Sunday Poster Session
Category: Esophagus
P0597 - Outcomes Following Esophageal Stenting With and Without Fixation - A Single-Center Characterization Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- KM
Karishma Mistry, MD
Rutgers Robert Wood Johnson University Hospital
New Brunswick, NJ
Presenting Author(s)
Karishma Mistry, MD1, Thomas Rees. Checketts, DO2, Omar Alaber, MD2, Alexander Hall, BS2, Saurabh Chandan, MD2, Kalyana Nandipati, MD2
1Rutgers Robert Wood Johnson University Hospital, New Brunswick, NJ; 2Creighton University, Omaha, NE
Introduction: Esophageal stents are placed endoscopically for various indications, including relieving obstruction from strictures and closing pathologic perforations or fistulae. Stents differ in material, pharmaceutical/radioactive properties, size, and expansion ability. Complications can occur after placement. Currently, there is little consensus on whether stents should be fixated. Our goal was to identify differences in outcomes (intended and adverse) after stent placement, and whether fixation (via suture, clip, or both) helps prevent restenosis, migration, or displacement compared to no fixation. This abstract focuses on fixation in strictures.
Methods: A retrospective analysis of Creighton University Medical Center patients was conducted on non-pregnant adult (19+) patients who underwent esophageal stenting for esophageal disease (obstruction, leaks, perforation, and fistulas) from January 1, 2013- April 1, 2023. Stents were placed by experienced gastroenterologists and esophageal surgeons. Stent characteristics and outcomes were stratified by use of fixation or not. Fixation modalities (table 1) included: endo-suturing, over the scope clips, standard hemostatic clips, flanges, and wing, Migration was confirmed during the next endoscope. Relief from dysphagia and retrosternal pain were assessed by follow-up notes of patient’s food tolerance, if weight was stable or increasing, and the absence of new pain not otherwise explained. Study outcomes were presented as frequency and percentage and compared using Chi-square tests.
Results: There were 192 patients (mean age 62, sd =14) included. Most stents were placed for malignant (n = 65, 34%) or benign (n = 58, 30%) strictures; other indications included leaks (n=35, 18%), perforations (n=16, 8%), and fistula (n=10, 5%). Of these 71 (37%) received some form of fixation; endo-suturing was most common (n=55) followed by hemostatic clips (n=12) (Table 1).
Discussion: A variety of esophageal stents were used, including covered (silicone or polyurethane), partially covered, uncovered, self-expandable metallic, and balloon-expandable stents. Covered stents were used in 176 (88%) cases. Comparing outcomes with and without fixation, there was no statistically significant difference in relief from dysphagia, hemorrhage, mortality, dysphagia recurrence, fistula formation, or perforation (Table 2). Notably, stent migration rates were identical with and without fixation (14% vs 14%, p = .987).
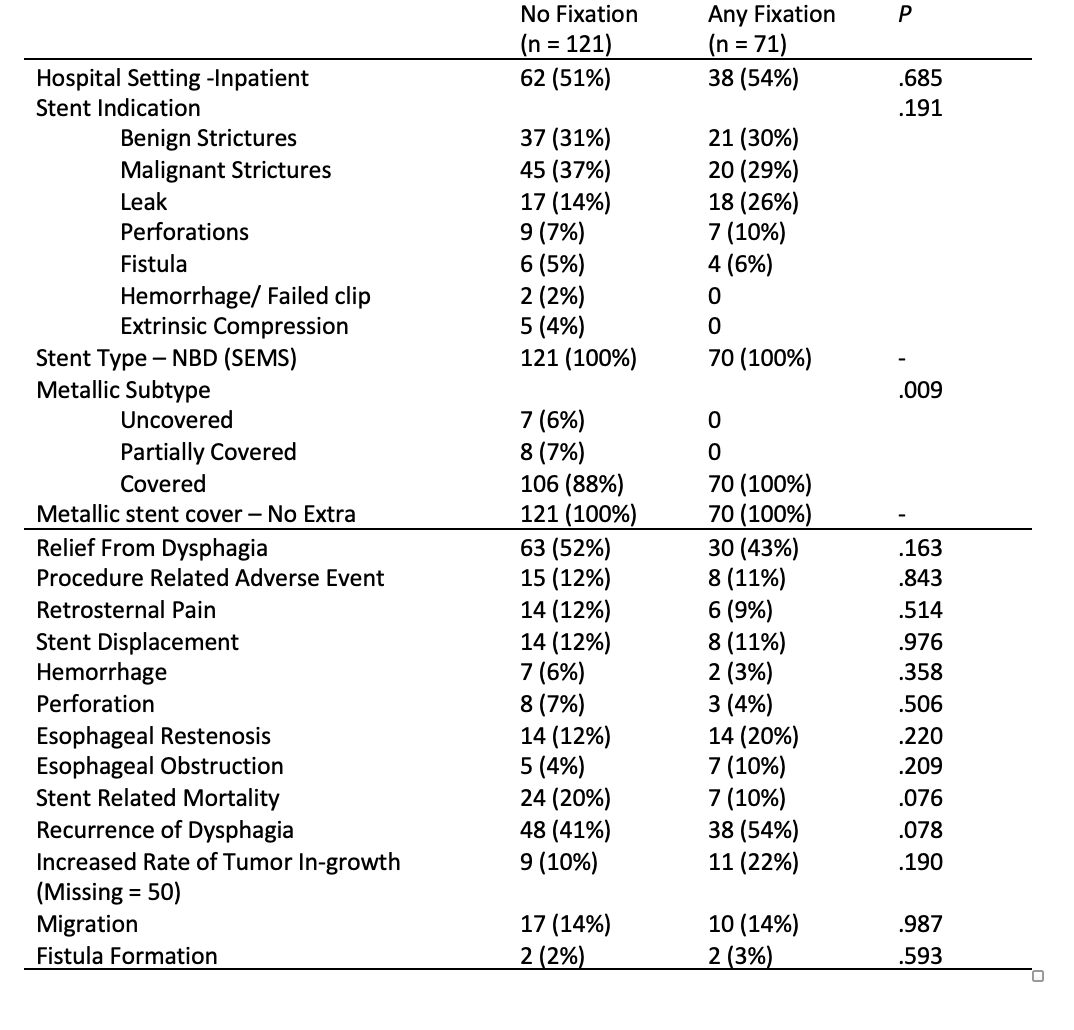
Figure: Fixation characteristics
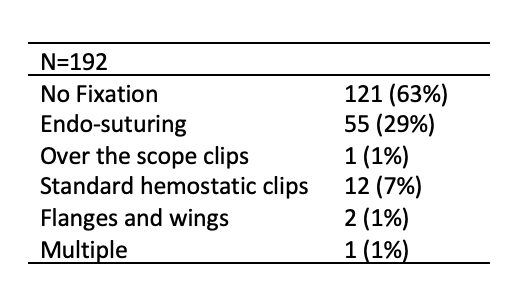
Figure: Adverse outcomes by fixation type
Disclosures:
Karishma Mistry indicated no relevant financial relationships.
Thomas Checketts indicated no relevant financial relationships.
Omar Alaber indicated no relevant financial relationships.
Alexander Hall indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Kalyana Nandipati indicated no relevant financial relationships.
Karishma Mistry, MD1, Thomas Rees. Checketts, DO2, Omar Alaber, MD2, Alexander Hall, BS2, Saurabh Chandan, MD2, Kalyana Nandipati, MD2. P0597 - Outcomes Following Esophageal Stenting With and Without Fixation - A Single-Center Characterization Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rutgers Robert Wood Johnson University Hospital, New Brunswick, NJ; 2Creighton University, Omaha, NE
Introduction: Esophageal stents are placed endoscopically for various indications, including relieving obstruction from strictures and closing pathologic perforations or fistulae. Stents differ in material, pharmaceutical/radioactive properties, size, and expansion ability. Complications can occur after placement. Currently, there is little consensus on whether stents should be fixated. Our goal was to identify differences in outcomes (intended and adverse) after stent placement, and whether fixation (via suture, clip, or both) helps prevent restenosis, migration, or displacement compared to no fixation. This abstract focuses on fixation in strictures.
Methods: A retrospective analysis of Creighton University Medical Center patients was conducted on non-pregnant adult (19+) patients who underwent esophageal stenting for esophageal disease (obstruction, leaks, perforation, and fistulas) from January 1, 2013- April 1, 2023. Stents were placed by experienced gastroenterologists and esophageal surgeons. Stent characteristics and outcomes were stratified by use of fixation or not. Fixation modalities (table 1) included: endo-suturing, over the scope clips, standard hemostatic clips, flanges, and wing, Migration was confirmed during the next endoscope. Relief from dysphagia and retrosternal pain were assessed by follow-up notes of patient’s food tolerance, if weight was stable or increasing, and the absence of new pain not otherwise explained. Study outcomes were presented as frequency and percentage and compared using Chi-square tests.
Results: There were 192 patients (mean age 62, sd =14) included. Most stents were placed for malignant (n = 65, 34%) or benign (n = 58, 30%) strictures; other indications included leaks (n=35, 18%), perforations (n=16, 8%), and fistula (n=10, 5%). Of these 71 (37%) received some form of fixation; endo-suturing was most common (n=55) followed by hemostatic clips (n=12) (Table 1).
Discussion: A variety of esophageal stents were used, including covered (silicone or polyurethane), partially covered, uncovered, self-expandable metallic, and balloon-expandable stents. Covered stents were used in 176 (88%) cases. Comparing outcomes with and without fixation, there was no statistically significant difference in relief from dysphagia, hemorrhage, mortality, dysphagia recurrence, fistula formation, or perforation (Table 2). Notably, stent migration rates were identical with and without fixation (14% vs 14%, p = .987).
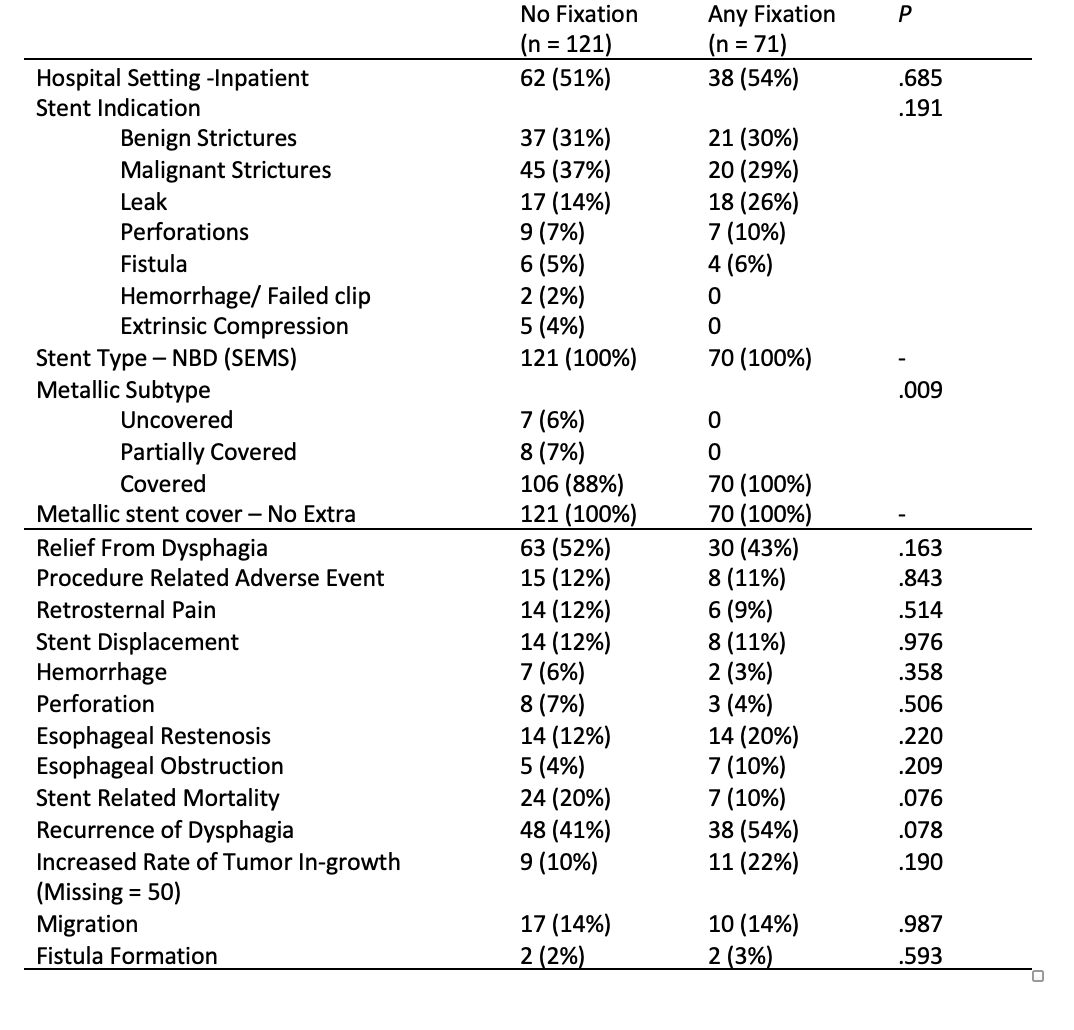
Figure: Fixation characteristics
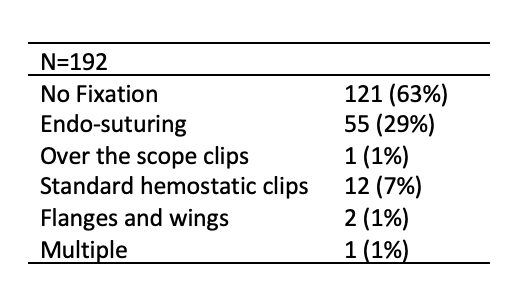
Figure: Adverse outcomes by fixation type
Disclosures:
Karishma Mistry indicated no relevant financial relationships.
Thomas Checketts indicated no relevant financial relationships.
Omar Alaber indicated no relevant financial relationships.
Alexander Hall indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Kalyana Nandipati indicated no relevant financial relationships.
Karishma Mistry, MD1, Thomas Rees. Checketts, DO2, Omar Alaber, MD2, Alexander Hall, BS2, Saurabh Chandan, MD2, Kalyana Nandipati, MD2. P0597 - Outcomes Following Esophageal Stenting With and Without Fixation - A Single-Center Characterization Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
