Sunday Poster Session
Category: Diet, Nutrition, and Obesity
P0563 - Underutilization and Racial Disparities in Obesity Management in the United States
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Abdellatif Ismail, MD
University of Maryland
Baltimore, MD
Presenting Author(s)
Abdellatif Ismail, MD1, Mohammed Al-Aquily, MD2, Mohammad Kloub, MD3, Khalid Ahmed, MD4, Monzer Abdalla, MD5, Mohamed Abdallah, MD6, Mohammad Bilal, MD, FACG7
1University of Maryland, Baltimore, MD; 2Norwalk Hospital/Yale University, Norwalk, CT; 3New York Medical College - Saint Michael's Medical Center, Bloomfield, NJ; 4University of Minnesota, Minneapolis, MN; 5Rosalind Franklin University of Medicine and Science, Evanston, IL; 6Corewell Health, Royal Oak, MI; 7University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Obesity is a prevalent health problem in the United States with significant racial disparities in both the prevalence and access to treatment. Bariatric surgery & glucagon-like peptide-1 receptor agonists (GLP-1RAs) are two of the most effective interventions for obesity & their utilization across racial groups is not well studied. This study aims to evaluate disparities in access to bariatric surgery & GLP-1RA medications based on race and gender.
Methods: We conducted a retrospective study using data from the TriNetX US Collaborative Network, which includes electronic health records from 61 healthcare organizations. We included patients with severe obesity defined as body mass index (BMI) ≥40 kg/m². Patients were divided into two cohorts: Cohort 1 included African American (AA) adult patients, while Cohort 2 included Caucasian adult patients. Separate analyses were conducted for males & females. Outcomes were measured over a 10-year period and included undergoing bariatric surgery and the use of GLP-1RA medications (semaglutide, liraglutide & tirzepatide). Propensity score matching was used to balance cohorts according to age, comorbidities, and BMI.
Results: AA males had significantly lower rates of bariatric surgery (1.1% vs 1.4%, RR: 0.79, p< 0.001) & GLP-1RA utilization compared to Caucasian males (5.6% vs 6.7%, RR: 0.84, p< 0.001). No significant difference was observed between AA & Caucasian females (2.5% vs 2.4%, RR: 1.01, p=0.508) in access to bariatric surgery, while utilization of GLP-1RA was slightly lower in AA females (6.2% vs 6.6%, RR: 0.94, p< 0.001). Furthermore, both types of obesity treatment were underutilized overall, specifically in adult males.
Discussion: Racial disparities in access to surgical and pharmacological obesity treatments are more prevalent among male populations (AA vs. Caucasian) compared to females. AA males were less likely to receive bariatric surgery and GLP-1RA medications. Moreover, obesity treatments remain largely underutilized in the population as a whole, and this is more pronounced in males compared to females. Targeted strategies are needed to ensure equitable access and removal of barriers to treatment across different patient groups.
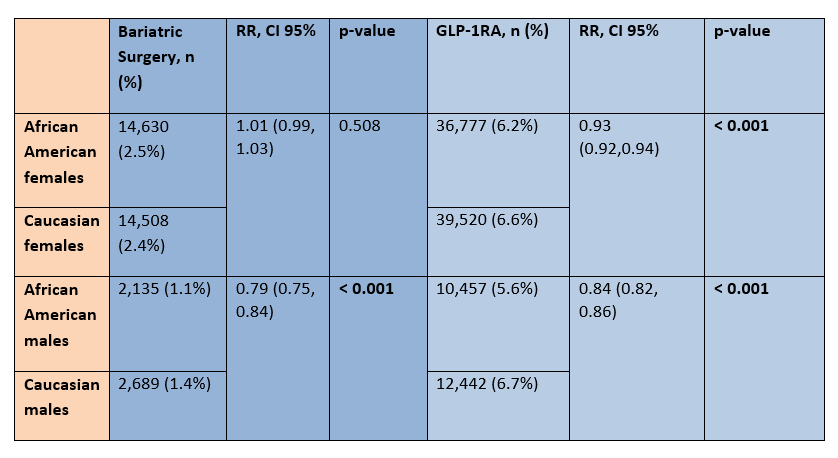
Figure: Table 1: Shows the racial differences between African American females and males vs Caucasian females and males, respectively, in regards to access to bariatric surgery and GLP-1RA medications.
Disclosures:
Abdellatif Ismail indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Mohammad Kloub indicated no relevant financial relationships.
Khalid Ahmed indicated no relevant financial relationships.
Monzer Abdalla indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Abdellatif Ismail, MD1, Mohammed Al-Aquily, MD2, Mohammad Kloub, MD3, Khalid Ahmed, MD4, Monzer Abdalla, MD5, Mohamed Abdallah, MD6, Mohammad Bilal, MD, FACG7. P0563 - Underutilization and Racial Disparities in Obesity Management in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Maryland, Baltimore, MD; 2Norwalk Hospital/Yale University, Norwalk, CT; 3New York Medical College - Saint Michael's Medical Center, Bloomfield, NJ; 4University of Minnesota, Minneapolis, MN; 5Rosalind Franklin University of Medicine and Science, Evanston, IL; 6Corewell Health, Royal Oak, MI; 7University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Obesity is a prevalent health problem in the United States with significant racial disparities in both the prevalence and access to treatment. Bariatric surgery & glucagon-like peptide-1 receptor agonists (GLP-1RAs) are two of the most effective interventions for obesity & their utilization across racial groups is not well studied. This study aims to evaluate disparities in access to bariatric surgery & GLP-1RA medications based on race and gender.
Methods: We conducted a retrospective study using data from the TriNetX US Collaborative Network, which includes electronic health records from 61 healthcare organizations. We included patients with severe obesity defined as body mass index (BMI) ≥40 kg/m². Patients were divided into two cohorts: Cohort 1 included African American (AA) adult patients, while Cohort 2 included Caucasian adult patients. Separate analyses were conducted for males & females. Outcomes were measured over a 10-year period and included undergoing bariatric surgery and the use of GLP-1RA medications (semaglutide, liraglutide & tirzepatide). Propensity score matching was used to balance cohorts according to age, comorbidities, and BMI.
Results: AA males had significantly lower rates of bariatric surgery (1.1% vs 1.4%, RR: 0.79, p< 0.001) & GLP-1RA utilization compared to Caucasian males (5.6% vs 6.7%, RR: 0.84, p< 0.001). No significant difference was observed between AA & Caucasian females (2.5% vs 2.4%, RR: 1.01, p=0.508) in access to bariatric surgery, while utilization of GLP-1RA was slightly lower in AA females (6.2% vs 6.6%, RR: 0.94, p< 0.001). Furthermore, both types of obesity treatment were underutilized overall, specifically in adult males.
Discussion: Racial disparities in access to surgical and pharmacological obesity treatments are more prevalent among male populations (AA vs. Caucasian) compared to females. AA males were less likely to receive bariatric surgery and GLP-1RA medications. Moreover, obesity treatments remain largely underutilized in the population as a whole, and this is more pronounced in males compared to females. Targeted strategies are needed to ensure equitable access and removal of barriers to treatment across different patient groups.
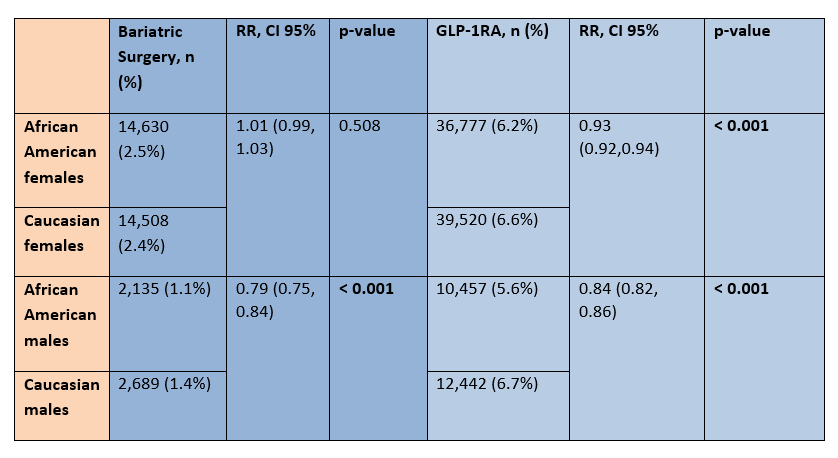
Figure: Table 1: Shows the racial differences between African American females and males vs Caucasian females and males, respectively, in regards to access to bariatric surgery and GLP-1RA medications.
Disclosures:
Abdellatif Ismail indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Mohammad Kloub indicated no relevant financial relationships.
Khalid Ahmed indicated no relevant financial relationships.
Monzer Abdalla indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Abdellatif Ismail, MD1, Mohammed Al-Aquily, MD2, Mohammad Kloub, MD3, Khalid Ahmed, MD4, Monzer Abdalla, MD5, Mohamed Abdallah, MD6, Mohammad Bilal, MD, FACG7. P0563 - Underutilization and Racial Disparities in Obesity Management in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

