Sunday Poster Session
Category: Colorectal Cancer Prevention
P0502 - Implementation of Mailed Fecal Immunochemical Testing: A Quality Improvement Initiative
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Meagan H. Phox, DO (she/her/hers)
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Meagan H. Phox, DO1, John Thesing, DO1, Stephanie J. Melquist, MD, MPH2, Kyle Rowe, MD1
1University of Kansas School of Medicine, Wichita, KS; 2University of Kansas School of Medicine-Wichita, Wichita, KS
Introduction: Colorectal cancer (CRC) is the third most common cancer in men and women, and the second leading cause of cancer death in the United States. CRC incidence and mortality rates have declined due to changes in risk factors, early detection, and improved treatment. In 2021, the American College of Gastroenterology (ACG) strongly recommended colonoscopy and fecal immunochemical test (FIT) as primary screening modalities. Programmatic screening has been shown to improve screening rates over opportunistic screening. This quality improvement study aimed to compare outcomes from a systematic mailed FIT program versus opportunistic FIT screening in a VA medical center from February 2024 to April 2025.
Methods: To improve CRC screening rates, a systematic mailed FIT program was implemented. Traditionally, FIT kits were given only during in-person visits (opportunistic). The mailed approach is system-initiated, sending annual FIT kits to average-risk patients, independent of clinic visits. Exclusion criteria include personal history of adenomas or CRC, colonoscopy within 9 years, inflammatory bowel disease, family history of CRC, and recent initiation of Plavix.
Results: The opportunistic group received 2,781 kits with a 43% return rate (1,192 returned), while the mailed group sent 1,869 kits with a 33% return rate (614 returned). The opportunistic group had a higher FIT positivity rate (10% vs. 7%) and more completed colonoscopies (57 vs. 32). While opportunistic screening detected more adenomas (27 vs. 23), the mailed group had a higher adenoma detection rate (72% vs. 47%). More cases of advanced neoplasia were found in the opportunistic group (10 vs. 3), with detection rates of 18% vs. 9%.
Discussion: Opportunistic screening achieved higher overall engagement and detected more advanced neoplasia, showing that in-person counseling may be advantageous in ensuring patient participation. Neoplasia rates may have been influenced using opportunistic FIT testing in patients with alarm features. Mailed screening showed greater efficiency per colonoscopy, with a higher adenoma detection rate. FIT testing is convenient, cost-effective, and does not require medication or dietary restrictions. However, mailing FIT kits expands access to patients who may not attend regular preventive visits, addressing barriers like time, cost, and transportation. This proactive approach may help reduce disparities in preventive care.
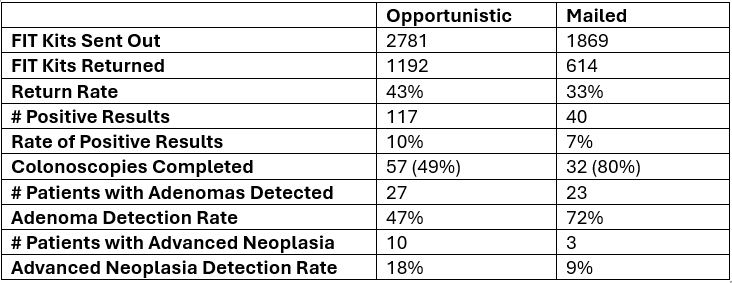
Figure: Table 1. Comparison of Opportunistic vs Mailed screening approach
Disclosures:
Meagan Phox indicated no relevant financial relationships.
John Thesing indicated no relevant financial relationships.
Stephanie Melquist indicated no relevant financial relationships.
Kyle Rowe indicated no relevant financial relationships.
Meagan H. Phox, DO1, John Thesing, DO1, Stephanie J. Melquist, MD, MPH2, Kyle Rowe, MD1. P0502 - Implementation of Mailed Fecal Immunochemical Testing: A Quality Improvement Initiative, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Kansas School of Medicine, Wichita, KS; 2University of Kansas School of Medicine-Wichita, Wichita, KS
Introduction: Colorectal cancer (CRC) is the third most common cancer in men and women, and the second leading cause of cancer death in the United States. CRC incidence and mortality rates have declined due to changes in risk factors, early detection, and improved treatment. In 2021, the American College of Gastroenterology (ACG) strongly recommended colonoscopy and fecal immunochemical test (FIT) as primary screening modalities. Programmatic screening has been shown to improve screening rates over opportunistic screening. This quality improvement study aimed to compare outcomes from a systematic mailed FIT program versus opportunistic FIT screening in a VA medical center from February 2024 to April 2025.
Methods: To improve CRC screening rates, a systematic mailed FIT program was implemented. Traditionally, FIT kits were given only during in-person visits (opportunistic). The mailed approach is system-initiated, sending annual FIT kits to average-risk patients, independent of clinic visits. Exclusion criteria include personal history of adenomas or CRC, colonoscopy within 9 years, inflammatory bowel disease, family history of CRC, and recent initiation of Plavix.
Results: The opportunistic group received 2,781 kits with a 43% return rate (1,192 returned), while the mailed group sent 1,869 kits with a 33% return rate (614 returned). The opportunistic group had a higher FIT positivity rate (10% vs. 7%) and more completed colonoscopies (57 vs. 32). While opportunistic screening detected more adenomas (27 vs. 23), the mailed group had a higher adenoma detection rate (72% vs. 47%). More cases of advanced neoplasia were found in the opportunistic group (10 vs. 3), with detection rates of 18% vs. 9%.
Discussion: Opportunistic screening achieved higher overall engagement and detected more advanced neoplasia, showing that in-person counseling may be advantageous in ensuring patient participation. Neoplasia rates may have been influenced using opportunistic FIT testing in patients with alarm features. Mailed screening showed greater efficiency per colonoscopy, with a higher adenoma detection rate. FIT testing is convenient, cost-effective, and does not require medication or dietary restrictions. However, mailing FIT kits expands access to patients who may not attend regular preventive visits, addressing barriers like time, cost, and transportation. This proactive approach may help reduce disparities in preventive care.
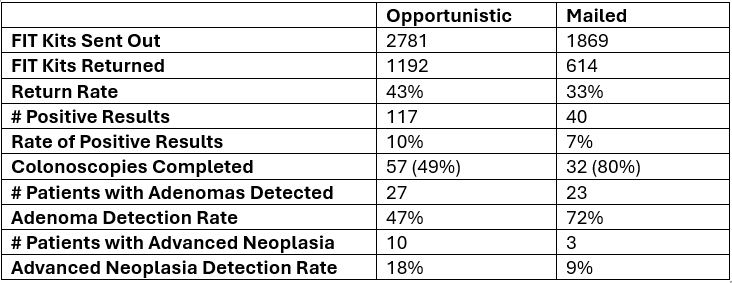
Figure: Table 1. Comparison of Opportunistic vs Mailed screening approach
Disclosures:
Meagan Phox indicated no relevant financial relationships.
John Thesing indicated no relevant financial relationships.
Stephanie Melquist indicated no relevant financial relationships.
Kyle Rowe indicated no relevant financial relationships.
Meagan H. Phox, DO1, John Thesing, DO1, Stephanie J. Melquist, MD, MPH2, Kyle Rowe, MD1. P0502 - Implementation of Mailed Fecal Immunochemical Testing: A Quality Improvement Initiative, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
