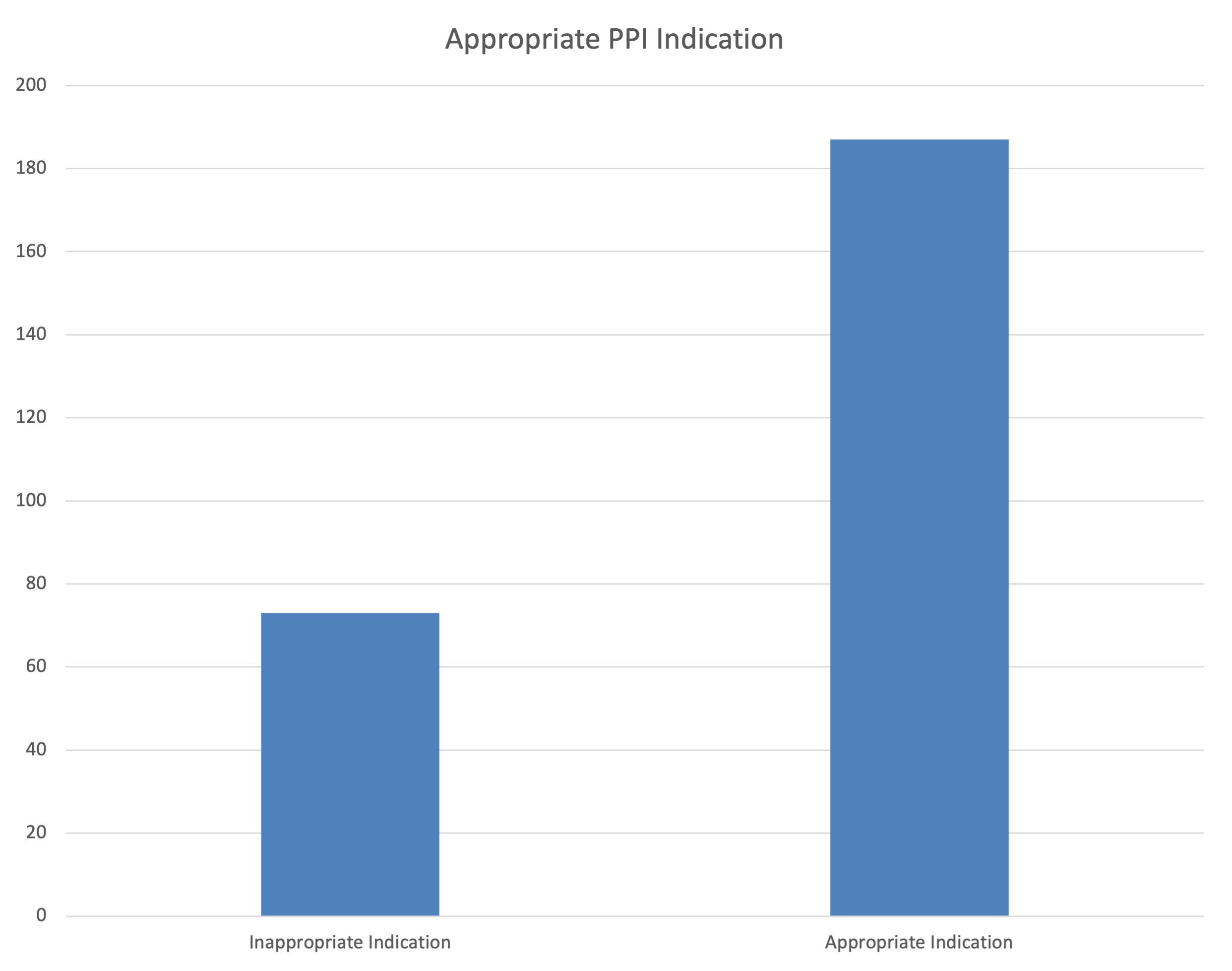
Figure: Patients with inappropriate versus appropriate indications of PPI. Indications were based on the 2022 AGA clinical practice update regarding appropriate PPI indications.
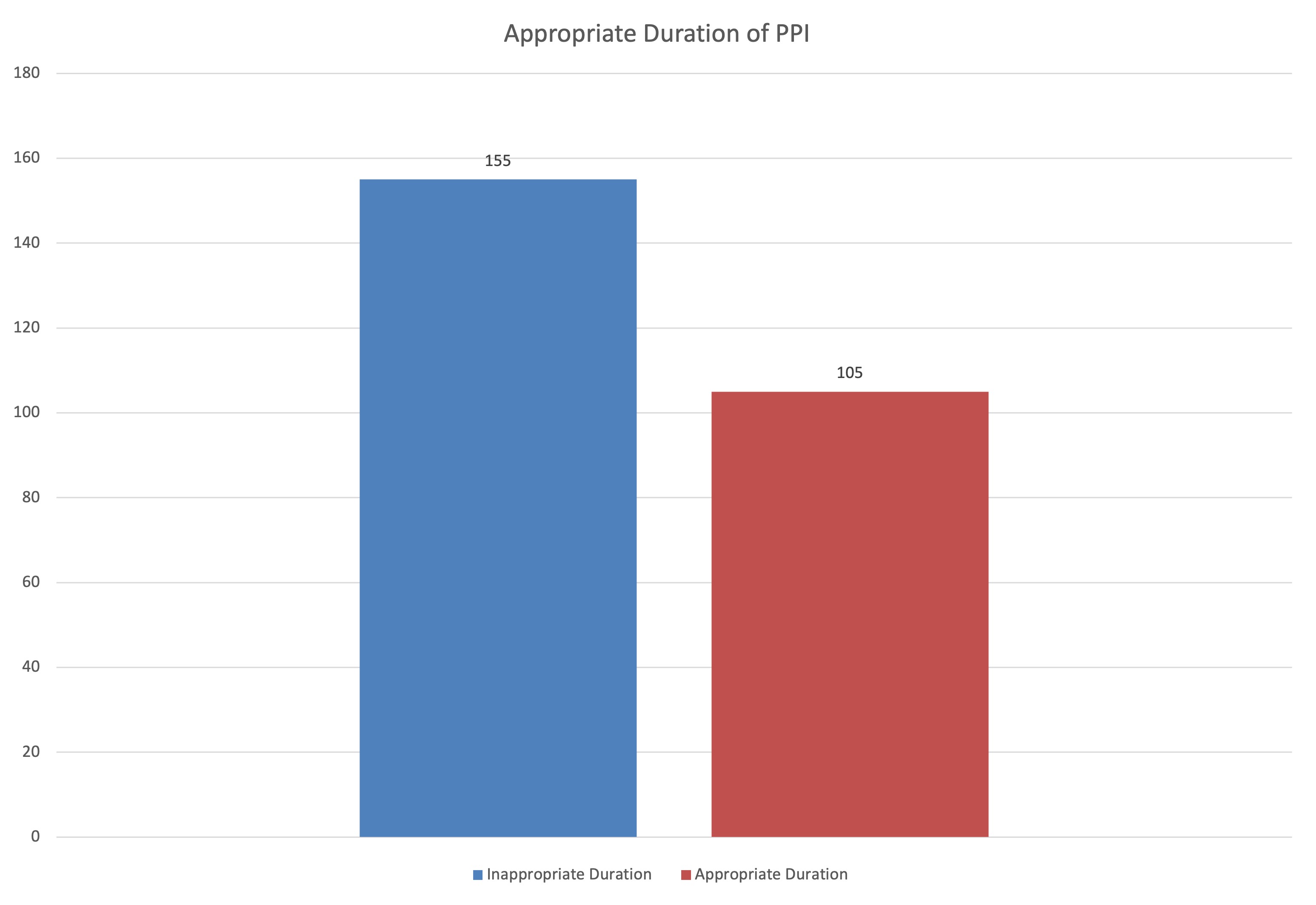
Figure: Patients with appropriate versus inappropriate duration of PPI. Durations were based on the 2022 AGA clinical practice update regarding appropriate PPI indications.
Disclosures:
Rohan Ahuja indicated no relevant financial relationships.
George Ishac indicated no relevant financial relationships.
Faraz Jafri indicated no relevant financial relationships.
Kazi Haque indicated no relevant financial relationships.
Fehintola Soetan indicated no relevant financial relationships.
Jason Lin indicated no relevant financial relationships.
Mariam Rizvi indicated no relevant financial relationships.
Mohammad Adil Qasim indicated no relevant financial relationships.
Rukma Govindu indicated no relevant financial relationships.
Rohan Ahuja, MD1, George Ishac, MD1, Faraz Jafri, MD1, Kazi Haque, MD2, Fehintola Soetan, MD1, Jason Lin, MD1, Mariam Rizvi, MD1, Mohammad Adil Qasim, PharmD1, Rukma Govindu, MD1. P0655 - Optimizing Proton Pump Inhibitor Use at a Safety-Net Provider Hospital, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas at Houston, Houston, TX; 2University of Texas Health Science Center, Houston, TX
Introduction: In 2022, the American Gastroenterology Association (AGA) released a clinical practice update regarding de-prescribing proton pump inhibitors (PPI). Anywhere from 7-15% patients use PPIs at any time. Patients over 70 have an estimated prevalence of 40% for PPI use. PPI use in the long term has been associated with several adverse effects including chronic kidney disease, electrolyte imbalances, and dementia. These associations are from observational studies and no direct causality can be created between the two groups. Nonetheless, the long-term safety of PPI use is brought into question and further evaluation is needed. In this study, we sought to evaluate this at LBJ hospital in Houston to evaluate the extent of PPI overprescription and apply interventions to reduce overprescription.
Methods: Patients discharged from LBJ Hospital from 7/1/2024 to 12/31/2024 were included in the study. IRB approval was obtained. Baseline characteristics were collected along with data surrounding the PPI prescription, type, duration, dose, and indication. Follow-up data was also collected including any esophagogastroduodenoscopies (EGD), adverse events, or reactions. PHI was protected using a linking log and all information was securely stored on one device with an encrypted file.
Results: Of the 260 patients discharged with PPIs, 73 (28.0%) of those patients did not have an appropriate indication. Notably, 155 (59.6%) patients did not have an appropriate duration for PPI. Most commonly, patients were given a 90 day prescription though the average prescription length for patients was 122 days. The most common diagnosis associated happened to be GERD with 61 patients having the diagnosis code. 103 (39.6%) patients did not have provider follow-up on the proton pump inhibitor for discontinuation or adjustment. 73 (28.0%) underwent EGD near time of diagnosis with 28 (10.8%) patients having esophagitis, ulcers, erosions, or Barretts that would warrant therapy. However, only 2 patients qualified for prolonged treatment.
Discussion: We were able to demonstrate a significant portion of patients who both had an inadequate diagnosis associated with prescription as well as those with an inappropriate duration of prescription. This is likely due to the limited access to follow up at the institution as well as a mechanism of the default prescription. Additionally, discussion of reflux is often ignored in hospitalization where not as much time is able to be dedicated to thorough prescription monitoring.
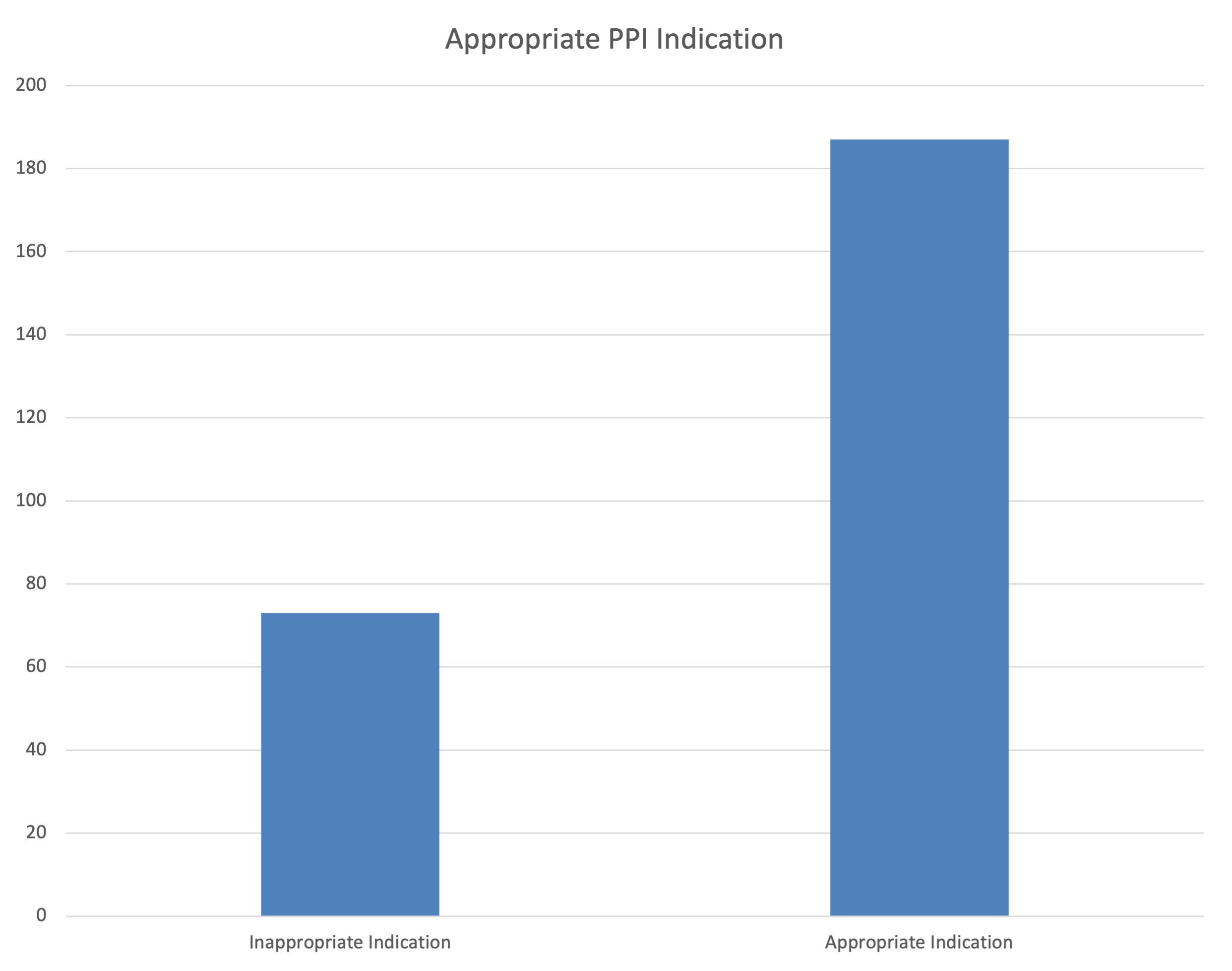
Figure: Patients with inappropriate versus appropriate indications of PPI. Indications were based on the 2022 AGA clinical practice update regarding appropriate PPI indications.
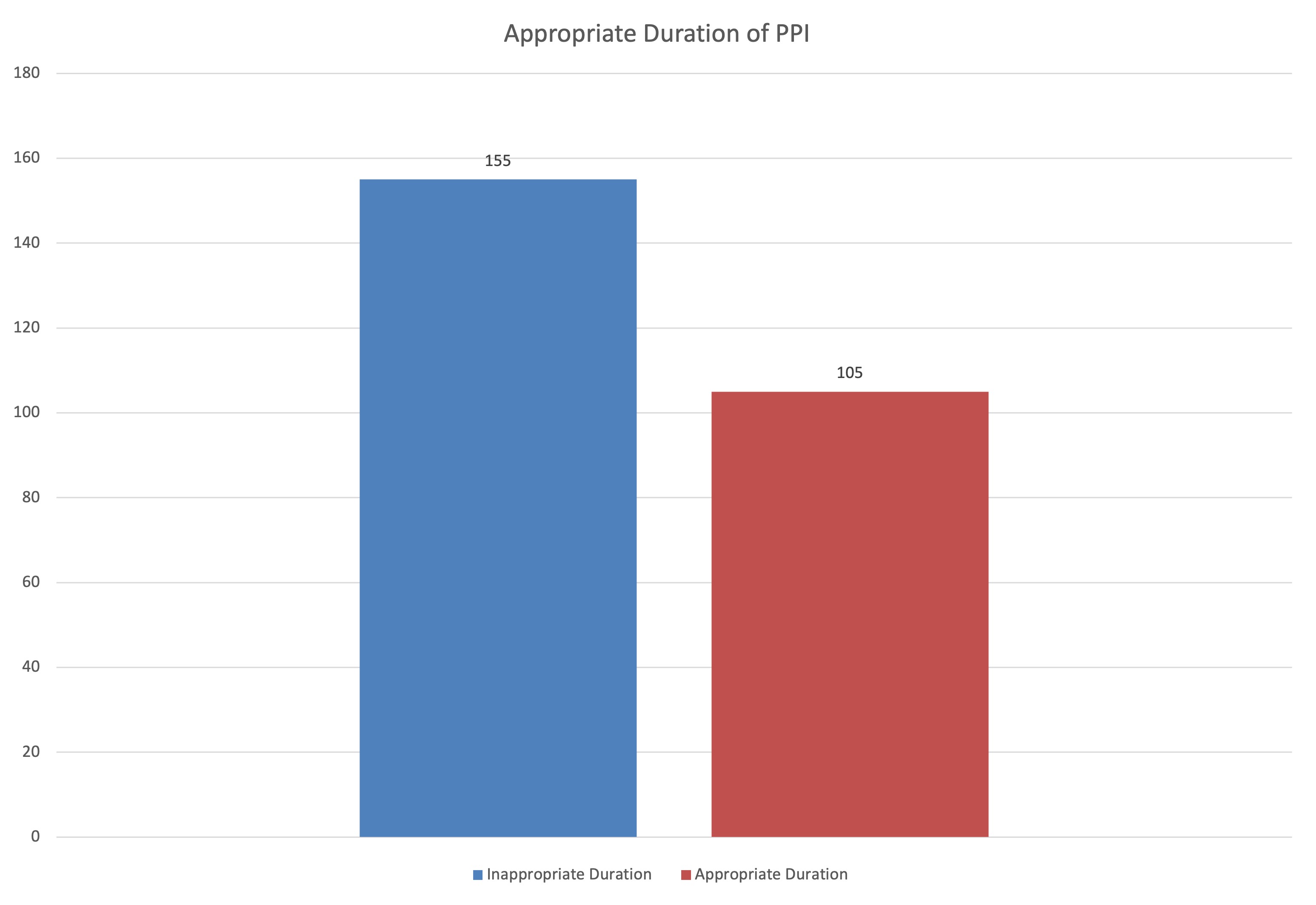
Figure: Patients with appropriate versus inappropriate duration of PPI. Durations were based on the 2022 AGA clinical practice update regarding appropriate PPI indications.
Disclosures:
Rohan Ahuja indicated no relevant financial relationships.
George Ishac indicated no relevant financial relationships.
Faraz Jafri indicated no relevant financial relationships.
Kazi Haque indicated no relevant financial relationships.
Fehintola Soetan indicated no relevant financial relationships.
Jason Lin indicated no relevant financial relationships.
Mariam Rizvi indicated no relevant financial relationships.
Mohammad Adil Qasim indicated no relevant financial relationships.
Rukma Govindu indicated no relevant financial relationships.
Rohan Ahuja, MD1, George Ishac, MD1, Faraz Jafri, MD1, Kazi Haque, MD2, Fehintola Soetan, MD1, Jason Lin, MD1, Mariam Rizvi, MD1, Mohammad Adil Qasim, PharmD1, Rukma Govindu, MD1. P0655 - Optimizing Proton Pump Inhibitor Use at a Safety-Net Provider Hospital, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
