Sunday Poster Session
Category: Diet, Nutrition, and Obesity
P0548 - Evaluating Surgical, Radiologic and Endoscopic PEG Tube Outcomes: A National Inpatient Sample Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Arvind Bussetty, MD (he/him/his)
Rutgers Robert Wood Johnson Medical School
New Brunswick, NJ
Presenting Author(s)
Arvind Bussetty, MD, Bhargav Vemulapalli, BS, Keerthana Kesavarapu, MD
Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Gastrostomy and enterostomy tubes provide nutritional support for patients with impaired oral intake. Common placement approaches including endoscopic (PEG), surgical (SG), and radiology-guided (PRG). The choice of approach should consider the patient factors and weighing risks and benefits. This study aims to compare PEG with SG and PRG, with a focus on their association with patient frailty and clinical outcomes.
Methods: Data were collected on patients with primary PEG, SG or PRG from the National Inpatient Sample database (NIS) from 2015–2020. Patients with PEG reintervention during the same hospitalization were excluded. Based on the Hospital Frailty Risk Score (HFRS), patients were categorized as low (HFRS < 5), intermediate (HFRS 5–15), or high frailty (HFRS > 15). Multivariable linear regression analyzed the relationship between PEG approach and HFRS. Logistic regression assessed mortality in HFRS patients. Linear regression examined associations with length of stay (LOS) and hospitalization charges.
Results: 393000 (32.0%) patients received PEG, 78190 (6.37%) received SG, and 756960 (61.63%) received PRG. Compared to PEG, SG was associated with a lower HFRS (β = -1.63; 95%CI: -1.69 to -1.57) while PRG was associated with a greater HFRS (β = 1.06; 95%CI: 1.06 to 1.14). Compared to PEG, there was a decreased mortality in SG (aOR = 0.74, CI: 0.65 to 0.84) and PRG (aOR = 0.37; 95%CI: 0.35 to 0.39) in the high HFRS cohort. Additionally, compared to PEG in the high HFRS cohort, SG had increased LOS (β = 5.96; 95% CI: 4.92–7.01) and hospitalization charges (β = 120830.05; 95% CI: 108884.24–132775.86), while PRG was also associated with increased LOS (β = 5.60; 95% CI: 5.26–5.94) and hospitalization charges (β = 83177.49; 95% CI: 79680.93–86674.05).
Discussion: In this large cohort study, feeding tube approach was significantly associated with frailty status. SG linked to lower frailty and PRG to higher frailty compared to endoscopic PEG placement. Among patients with high frailty (HFRS > 15), both SG and PRG demonstrated reduced mortality compared to PEG. However, SG and PRG were associated with longer hospital stays and higher hospitalization charges in this population. These findings highlight the influence of procedural approach and patient frailty on outcomes, underscoring the importance of individualized decision-making in PEG placement.
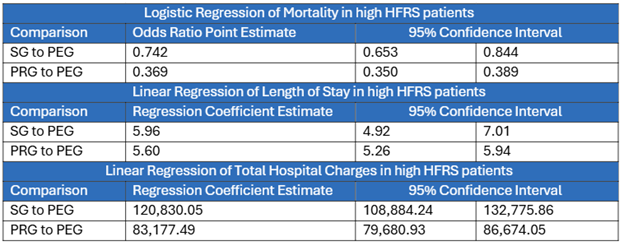
Figure: Logistic and Linear Regression Analysis Comparing Mortality, Total Hospital Charges and LOS between PEG to SG and PRG
Disclosures:
Arvind Bussetty indicated no relevant financial relationships.
Bhargav Vemulapalli indicated no relevant financial relationships.
Keerthana Kesavarapu indicated no relevant financial relationships.
Arvind Bussetty, MD, Bhargav Vemulapalli, BS, Keerthana Kesavarapu, MD. P0548 - Evaluating Surgical, Radiologic and Endoscopic PEG Tube Outcomes: A National Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Gastrostomy and enterostomy tubes provide nutritional support for patients with impaired oral intake. Common placement approaches including endoscopic (PEG), surgical (SG), and radiology-guided (PRG). The choice of approach should consider the patient factors and weighing risks and benefits. This study aims to compare PEG with SG and PRG, with a focus on their association with patient frailty and clinical outcomes.
Methods: Data were collected on patients with primary PEG, SG or PRG from the National Inpatient Sample database (NIS) from 2015–2020. Patients with PEG reintervention during the same hospitalization were excluded. Based on the Hospital Frailty Risk Score (HFRS), patients were categorized as low (HFRS < 5), intermediate (HFRS 5–15), or high frailty (HFRS > 15). Multivariable linear regression analyzed the relationship between PEG approach and HFRS. Logistic regression assessed mortality in HFRS patients. Linear regression examined associations with length of stay (LOS) and hospitalization charges.
Results: 393000 (32.0%) patients received PEG, 78190 (6.37%) received SG, and 756960 (61.63%) received PRG. Compared to PEG, SG was associated with a lower HFRS (β = -1.63; 95%CI: -1.69 to -1.57) while PRG was associated with a greater HFRS (β = 1.06; 95%CI: 1.06 to 1.14). Compared to PEG, there was a decreased mortality in SG (aOR = 0.74, CI: 0.65 to 0.84) and PRG (aOR = 0.37; 95%CI: 0.35 to 0.39) in the high HFRS cohort. Additionally, compared to PEG in the high HFRS cohort, SG had increased LOS (β = 5.96; 95% CI: 4.92–7.01) and hospitalization charges (β = 120830.05; 95% CI: 108884.24–132775.86), while PRG was also associated with increased LOS (β = 5.60; 95% CI: 5.26–5.94) and hospitalization charges (β = 83177.49; 95% CI: 79680.93–86674.05).
Discussion: In this large cohort study, feeding tube approach was significantly associated with frailty status. SG linked to lower frailty and PRG to higher frailty compared to endoscopic PEG placement. Among patients with high frailty (HFRS > 15), both SG and PRG demonstrated reduced mortality compared to PEG. However, SG and PRG were associated with longer hospital stays and higher hospitalization charges in this population. These findings highlight the influence of procedural approach and patient frailty on outcomes, underscoring the importance of individualized decision-making in PEG placement.
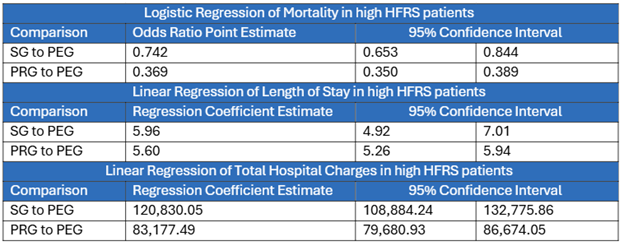
Figure: Logistic and Linear Regression Analysis Comparing Mortality, Total Hospital Charges and LOS between PEG to SG and PRG
Disclosures:
Arvind Bussetty indicated no relevant financial relationships.
Bhargav Vemulapalli indicated no relevant financial relationships.
Keerthana Kesavarapu indicated no relevant financial relationships.
Arvind Bussetty, MD, Bhargav Vemulapalli, BS, Keerthana Kesavarapu, MD. P0548 - Evaluating Surgical, Radiologic and Endoscopic PEG Tube Outcomes: A National Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

