Sunday Poster Session
Category: Colorectal Cancer Prevention
P0522 - Evaluating Real-World Performance of the Family Health History Tool for Identifying Individuals With Colorectal Neoplasia on Colonoscopy
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AZ
Aleksandra Zarska, BS
University of Michigan Medical School
Ann Arbor, MI
Presenting Author(s)
Aleksandra Zarska, BS1, Erika Koeppe, MS2, Anudeep Mukkamala, MD2, Joshua Smith, MD2, Elena Stoffel, MD, MPH2
1University of Michigan Medical School, Ann Arbor, MI; 2Michigan Medicine, Ann Arbor, MI
Introduction: Recent guidelines expanded colorectal cancer (CRC) screening to all individuals aged 45 and older, adding 19 million people to the eligible screening pool. Given the limited availability of colonoscopies, prioritizing individuals at highest risk for neoplasia is critical, yet implementation of risk-based CRC screening has been haphazard. Here we assess the utility of the Family Health History Tool for predicting neoplastic findings on colonoscopy.
Methods: Patients aged 18 and older with an upcoming colonoscopy appointment at a large academic medical center were invited to complete an electronic Family Health History Tool (FHHT). The FHHT collects cancer history in first- and second-degree relatives and computes a PREMM5 risk model score. Based on self-report responses, patients were classified as increased risk for CRC (defined as PREMM≥ 2.5% and/or a first-degree relative with CRC) or average risk. Retrospective chart reviews were conducted for all patients at increased risk, along with a random, age-matched sample of those at average risk. Chi-square tests were used to assess the relationship between risk category and history of colorectal neoplasia (defined as adenoma, sessile serrated adenoma, or cancer) at the time of FHHT completion.
Results: 947 patients completed the FHHT between May 2023 and May 2025, 139 of whom were excluded due to inflammatory bowel disease or canceled appointment, resulting in a final sample size of 404 increased risk patients and 404 eligible age-matched average risk patients. 57.4% of average risk and 68.3% of increased risk patients had neoplasia. Of all patients aged < 50, 44.7% had neoplasia. Among the 103 patients aged < 50 classified as increased risk, 56 (54.4%) had neoplasia, compared to 36 out of 103 (35%) in the average-risk group (OR=2.2, p=0.005). Overall, patients classified as increased risk per the FHHT were more likely to have neoplasia (OR=1.6, p=0.001).
Discussion: Patients identified at increased risk for the development of CRC based on the FHHT had significantly higher rates of neoplasia. This finding was particularly notable in patients aged < 50, supporting the utility of using a structured family history screening tool for CRC risk stratification to optimize resource allocation for screening colonoscopy and prioritize those at highest risk for CRC. Future directions include enhancing our predictive model by integrating demographic, lifestyle, and clinical factors to improve individualized risk assessment and screening efficiency.
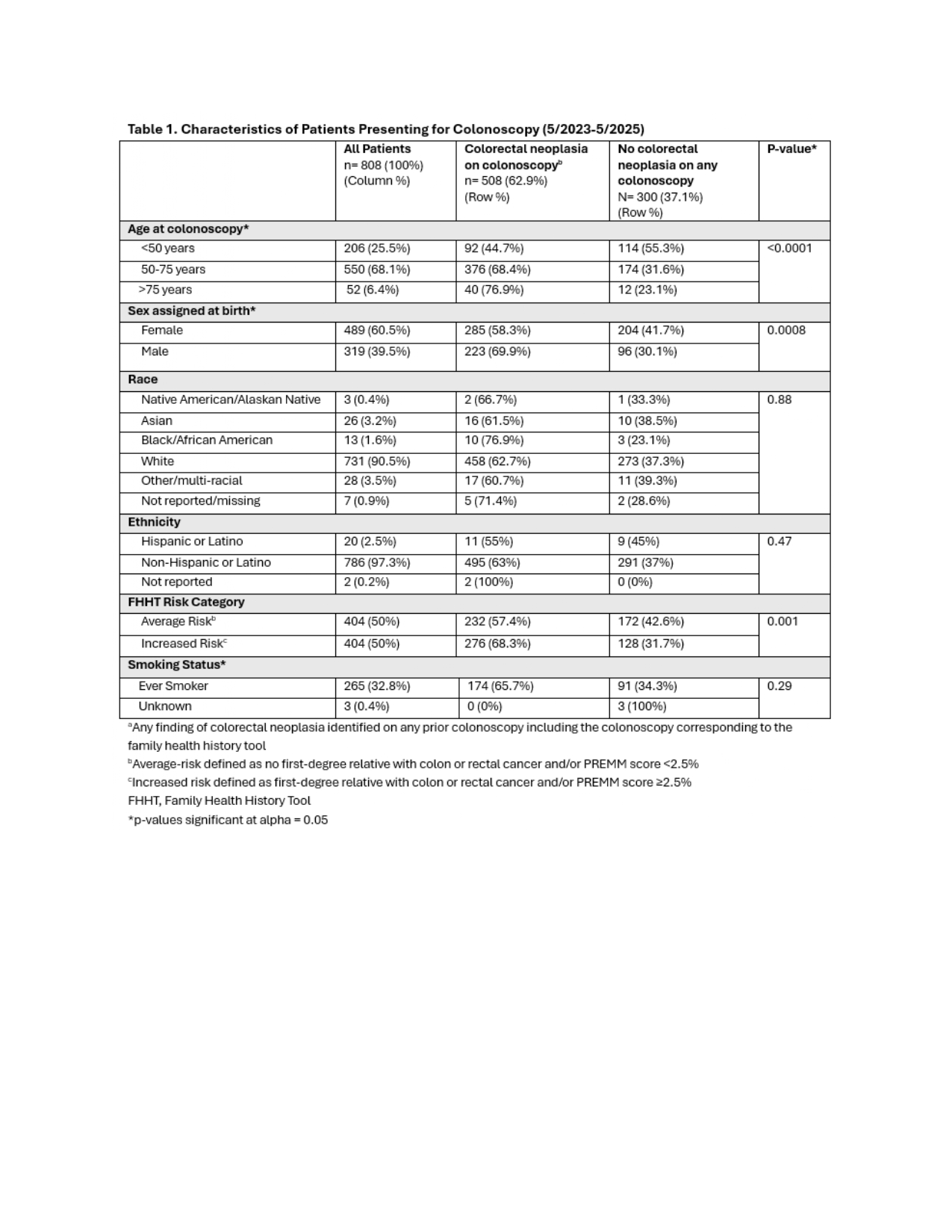
Figure: Demographics, risk stratification, and history of colorectal neoplasia of all patients presenting for colonoscopy between May 2023 and May 2025.
Disclosures:
Aleksandra Zarska indicated no relevant financial relationships.
Erika Koeppe indicated no relevant financial relationships.
Anudeep Mukkamala indicated no relevant financial relationships.
Joshua Smith indicated no relevant financial relationships.
Elena Stoffel indicated no relevant financial relationships.
Aleksandra Zarska, BS1, Erika Koeppe, MS2, Anudeep Mukkamala, MD2, Joshua Smith, MD2, Elena Stoffel, MD, MPH2. P0522 - Evaluating Real-World Performance of the Family Health History Tool for Identifying Individuals With Colorectal Neoplasia on Colonoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Michigan Medical School, Ann Arbor, MI; 2Michigan Medicine, Ann Arbor, MI
Introduction: Recent guidelines expanded colorectal cancer (CRC) screening to all individuals aged 45 and older, adding 19 million people to the eligible screening pool. Given the limited availability of colonoscopies, prioritizing individuals at highest risk for neoplasia is critical, yet implementation of risk-based CRC screening has been haphazard. Here we assess the utility of the Family Health History Tool for predicting neoplastic findings on colonoscopy.
Methods: Patients aged 18 and older with an upcoming colonoscopy appointment at a large academic medical center were invited to complete an electronic Family Health History Tool (FHHT). The FHHT collects cancer history in first- and second-degree relatives and computes a PREMM5 risk model score. Based on self-report responses, patients were classified as increased risk for CRC (defined as PREMM≥ 2.5% and/or a first-degree relative with CRC) or average risk. Retrospective chart reviews were conducted for all patients at increased risk, along with a random, age-matched sample of those at average risk. Chi-square tests were used to assess the relationship between risk category and history of colorectal neoplasia (defined as adenoma, sessile serrated adenoma, or cancer) at the time of FHHT completion.
Results: 947 patients completed the FHHT between May 2023 and May 2025, 139 of whom were excluded due to inflammatory bowel disease or canceled appointment, resulting in a final sample size of 404 increased risk patients and 404 eligible age-matched average risk patients. 57.4% of average risk and 68.3% of increased risk patients had neoplasia. Of all patients aged < 50, 44.7% had neoplasia. Among the 103 patients aged < 50 classified as increased risk, 56 (54.4%) had neoplasia, compared to 36 out of 103 (35%) in the average-risk group (OR=2.2, p=0.005). Overall, patients classified as increased risk per the FHHT were more likely to have neoplasia (OR=1.6, p=0.001).
Discussion: Patients identified at increased risk for the development of CRC based on the FHHT had significantly higher rates of neoplasia. This finding was particularly notable in patients aged < 50, supporting the utility of using a structured family history screening tool for CRC risk stratification to optimize resource allocation for screening colonoscopy and prioritize those at highest risk for CRC. Future directions include enhancing our predictive model by integrating demographic, lifestyle, and clinical factors to improve individualized risk assessment and screening efficiency.
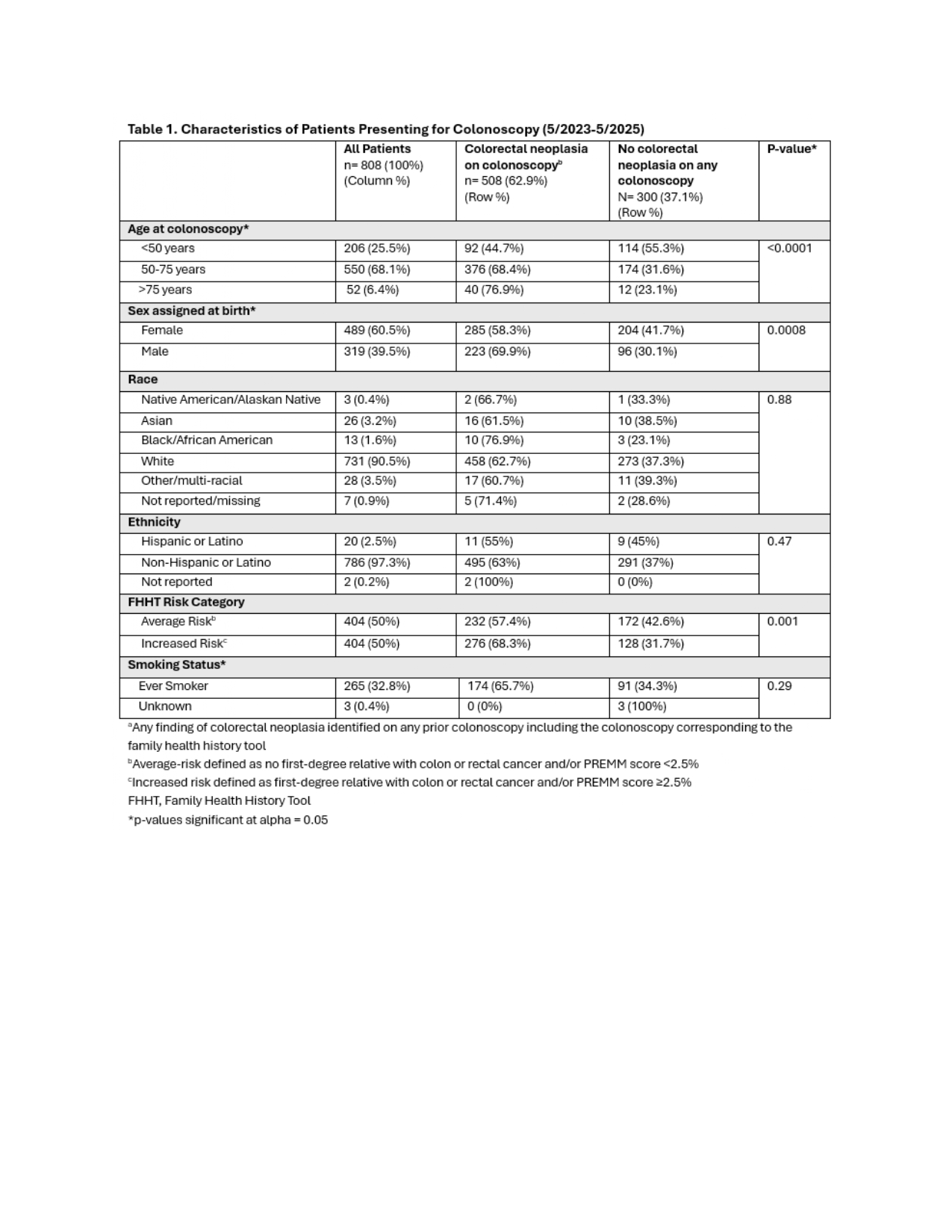
Figure: Demographics, risk stratification, and history of colorectal neoplasia of all patients presenting for colonoscopy between May 2023 and May 2025.
Disclosures:
Aleksandra Zarska indicated no relevant financial relationships.
Erika Koeppe indicated no relevant financial relationships.
Anudeep Mukkamala indicated no relevant financial relationships.
Joshua Smith indicated no relevant financial relationships.
Elena Stoffel indicated no relevant financial relationships.
Aleksandra Zarska, BS1, Erika Koeppe, MS2, Anudeep Mukkamala, MD2, Joshua Smith, MD2, Elena Stoffel, MD, MPH2. P0522 - Evaluating Real-World Performance of the Family Health History Tool for Identifying Individuals With Colorectal Neoplasia on Colonoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

