Sunday Poster Session
Category: Esophagus
P0636 - Temporal Trends of High Grade Dysplasia in the Esophagus and GE Junction
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Nicholas Catanzaro, BS
Case Western Reserve University School of Medicine
Cleveland, OH
Presenting Author(s)
Nicholas Catanzaro, BS1, Rajesh Gupta, MSN, MS1, Andrew Catanzaro, MD2, Ashley Faulx, MD2, Wendy Brock, BSN, RN2, Beth Bednarchik, BSN, RN3, Joseph Willis, MD3, Amitabh Chak, MD, FACG3
1Case Western Reserve University School of Medicine, Cleveland, OH; 2Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 3University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Current guidelines that focus on the prevention and early detection of esophageal adenocarcinomas may not impact gastroesophageal junction adenocarcinomas, although both are rising in incidence in the United States. To determine the import and to help develop potential future strategies we retrospectively reviewed patients with high-grade dysplasia (HGD) of the esophagus and HGD of the gastroesophageal junction (GEJ) using a prospectively collected database.
Methods: Data on GERD symptoms, risk factors, endoscopic findings, and pathology have been collected prospectively since 1995 from all patients with non-dysplastic BE, dysplastic GEJ or dysplastic BE, and cancers of the esophagus or GEJ who consent. The database was searched to identify all patients with HGD. Three blinded endoscopists reviewed available de-identified images of the lower third of the esophagus and GEJ from 16 subjects with confirmed HGD and Prague maximum scores ≤ 1. Junctional HGD was defined as no visible columnar metaplasia in the distal esophagus, or involvement limited to a < 5 mm island. Cases where at least 2 endoscopists agreed were classified as junctional or short segment HGD. Chi-squares, fisher’s exact, or Student t-tests were calculated with R v4.5.0 to compare known BE risk factors between groups. The temporal incidence of junctional dysplasia and SSBE in the prospectively collected database was explored.
Results: Ten cases of junctional HGD (see images Fig. 1) , 31 cases of SSBE with HGD, and 90 cases of LSBE with HGD were identified. There was no significant difference in BE risk factors (male sex, white race, mean age, obesity, smoking history, GERD, or family history) found between groups. Temporally, HGD cases within SSBE and junctional HGD were only seen within the past 10 years (p-value = 0.0008) and past 5 years (p-value < 0.0001), respectively.
Discussion: Patients with junctional HGD who are at risk of progression to junctional cancer have the same risk factors as BE patients with HGD. Although current guidelines do not recommend endoscopic screening and surveillance for IM of the GEJ because the progression risk is low, junctional HGD appears to be increasing. Strategies to routinely identify junctional HGD may need to be developed to effectively prevent junctional adenocarcinomas.
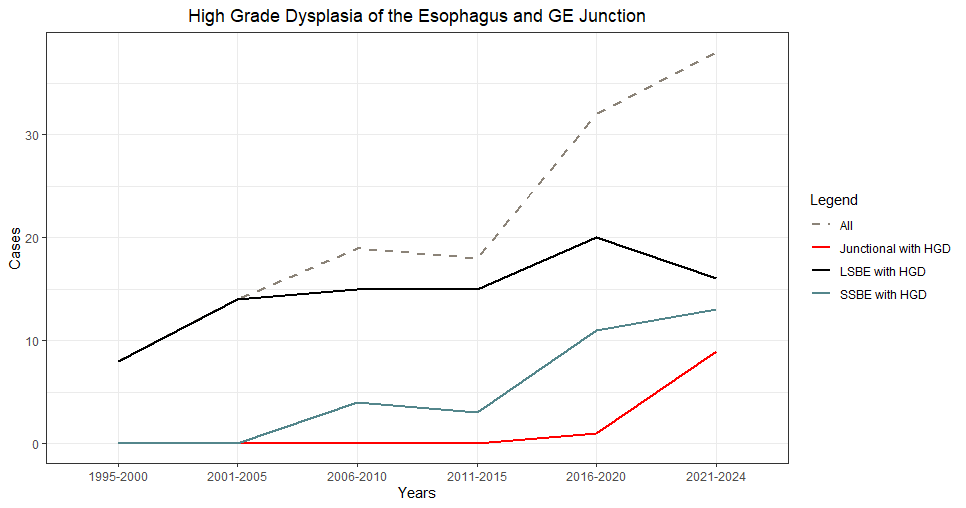
Figure: Cases of High-Grade Dysplasia. Total case counts were aggregated every 5 years.

Figure: Examples of images classified as “Junctional Dysplasia” by blinded endoscopists. Each image represents a different individual.
Disclosures:
Nicholas Catanzaro indicated no relevant financial relationships.
Rajesh Gupta indicated no relevant financial relationships.
Andrew Catanzaro indicated no relevant financial relationships.
Ashley Faulx: Steris – Consultant.
Wendy Brock indicated no relevant financial relationships.
Beth Bednarchik indicated no relevant financial relationships.
Joseph Willis: Lucid Diagnostics – Consultant, Intellectual Property/Patents, Royalties.
Amitabh Chak: Lucid Dx – Consultant, Grant/Research Support, Intellectual Property/Patents, Royalties, Stock Options, Stock-publicly held company(excluding mutual/index funds). MicroTech – Consultant. Pentax – Consultant. Steris – Consultant.
Nicholas Catanzaro, BS1, Rajesh Gupta, MSN, MS1, Andrew Catanzaro, MD2, Ashley Faulx, MD2, Wendy Brock, BSN, RN2, Beth Bednarchik, BSN, RN3, Joseph Willis, MD3, Amitabh Chak, MD, FACG3. P0636 - Temporal Trends of High Grade Dysplasia in the Esophagus and GE Junction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Case Western Reserve University School of Medicine, Cleveland, OH; 2Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 3University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Current guidelines that focus on the prevention and early detection of esophageal adenocarcinomas may not impact gastroesophageal junction adenocarcinomas, although both are rising in incidence in the United States. To determine the import and to help develop potential future strategies we retrospectively reviewed patients with high-grade dysplasia (HGD) of the esophagus and HGD of the gastroesophageal junction (GEJ) using a prospectively collected database.
Methods: Data on GERD symptoms, risk factors, endoscopic findings, and pathology have been collected prospectively since 1995 from all patients with non-dysplastic BE, dysplastic GEJ or dysplastic BE, and cancers of the esophagus or GEJ who consent. The database was searched to identify all patients with HGD. Three blinded endoscopists reviewed available de-identified images of the lower third of the esophagus and GEJ from 16 subjects with confirmed HGD and Prague maximum scores ≤ 1. Junctional HGD was defined as no visible columnar metaplasia in the distal esophagus, or involvement limited to a < 5 mm island. Cases where at least 2 endoscopists agreed were classified as junctional or short segment HGD. Chi-squares, fisher’s exact, or Student t-tests were calculated with R v4.5.0 to compare known BE risk factors between groups. The temporal incidence of junctional dysplasia and SSBE in the prospectively collected database was explored.
Results: Ten cases of junctional HGD (see images Fig. 1) , 31 cases of SSBE with HGD, and 90 cases of LSBE with HGD were identified. There was no significant difference in BE risk factors (male sex, white race, mean age, obesity, smoking history, GERD, or family history) found between groups. Temporally, HGD cases within SSBE and junctional HGD were only seen within the past 10 years (p-value = 0.0008) and past 5 years (p-value < 0.0001), respectively.
Discussion: Patients with junctional HGD who are at risk of progression to junctional cancer have the same risk factors as BE patients with HGD. Although current guidelines do not recommend endoscopic screening and surveillance for IM of the GEJ because the progression risk is low, junctional HGD appears to be increasing. Strategies to routinely identify junctional HGD may need to be developed to effectively prevent junctional adenocarcinomas.
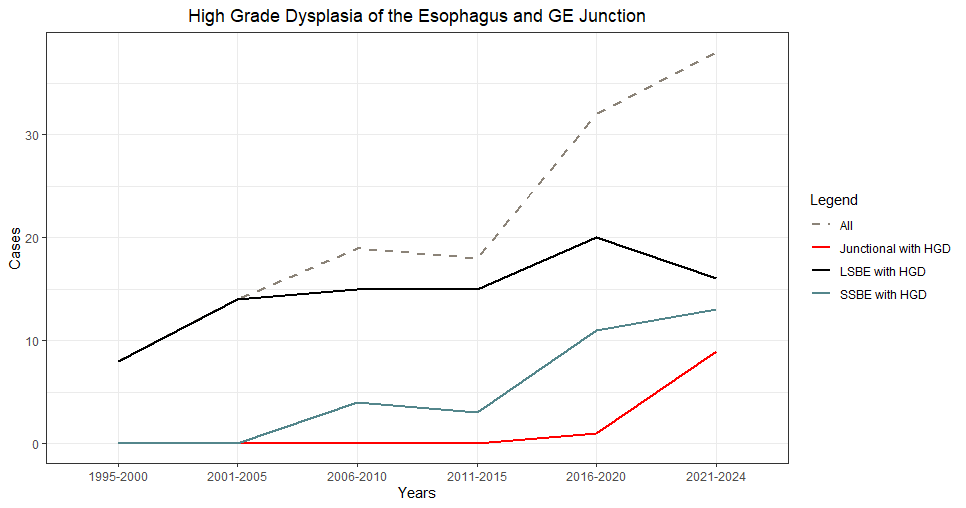
Figure: Cases of High-Grade Dysplasia. Total case counts were aggregated every 5 years.

Figure: Examples of images classified as “Junctional Dysplasia” by blinded endoscopists. Each image represents a different individual.
Disclosures:
Nicholas Catanzaro indicated no relevant financial relationships.
Rajesh Gupta indicated no relevant financial relationships.
Andrew Catanzaro indicated no relevant financial relationships.
Ashley Faulx: Steris – Consultant.
Wendy Brock indicated no relevant financial relationships.
Beth Bednarchik indicated no relevant financial relationships.
Joseph Willis: Lucid Diagnostics – Consultant, Intellectual Property/Patents, Royalties.
Amitabh Chak: Lucid Dx – Consultant, Grant/Research Support, Intellectual Property/Patents, Royalties, Stock Options, Stock-publicly held company(excluding mutual/index funds). MicroTech – Consultant. Pentax – Consultant. Steris – Consultant.
Nicholas Catanzaro, BS1, Rajesh Gupta, MSN, MS1, Andrew Catanzaro, MD2, Ashley Faulx, MD2, Wendy Brock, BSN, RN2, Beth Bednarchik, BSN, RN3, Joseph Willis, MD3, Amitabh Chak, MD, FACG3. P0636 - Temporal Trends of High Grade Dysplasia in the Esophagus and GE Junction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
