Sunday Poster Session
Category: Diet, Nutrition, and Obesity
P0568 - Vitamin A and Zinc Deficiencies Correlate with More Progressive Disease in Veterans with Advanced Liver Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Navila Sharif, MD
Emory University School of Medicine
Nashville, TN
Presenting Author(s)
Navila Sharif, MD1, Thuy-Van Hang, MD2
1Emory University School of Medicine, Nashville, TN; 2Emory University School of Medicine, Atlanta, GA
Introduction: Patients with advanced liver disease (ALD) should be assessed for vitamin and micronutrient deficiencies as malnutrition and sarcopenia are associated with mortality, worse outcomes with transplant, and overall complications. The 2021 American Association for the Study of Liver Diseases (AASLD) guidelines recommend at least annual screening, with more frequent checks in decompensated disease. There is minimal research on the degree of nutritional deficiencies and targets for supplementation. Our study aims to identify correlations between the presence of certain deficiencies and the severity of liver disease.
Methods: This is a single center, retrospective study evaluating vitamin and micronutrient deficiencies in Veterans with ALD seen at the Atlanta Veterans Affairs Liver Clinics from 11/1/2022 to 10/31/2024. Patients older than 18 years old, with a diagnosis of cirrhosis or advanced fibrosis, and at least 3 vitamins or micronutrients of interest checked within 12 months of the clinic visit, were included. Demographic data and liver disease history was obtained, along with levels of vitamin A, D, E, K, B1, B6, B9, B12, and C; zinc, selenium, copper, and iron. Statistical analysis was performed using Chi-square tests and T-tests, as appropriate.
Results: Of 106 patients included, the average age was 64 years old, and 51% had a BMI greater than 30. The most common deficiencies were vitamins A (47%), D (50%), C (26.8%), and zinc (28%). A higher MELD 3.0 score correlated with deficiencies in vitamins A, E, B1, zinc, selenium, and iron. Patients with vitamins A, B1, B9 and zinc deficiencies were more likely to have had a hospitalization in the past 12 months related to cirrhosis. Similarly, vitamins A, E, B9 and zinc deficiencies were significantly associated with decompensated cirrhosis.
Discussion: Vitamin A and zinc deficiencies were associated with higher MELD 3.0 score, higher Child-Pugh score, recent hospitalization linked to cirrhosis, decompensation, clinically significant portal hypertension, ascites, history of large volume paracentesis, diuretic use, and higher grade esophageal varices. While vitamin D deficiency was very common, there were no significant correlations with cirrhosis features or decompensation markers. Our study highlights the importance of screening for vitamin and micronutrient deficiencies. In particular, vitamin A and zinc may play key roles in end stage liver disease. Further studies are needed to determine longitudinal outcomes with supplementation.
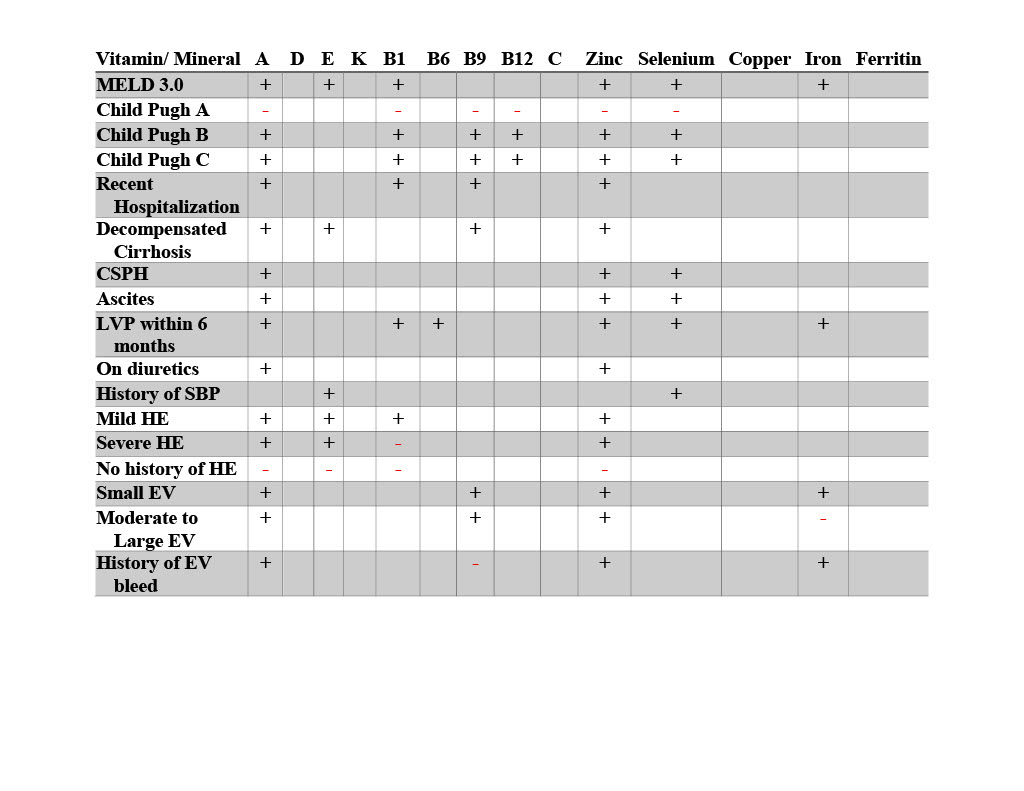
Figure: Correlation Between Vitamin and Mineral Deficiencies and Markers of Liver Disease
Only statistically significant relationships (p≤ 0.05) are labeled, with + meaning positive correlation, and – meaning negative correlation for the vitamin/ mineral deficiency.
Clinically significant portal hypertension (CSPH), esophageal varices (EV), hepatic encephalopathy (HE), large volume paracentesis (LVP), spontaneous bacterial peritonitis (SBP)
Disclosures:
Navila Sharif indicated no relevant financial relationships.
Thuy-Van Hang indicated no relevant financial relationships.
Navila Sharif, MD1, Thuy-Van Hang, MD2. P0568 - Vitamin A and Zinc Deficiencies Correlate with More Progressive Disease in Veterans with Advanced Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Emory University School of Medicine, Nashville, TN; 2Emory University School of Medicine, Atlanta, GA
Introduction: Patients with advanced liver disease (ALD) should be assessed for vitamin and micronutrient deficiencies as malnutrition and sarcopenia are associated with mortality, worse outcomes with transplant, and overall complications. The 2021 American Association for the Study of Liver Diseases (AASLD) guidelines recommend at least annual screening, with more frequent checks in decompensated disease. There is minimal research on the degree of nutritional deficiencies and targets for supplementation. Our study aims to identify correlations between the presence of certain deficiencies and the severity of liver disease.
Methods: This is a single center, retrospective study evaluating vitamin and micronutrient deficiencies in Veterans with ALD seen at the Atlanta Veterans Affairs Liver Clinics from 11/1/2022 to 10/31/2024. Patients older than 18 years old, with a diagnosis of cirrhosis or advanced fibrosis, and at least 3 vitamins or micronutrients of interest checked within 12 months of the clinic visit, were included. Demographic data and liver disease history was obtained, along with levels of vitamin A, D, E, K, B1, B6, B9, B12, and C; zinc, selenium, copper, and iron. Statistical analysis was performed using Chi-square tests and T-tests, as appropriate.
Results: Of 106 patients included, the average age was 64 years old, and 51% had a BMI greater than 30. The most common deficiencies were vitamins A (47%), D (50%), C (26.8%), and zinc (28%). A higher MELD 3.0 score correlated with deficiencies in vitamins A, E, B1, zinc, selenium, and iron. Patients with vitamins A, B1, B9 and zinc deficiencies were more likely to have had a hospitalization in the past 12 months related to cirrhosis. Similarly, vitamins A, E, B9 and zinc deficiencies were significantly associated with decompensated cirrhosis.
Discussion: Vitamin A and zinc deficiencies were associated with higher MELD 3.0 score, higher Child-Pugh score, recent hospitalization linked to cirrhosis, decompensation, clinically significant portal hypertension, ascites, history of large volume paracentesis, diuretic use, and higher grade esophageal varices. While vitamin D deficiency was very common, there were no significant correlations with cirrhosis features or decompensation markers. Our study highlights the importance of screening for vitamin and micronutrient deficiencies. In particular, vitamin A and zinc may play key roles in end stage liver disease. Further studies are needed to determine longitudinal outcomes with supplementation.
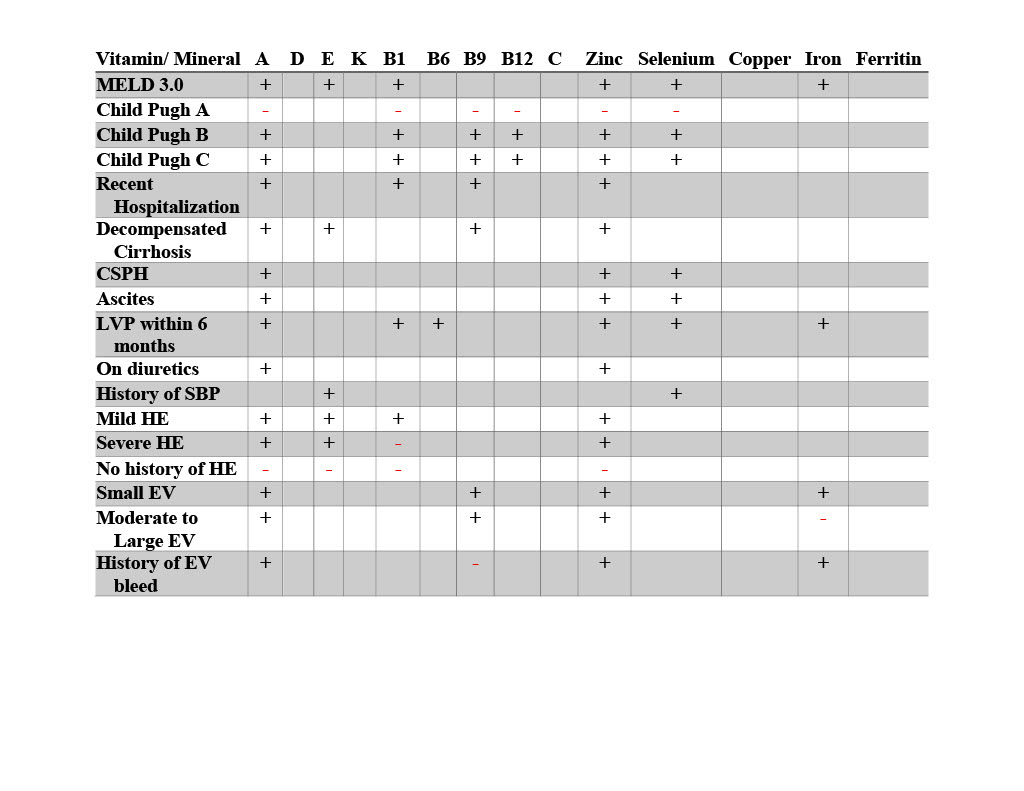
Figure: Correlation Between Vitamin and Mineral Deficiencies and Markers of Liver Disease
Only statistically significant relationships (p≤ 0.05) are labeled, with + meaning positive correlation, and – meaning negative correlation for the vitamin/ mineral deficiency.
Clinically significant portal hypertension (CSPH), esophageal varices (EV), hepatic encephalopathy (HE), large volume paracentesis (LVP), spontaneous bacterial peritonitis (SBP)
Disclosures:
Navila Sharif indicated no relevant financial relationships.
Thuy-Van Hang indicated no relevant financial relationships.
Navila Sharif, MD1, Thuy-Van Hang, MD2. P0568 - Vitamin A and Zinc Deficiencies Correlate with More Progressive Disease in Veterans with Advanced Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

