Sunday Poster Session
Category: Esophagus
P0600 - Case-Based Learning in Action: Enhancing Resident Knowledge of Achalasia and Eosinophilic Esophagitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ines Varela Knorr, MD
Mount Sinai West, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Ines Varela Knorr, MD1, Swati Patel, MD1, Daniela Jodorkovsky, MD2, Priya Simoes, MBBS2
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Variability in clinical rotations can lead to inconsistent subspecialty exposure for internal medicine residents, posing challenges for board exam preparation. To address this issue, we developed a targeted case-based curriculum to unify and enhance residents' understanding of high-yield gastroenterology (GI) topics frequently tested on the ABIM exam.
Methods: We conducted a 10-question needs assessment focused on 'High Importance' ABIM blueprint topics to evaluate resident familiarity with core GI subjects at a large internal medicine program. Of the 53 residents who completed this assessment, 77% (41/53) felt unfamiliar with upper gastrointestinal (GI) motility disorders, and 81% (43/53) with non-malignant esophageal disorders. Based on these results, we developed several case-based lectures designed to enhance familiarity with these topics (Figure 1). The session on non-malignant esophageal disorders focused on a case of eosinophilic esophagitis (EOE). While the session on upper GI motility disorders centered on the diagnosis and management of achalasia. Residents’ knowledge was assessed using pre- and post-session assessments. The post-learning assessment evaluated both objective knowledge gains as well as self reported level of comfort with the material.
Results: Before the session on EOE, 86% of interns (31/36) correctly answered an ABIM-style question on its diagnosis and management. At a five-month follow up all respondents (20/20) answered the question correctly, with 89% reporting feeling comfortable or very comfortable with the topic.
The session on diagnosis and management of achalasia was given to residents from all three years of training. 62% of residents (24/39) answered the pre-assessment correctly, improving to 85% (29/34) immediately post intervention. However, only 59% reported feeling comfortable or very comfortable with the material. At five-month follow-up, 73% (11/15) of PGY-2 and PGY-3 residents who had attended the original lecture retained correct answers. A comparable intern follow-up was not available, as their session occurred later and the five-month follow-up mark had not yet been reached.
Discussion: Case-based learning effectively addresses gaps from variable clinical exposure by enhancing immediate understanding. However, its impact may diminish over time without reinforcement, especially when learners report discomfort with the topic in the post- learning assessment. This study helps identify effective strategies to standardize resident knowledge.
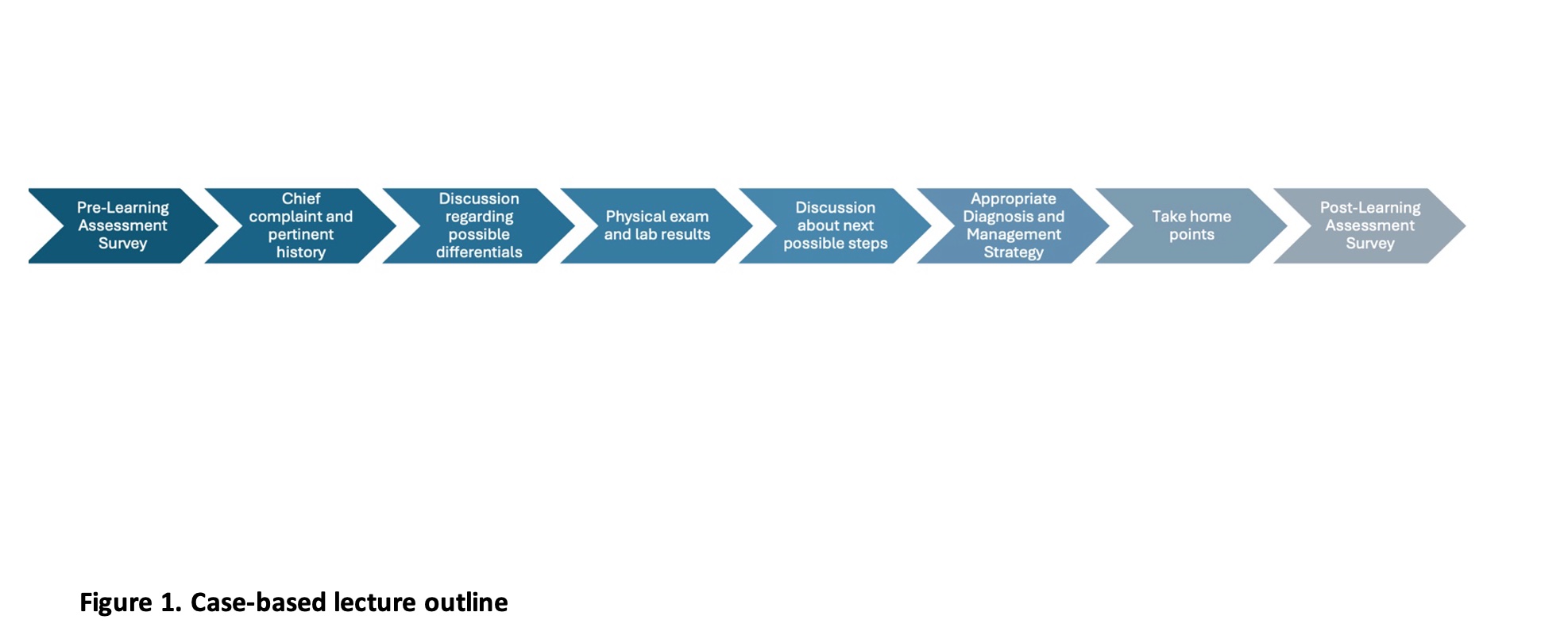
Figure: Figure 1: Case-based lecture outline
Disclosures:
Ines Varela Knorr indicated no relevant financial relationships.
Swati Patel indicated no relevant financial relationships.
Daniela Jodorkovsky indicated no relevant financial relationships.
Priya Simoes indicated no relevant financial relationships.
Ines Varela Knorr, MD1, Swati Patel, MD1, Daniela Jodorkovsky, MD2, Priya Simoes, MBBS2. P0600 - Case-Based Learning in Action: Enhancing Resident Knowledge of Achalasia and Eosinophilic Esophagitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Variability in clinical rotations can lead to inconsistent subspecialty exposure for internal medicine residents, posing challenges for board exam preparation. To address this issue, we developed a targeted case-based curriculum to unify and enhance residents' understanding of high-yield gastroenterology (GI) topics frequently tested on the ABIM exam.
Methods: We conducted a 10-question needs assessment focused on 'High Importance' ABIM blueprint topics to evaluate resident familiarity with core GI subjects at a large internal medicine program. Of the 53 residents who completed this assessment, 77% (41/53) felt unfamiliar with upper gastrointestinal (GI) motility disorders, and 81% (43/53) with non-malignant esophageal disorders. Based on these results, we developed several case-based lectures designed to enhance familiarity with these topics (Figure 1). The session on non-malignant esophageal disorders focused on a case of eosinophilic esophagitis (EOE). While the session on upper GI motility disorders centered on the diagnosis and management of achalasia. Residents’ knowledge was assessed using pre- and post-session assessments. The post-learning assessment evaluated both objective knowledge gains as well as self reported level of comfort with the material.
Results: Before the session on EOE, 86% of interns (31/36) correctly answered an ABIM-style question on its diagnosis and management. At a five-month follow up all respondents (20/20) answered the question correctly, with 89% reporting feeling comfortable or very comfortable with the topic.
The session on diagnosis and management of achalasia was given to residents from all three years of training. 62% of residents (24/39) answered the pre-assessment correctly, improving to 85% (29/34) immediately post intervention. However, only 59% reported feeling comfortable or very comfortable with the material. At five-month follow-up, 73% (11/15) of PGY-2 and PGY-3 residents who had attended the original lecture retained correct answers. A comparable intern follow-up was not available, as their session occurred later and the five-month follow-up mark had not yet been reached.
Discussion: Case-based learning effectively addresses gaps from variable clinical exposure by enhancing immediate understanding. However, its impact may diminish over time without reinforcement, especially when learners report discomfort with the topic in the post- learning assessment. This study helps identify effective strategies to standardize resident knowledge.
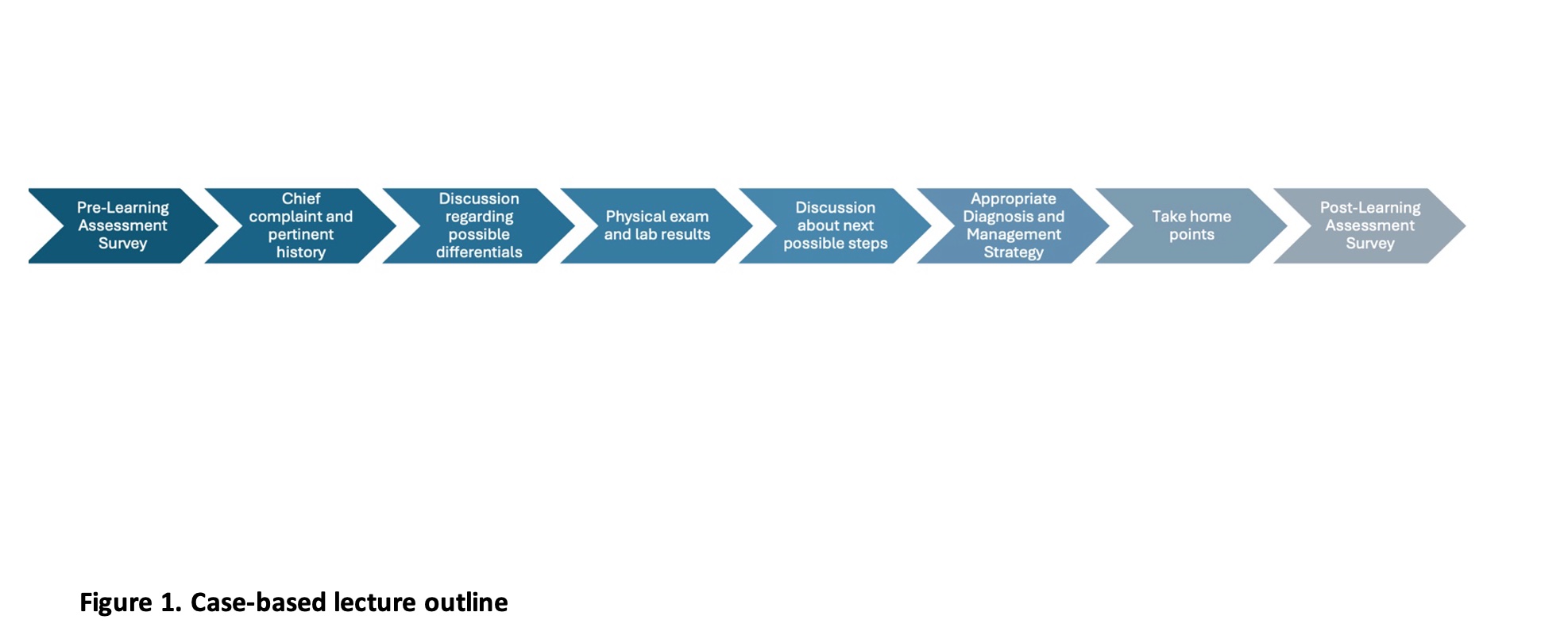
Figure: Figure 1: Case-based lecture outline
Disclosures:
Ines Varela Knorr indicated no relevant financial relationships.
Swati Patel indicated no relevant financial relationships.
Daniela Jodorkovsky indicated no relevant financial relationships.
Priya Simoes indicated no relevant financial relationships.
Ines Varela Knorr, MD1, Swati Patel, MD1, Daniela Jodorkovsky, MD2, Priya Simoes, MBBS2. P0600 - Case-Based Learning in Action: Enhancing Resident Knowledge of Achalasia and Eosinophilic Esophagitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
