Sunday Poster Session
Category: Esophagus
P0603 - Unmasking Esophageal Granular Cell Tumors: Clinical and Endoscopic Insights
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Qusai Al Zureikat, MD (he/him/his)
MedStar Health-Georgetown/Washington Hospital Center
Washington, DC
Presenting Author(s)
Qusai Al Zureikat, MD1, Ahmad Abdulraheem, MD2, Ahmad Al-Dwairy, MBBS3, Abdalla Khouqeer, MD3, Stephanie Woo, MD3, Roaa Aljuaid, MBBS3, Nadim Haddad, MD3, Walid Chalhoub, MD3
1MedStar Health-Georgetown/Washington Hospital Center, Washington, DC; 2MedStar Washington Hospital Center-Georgetown University, Washington, DC; 3MedStar Georgetown University Hospital, Washington, DC
Introduction: Esophageal granular cell tumors (EGCTs) are rare subepithelial neoplasms comprising less than 1% of all GCTs. Their variable presentations and histologic complexity pose diagnostic and management challenges. There are currently no established guidelines for the evaluation and treatment of EGCTs, leading to variability in clinical practice. This study aimed to describe the clinical features, diagnostic methods, and outcomes of patients with esophageal GCTs at a single center, with the goal of contributing to a more standardized approach to their management.
Methods: We conducted a retrospective review of 19 patients diagnosed with esophageal GCTs from January 2010 to November 2024. Data collected included demographics, clinical presentation, tumor characteristics, endoscopic and histologic findings, treatment approach, and outcomes.
Results: The mean age was 43 years, with a slight female predominance. Most lesions were incidentally found during evaluation for refractory gastroesophageal reflux disease (GERD) and were located in the lower esophagus. Endoscopic ultrasound (EUS) revealed hypoechoic submucosal nodules in 11 cases.
Conventional
Endoscopic mucosal resection (EMR) was the most common treatment (68.4%), followed by EMR with hot snare and cap-assisted EMR. One case was managed conservatively. No complications, recurrences, or malignant transformations were observed. Immunohistochemistry was available for 11 cases, all positive for S100, with CD68 and Inhibin positive in 36%.
Discussion: Esophageal granular cell tumors (EGCTs) are rare, typically benign neoplasms increasingly detected due to widespread endoscopy use. Most are incidental findings, often located in the mid to distal esophagus. Diagnosis relies on endoscopic appearance, EUS features, and confirmation via histology and immunohistochemistry (e.g., S-100 positivity). EMR is the preferred management for small, localized tumors, offering high rates of complete resection with minimal complications. In our series, all resected lesions were removed en bloc without recurrence. Cap-assisted and ligation-assisted EMR techniques were effective and safe. Notably, GERD symptoms were present in most patients, and a predominance of distal lesions raises the possibility of an association. Further studies are needed to clarify the clinical significance of this relationship and optimize management strategies.
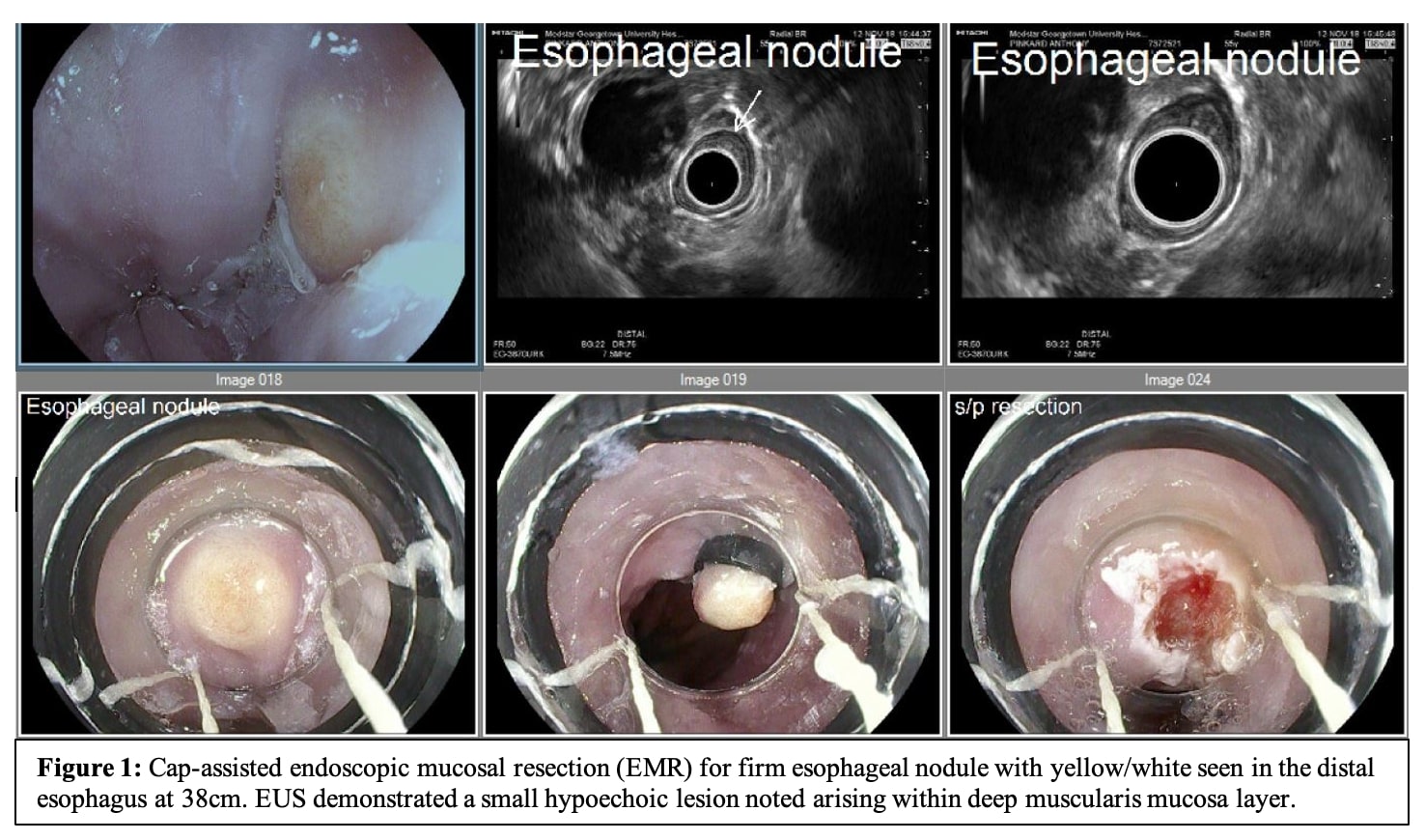
Figure: Figure 1: Cap-assisted endoscopic mucosal resection (EMR) for firm esophageal nodule with yellow/white seen in the distal esophagus at 38cm. EUS demonstrated a small hypoechoic lesion noted arising within deep muscularis mucosa layer.
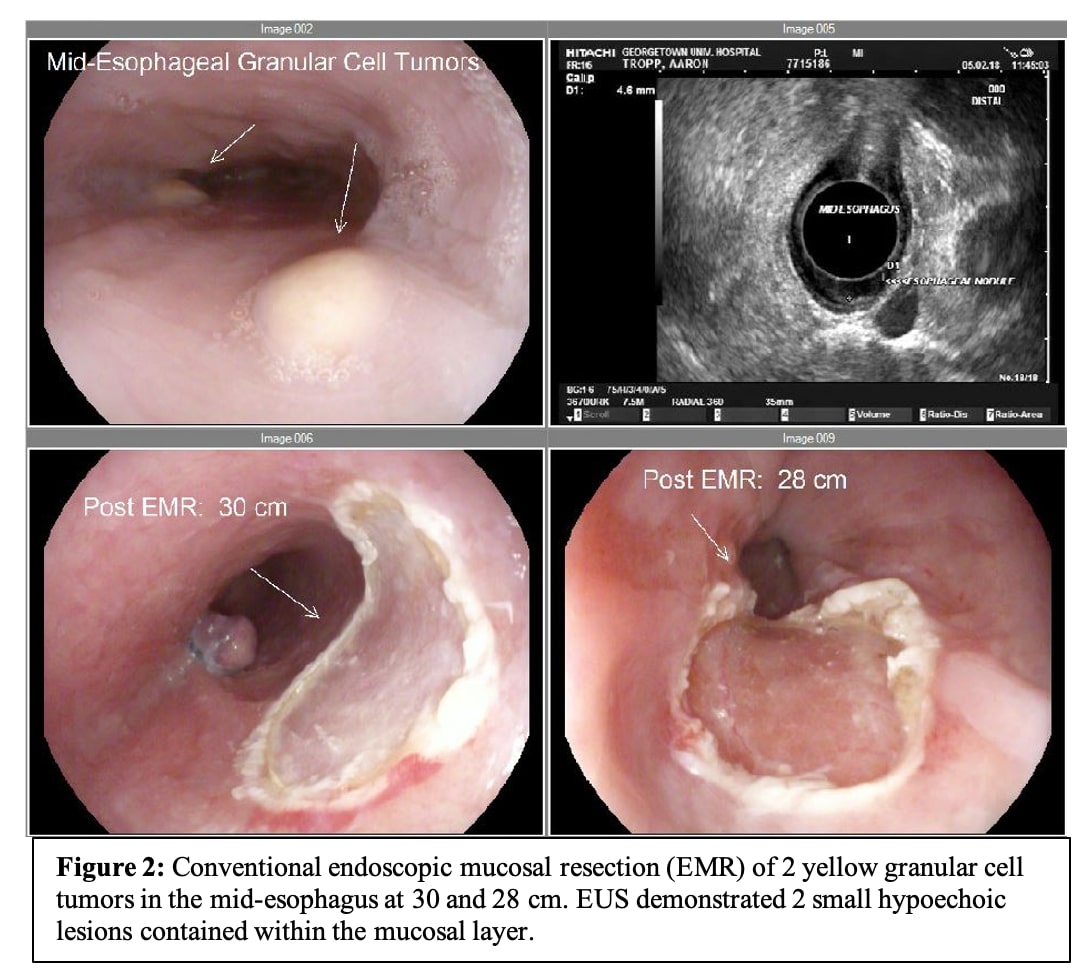
Figure: Figure 2: Conventional endoscopic mucosal resection (EMR) of 2 yellow granular cell tumors in the mid-esophagus at 30 and 28 cm. EUS demonstrated 2 small hypoechoic lesions contained within the mucosal layer.
Disclosures:
Qusai Al Zureikat indicated no relevant financial relationships.
Ahmad Abdulraheem indicated no relevant financial relationships.
Ahmad Al-Dwairy indicated no relevant financial relationships.
Abdalla Khouqeer indicated no relevant financial relationships.
Stephanie Woo indicated no relevant financial relationships.
Roaa Aljuaid indicated no relevant financial relationships.
Nadim Haddad indicated no relevant financial relationships.
Walid Chalhoub indicated no relevant financial relationships.
Qusai Al Zureikat, MD1, Ahmad Abdulraheem, MD2, Ahmad Al-Dwairy, MBBS3, Abdalla Khouqeer, MD3, Stephanie Woo, MD3, Roaa Aljuaid, MBBS3, Nadim Haddad, MD3, Walid Chalhoub, MD3. P0603 - Unmasking Esophageal Granular Cell Tumors: Clinical and Endoscopic Insights, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1MedStar Health-Georgetown/Washington Hospital Center, Washington, DC; 2MedStar Washington Hospital Center-Georgetown University, Washington, DC; 3MedStar Georgetown University Hospital, Washington, DC
Introduction: Esophageal granular cell tumors (EGCTs) are rare subepithelial neoplasms comprising less than 1% of all GCTs. Their variable presentations and histologic complexity pose diagnostic and management challenges. There are currently no established guidelines for the evaluation and treatment of EGCTs, leading to variability in clinical practice. This study aimed to describe the clinical features, diagnostic methods, and outcomes of patients with esophageal GCTs at a single center, with the goal of contributing to a more standardized approach to their management.
Methods: We conducted a retrospective review of 19 patients diagnosed with esophageal GCTs from January 2010 to November 2024. Data collected included demographics, clinical presentation, tumor characteristics, endoscopic and histologic findings, treatment approach, and outcomes.
Results: The mean age was 43 years, with a slight female predominance. Most lesions were incidentally found during evaluation for refractory gastroesophageal reflux disease (GERD) and were located in the lower esophagus. Endoscopic ultrasound (EUS) revealed hypoechoic submucosal nodules in 11 cases.
Conventional
Endoscopic mucosal resection (EMR) was the most common treatment (68.4%), followed by EMR with hot snare and cap-assisted EMR. One case was managed conservatively. No complications, recurrences, or malignant transformations were observed. Immunohistochemistry was available for 11 cases, all positive for S100, with CD68 and Inhibin positive in 36%.
Discussion: Esophageal granular cell tumors (EGCTs) are rare, typically benign neoplasms increasingly detected due to widespread endoscopy use. Most are incidental findings, often located in the mid to distal esophagus. Diagnosis relies on endoscopic appearance, EUS features, and confirmation via histology and immunohistochemistry (e.g., S-100 positivity). EMR is the preferred management for small, localized tumors, offering high rates of complete resection with minimal complications. In our series, all resected lesions were removed en bloc without recurrence. Cap-assisted and ligation-assisted EMR techniques were effective and safe. Notably, GERD symptoms were present in most patients, and a predominance of distal lesions raises the possibility of an association. Further studies are needed to clarify the clinical significance of this relationship and optimize management strategies.
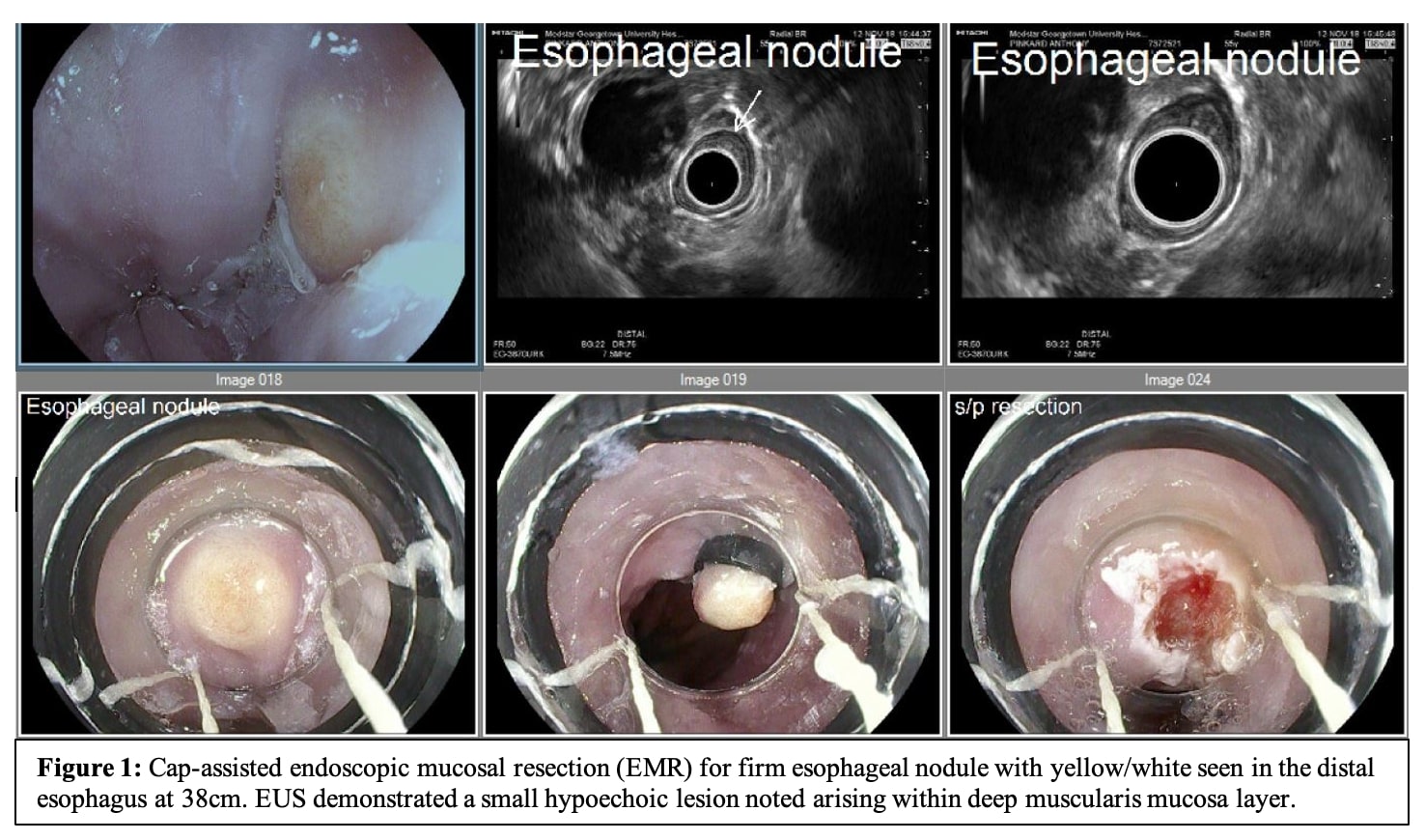
Figure: Figure 1: Cap-assisted endoscopic mucosal resection (EMR) for firm esophageal nodule with yellow/white seen in the distal esophagus at 38cm. EUS demonstrated a small hypoechoic lesion noted arising within deep muscularis mucosa layer.
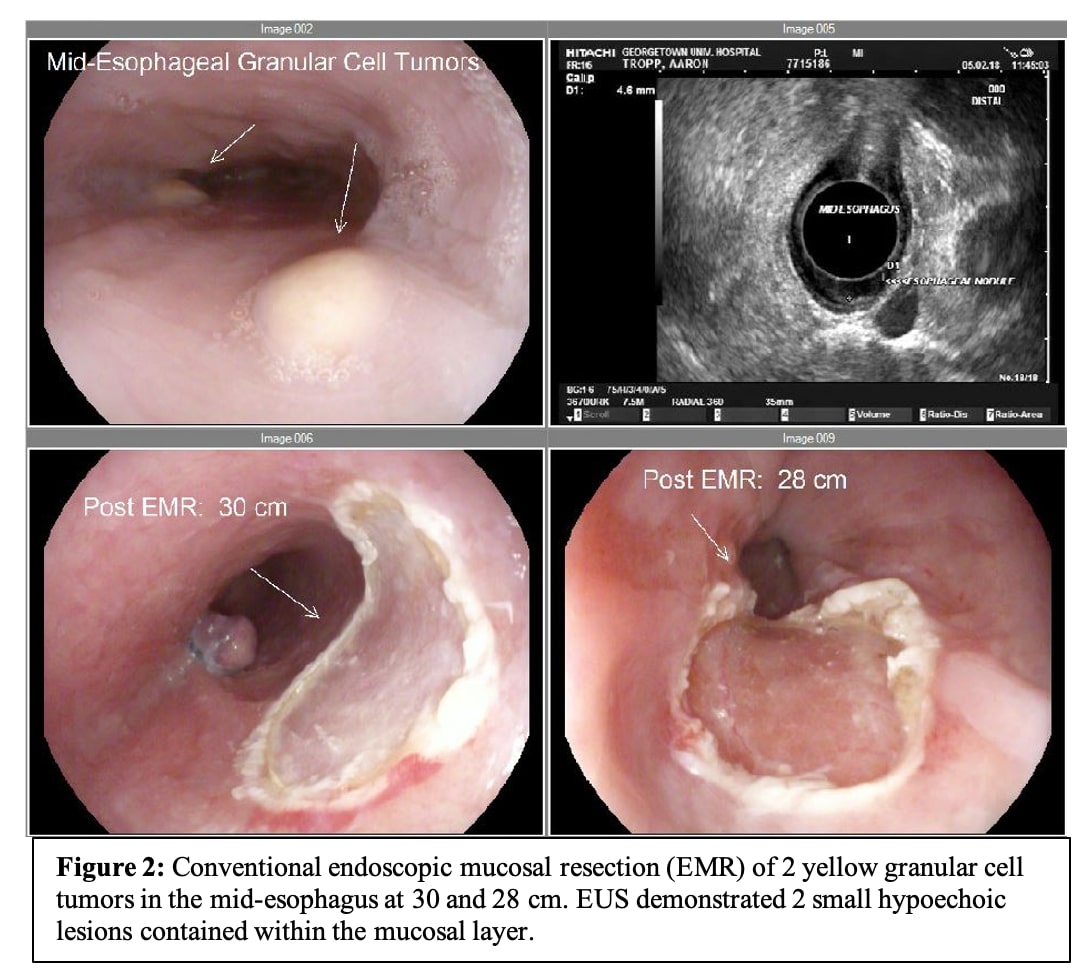
Figure: Figure 2: Conventional endoscopic mucosal resection (EMR) of 2 yellow granular cell tumors in the mid-esophagus at 30 and 28 cm. EUS demonstrated 2 small hypoechoic lesions contained within the mucosal layer.
Disclosures:
Qusai Al Zureikat indicated no relevant financial relationships.
Ahmad Abdulraheem indicated no relevant financial relationships.
Ahmad Al-Dwairy indicated no relevant financial relationships.
Abdalla Khouqeer indicated no relevant financial relationships.
Stephanie Woo indicated no relevant financial relationships.
Roaa Aljuaid indicated no relevant financial relationships.
Nadim Haddad indicated no relevant financial relationships.
Walid Chalhoub indicated no relevant financial relationships.
Qusai Al Zureikat, MD1, Ahmad Abdulraheem, MD2, Ahmad Al-Dwairy, MBBS3, Abdalla Khouqeer, MD3, Stephanie Woo, MD3, Roaa Aljuaid, MBBS3, Nadim Haddad, MD3, Walid Chalhoub, MD3. P0603 - Unmasking Esophageal Granular Cell Tumors: Clinical and Endoscopic Insights, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
