Sunday Poster Session
Category: Endoscopy Video Forum
P0584 - Novel Use of a Laparotomy Port Closure Device for Endoscopic Closure of a Persistent Gastrocutaneous Fistula
Xiang Yu Gao, BS (he/him/his)
Washington State University Elson S. Floyd School of Medicine
Spokane Valley, WA
Presenting Author(s)
1Washington State University Elson S. Floyd School of Medicine, Spokane Valley, WA; 2Washington State University Elson S. Floyd School of Medicine, Spokane, WA
Introduction:
Persistent gastrocutaneous fistula (GCF) is an uncommon adverse outcome of percutaneous endoscopic gastrostomy (PEG) tube placement. While most GCFs close spontaneously, a subset requires therapeutic interventions for closure. Conventionally, endoscopic closure with sutures, argon plasma coagulation, over-the-scope clips, or surgical closure are used for definitive therapy for persistent GCFs. We report a novel endoscopic adaptation of a laparoscopic port closure device for closure of a GCF that failed conventional endoscopic therapies.
Case Description/
Methods:
A 52-year-old female was referred for management of a persistent gastrocutaneous fistula (GCF) causing cutaneous maceration and drainage (Figure 1). She initially had a gastrostomy with a transgastric jejunal feeding tube placed for management of medication-refractory gastroparesis. The feeding tube was terminally removed but the GCF persisted necessitating multiple attempts at endoscopic closure with varying combinations of argon plasma coagulation (APC) of the margins, endoscopic suturing, an over-the-scope clip, and a combination of all three.
Due to the persistence of the GCF despite these interventions, a novel adaptation of the laparoscopic port closure device was used for endoscopic closure. An upper endoscopy with radiofrequency ablation of the margins was performed to prepare the tract for closure.
Using the laparoscopic port closure device, an introducer needle with a suture was passed transcutaneously into the gastric lumen under endoscopic visualization (Figure 2). Using a suture passer, the end of the previously placed suture was grasped within the gastric lumen, pulled across the gastrostomy tract and then out through the skin to tie a transgastric, transcutaneous knot. The suture was secured externally using the laparotomy port closure device. This resulted in complete closure of the GCF. Water insufflation testing demonstrated no leakage from the GCF. The patient tolerated the procedure well and recovered with no complications.
Discussion:
This case presents a successful closure of a persistent GCF using a novel endoscopic adaptation of a readily available laparoscopic port closure device. Given the persistence of the GCF despite multiple prior endoscopic interventions, the use of the port closure device may be an acceptable alternative to surgery in a subset of patients.
Figure: Figure 1. Visualization of the gastrocutaneous fistula from the skin aspect.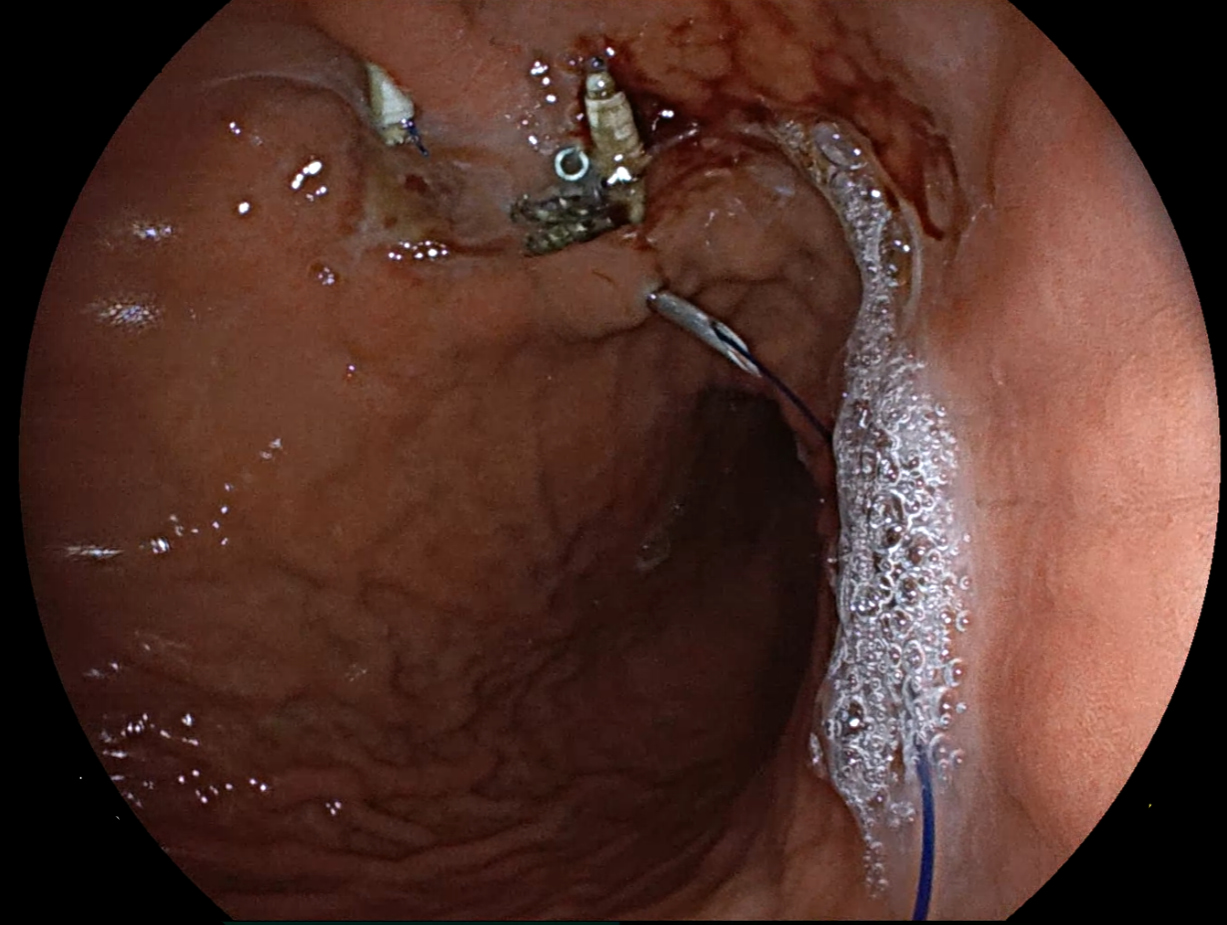
Figure: Figure 2. The transcutaneous and transgastric suture coursing through the laparotomy port closure device adjacent to the gastrocutaneous fistula.
Disclosures:
Xiang Yu Gao indicated no relevant financial relationships.
Divyanshoo Kohli: American Board of Internal Medicine – Advisory Committee/Board Member. Fujifilm – Grant/Research Support. Olympus Corporation of the Americas – Consultant.
Xiang Yu Gao, BS1, Divyanshoo Kohli, MD, FACG2. P0584 - Novel Use of a Laparotomy Port Closure Device for Endoscopic Closure of a Persistent Gastrocutaneous Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

