Sunday Poster Session
Category: Esophagus
P0638 - Incidence of Barrett’s Esophagus Following Sleeve Gastrectomy Compared to Patients With GERD
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- CW
Carolyn Wilson, MD
NYU Langone Health
New York, NY
Presenting Author(s)
Carolyn Wilson, MD1, Juan Cerezo, MD2, Shaili Babbar, MD, MBA2, Cooper Urban, BS2, Andy Qiao, BS2, Emily K. Lock, BA2, Theodore M. Hill, BA2, Anuraag Gopaluni, PhD3, Shreya Chablaney, MD1, Abraham Khan, MD1, Christine Ren-Fielding, MD1, Rita Knotts, MD1
1NYU Langone Health, New York, NY; 2New York University Langone Health, New York, NY; 3Harvard T.H. Chan School of Public Health, Cambridge, MA
Introduction: Gastroesophageal reflux disease (GERD) is a well-established risk factor for the development of Barrett’s Esophagus (BE), a premalignant condition characterized by metaplastic changes in the esophageal mucosa. Sleeve gastrectomy (SG) has been linked to an increased incidence of GERD and is therefore considered a risk factor for BE. In 2021, a meta-analysis by Qumseya et al. suggested an increased long-term risk of BE in patients who underwent SG. Additionally, the SLEEVEPASS trial reported an increased incidence of GERD symptoms and erosive esophagitis (EE) in SG patients when compared with Roux-en-Y patients at 10-year follow-up. These findings informed the 2024 ASGE GERD guidelines, which recommend BE screening in all post-SG patients regardless of symptoms. However, due to the limited evidence supporting screening in this population, our study aims to characterize the incidence of GERD, EE, and BE in patients who have undergone SG to better inform future guidelines.
Methods: This is a single-center retrospective case-control study comparing rates of EE and BE in adults with history of SG to controls without history of SG undergoing esophagogastroduodenoscopy (EGD) for GERD evaluation between 2015-2024. Patients were matched 1:1 by age (±5 years) and sex, with a total of 117 pairs. Exclusionary criteria included prior BE, alternative foregut surgery, and/or incomplete EGD data.
Results: Of the 117 SG patients, 63 (54%) had no documented history of GERD prior to surgery. Among these patients, 58 (92%) developed de novo GERD symptoms following SG. Table 1 depicts the rate of LA grade A esophagitis (LA-A), EE, and BE on EGD compared to patients with GERD without previous SG. Among patients without preexisting GERD, SG was not significantly associated with BE, EE, or LA-A compared to those who underwent EGD for GERD. Older age was independently associated with higher odds of LA-A (p = 0.008), but was not associated with BE or EE.
Discussion: Our results suggest that SG is associated with an increased risk of developing GERD. However, SG was not significantly associated with BE, EE, or LA-A compared to GERD controls. Older age was independently linked to higher odds of LA-A, suggesting age may be a stronger risk factor than surgical status. Our results did not correspond with prior studies that suggest increased risk of EE, but are largely limited by our small sample size. Large scale longitudinal studies are needed to characterize the risk of EE and BE in patients who have undergone SG.
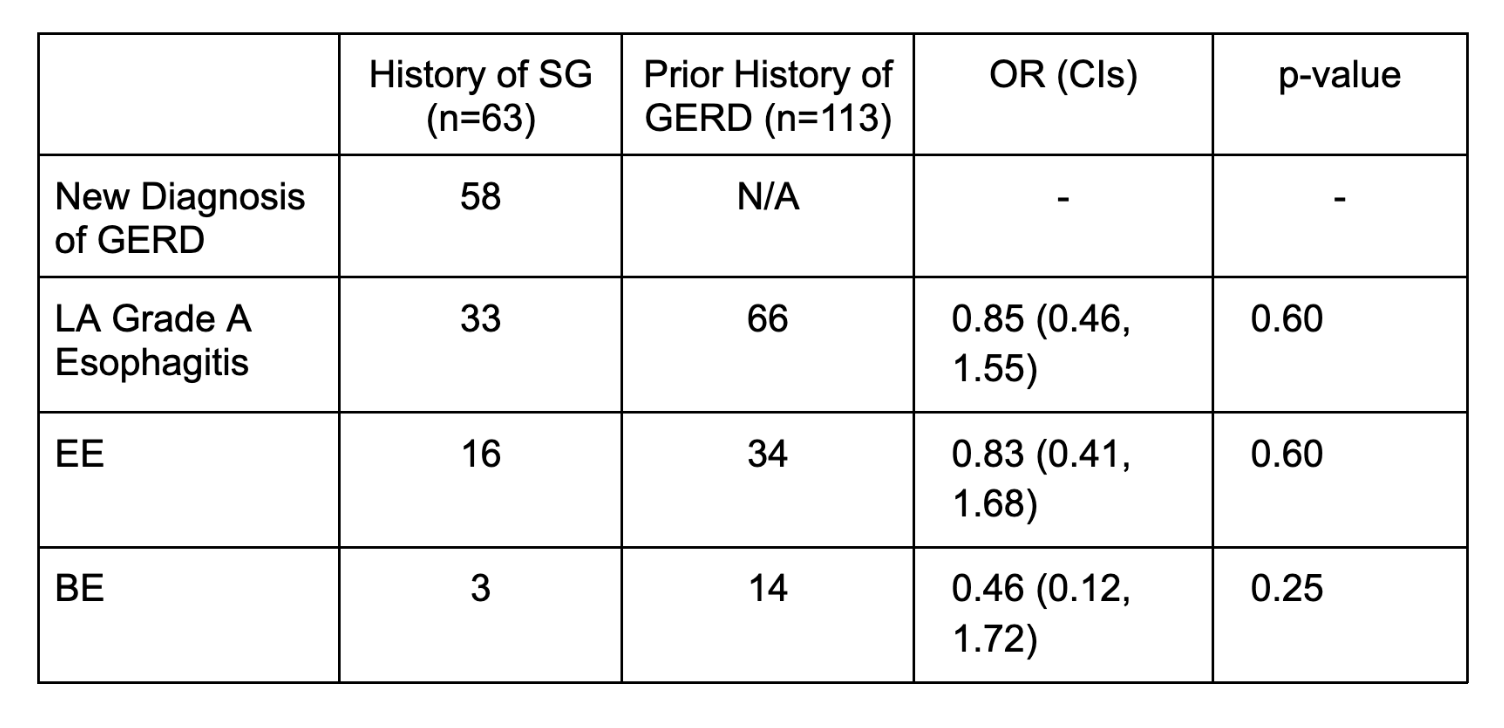
Figure: Table 1: Endoscopic outcomes in patients who developed GERD after SG compared to patients with GERD who have not undergone SG.
Disclosures:
Carolyn Wilson indicated no relevant financial relationships.
Juan Cerezo indicated no relevant financial relationships.
Shaili Babbar indicated no relevant financial relationships.
Cooper Urban indicated no relevant financial relationships.
Andy Qiao indicated no relevant financial relationships.
Emily Lock indicated no relevant financial relationships.
Theodore Hill indicated no relevant financial relationships.
Anuraag Gopaluni indicated no relevant financial relationships.
Shreya Chablaney: Phathom – Speakers Bureau.
Abraham Khan: Medtronic – Consultant. Phathom Pharmaceuticals – Speakers Bureau. Regeneron – Speakers Bureau. Sanofi – Speakers Bureau.
Christine Ren-Fielding indicated no relevant financial relationships.
Rita Knotts indicated no relevant financial relationships.
Carolyn Wilson, MD1, Juan Cerezo, MD2, Shaili Babbar, MD, MBA2, Cooper Urban, BS2, Andy Qiao, BS2, Emily K. Lock, BA2, Theodore M. Hill, BA2, Anuraag Gopaluni, PhD3, Shreya Chablaney, MD1, Abraham Khan, MD1, Christine Ren-Fielding, MD1, Rita Knotts, MD1. P0638 - Incidence of Barrett’s Esophagus Following Sleeve Gastrectomy Compared to Patients With GERD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYU Langone Health, New York, NY; 2New York University Langone Health, New York, NY; 3Harvard T.H. Chan School of Public Health, Cambridge, MA
Introduction: Gastroesophageal reflux disease (GERD) is a well-established risk factor for the development of Barrett’s Esophagus (BE), a premalignant condition characterized by metaplastic changes in the esophageal mucosa. Sleeve gastrectomy (SG) has been linked to an increased incidence of GERD and is therefore considered a risk factor for BE. In 2021, a meta-analysis by Qumseya et al. suggested an increased long-term risk of BE in patients who underwent SG. Additionally, the SLEEVEPASS trial reported an increased incidence of GERD symptoms and erosive esophagitis (EE) in SG patients when compared with Roux-en-Y patients at 10-year follow-up. These findings informed the 2024 ASGE GERD guidelines, which recommend BE screening in all post-SG patients regardless of symptoms. However, due to the limited evidence supporting screening in this population, our study aims to characterize the incidence of GERD, EE, and BE in patients who have undergone SG to better inform future guidelines.
Methods: This is a single-center retrospective case-control study comparing rates of EE and BE in adults with history of SG to controls without history of SG undergoing esophagogastroduodenoscopy (EGD) for GERD evaluation between 2015-2024. Patients were matched 1:1 by age (±5 years) and sex, with a total of 117 pairs. Exclusionary criteria included prior BE, alternative foregut surgery, and/or incomplete EGD data.
Results: Of the 117 SG patients, 63 (54%) had no documented history of GERD prior to surgery. Among these patients, 58 (92%) developed de novo GERD symptoms following SG. Table 1 depicts the rate of LA grade A esophagitis (LA-A), EE, and BE on EGD compared to patients with GERD without previous SG. Among patients without preexisting GERD, SG was not significantly associated with BE, EE, or LA-A compared to those who underwent EGD for GERD. Older age was independently associated with higher odds of LA-A (p = 0.008), but was not associated with BE or EE.
Discussion: Our results suggest that SG is associated with an increased risk of developing GERD. However, SG was not significantly associated with BE, EE, or LA-A compared to GERD controls. Older age was independently linked to higher odds of LA-A, suggesting age may be a stronger risk factor than surgical status. Our results did not correspond with prior studies that suggest increased risk of EE, but are largely limited by our small sample size. Large scale longitudinal studies are needed to characterize the risk of EE and BE in patients who have undergone SG.
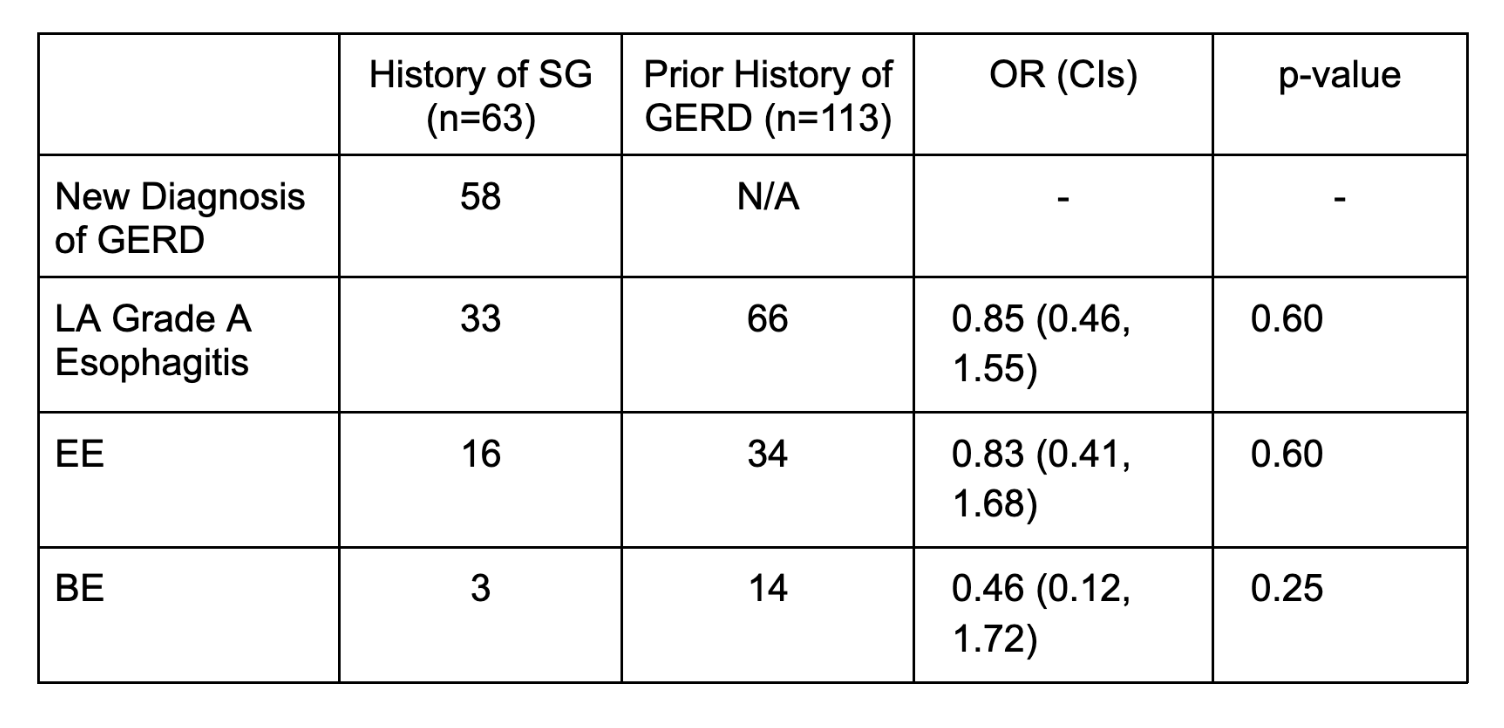
Figure: Table 1: Endoscopic outcomes in patients who developed GERD after SG compared to patients with GERD who have not undergone SG.
Disclosures:
Carolyn Wilson indicated no relevant financial relationships.
Juan Cerezo indicated no relevant financial relationships.
Shaili Babbar indicated no relevant financial relationships.
Cooper Urban indicated no relevant financial relationships.
Andy Qiao indicated no relevant financial relationships.
Emily Lock indicated no relevant financial relationships.
Theodore Hill indicated no relevant financial relationships.
Anuraag Gopaluni indicated no relevant financial relationships.
Shreya Chablaney: Phathom – Speakers Bureau.
Abraham Khan: Medtronic – Consultant. Phathom Pharmaceuticals – Speakers Bureau. Regeneron – Speakers Bureau. Sanofi – Speakers Bureau.
Christine Ren-Fielding indicated no relevant financial relationships.
Rita Knotts indicated no relevant financial relationships.
Carolyn Wilson, MD1, Juan Cerezo, MD2, Shaili Babbar, MD, MBA2, Cooper Urban, BS2, Andy Qiao, BS2, Emily K. Lock, BA2, Theodore M. Hill, BA2, Anuraag Gopaluni, PhD3, Shreya Chablaney, MD1, Abraham Khan, MD1, Christine Ren-Fielding, MD1, Rita Knotts, MD1. P0638 - Incidence of Barrett’s Esophagus Following Sleeve Gastrectomy Compared to Patients With GERD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

