Sunday Poster Session
Category: Colorectal Cancer Prevention
P0498 - Conventional Patient Demographics Do Not Predict Completion of Two-Step Colorectal Cancer Screening
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Neha Narayan, MD (she/her/hers)
Temple University Hospital
Philadelphia, PA
Presenting Author(s)
Neha Narayan, MD1, Elizabeth Li, MD1, Jessica Luce. Thelemaque, BS2, Sara B. Colyer, MD1, Adam C.. Ehrlich, MD, MPH1, Holly Greenwald, MD1
1Temple University Hospital, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: There are multiple screening modalities for colorectal cancer (CRC), including stool-based options such as fecal immunochemical testing and multitarget stool DNA. The use of these non-invasive options is a two-step process requiring a colonoscopy, if positive. This study aims to identify patient and systemic factors that influence time to follow-up colonoscopy after a positive stool-based screening test in our urban, tertiary-care center.
Methods: Our electronic health record (EHR) was queried for individuals aged 45-85 years old who had a positive stool-based CRC screening test between 7/1/2021 and 1/1/2024. Charts were reviewed for patient demographic data, whether a follow-up colonoscopy was completed, and colonoscopy results, including pathology. As a surrogate for economic disparity, each patient was assigned a value corresponding to the Distressed Communities Index (DCI), which stratifies U.S. zip codes based on economic health.
Results: Demographics are summarized in Table 1. Out of 426 patients, 53.5% were female with a mean age of 64 (+/- 9.1) years; 58% identified as white, and 93% were primarily English-speaking. In this cohort, 58.5% (n=249) of patients had a confirmed follow-up colonoscopy, with 56.5% of these completed within 90 days of a positive test. Overall, 25.4% of patients lived in a ‘distressed’ area and 19% in an ‘at-risk’ area based on DCI. There was no difference in the rate of follow-up colonoscopy based on a variety of factors, including sex, age, race, ethnicity, insurance type, or DCI (Table 2). Lastly, there was no significant difference in the rate of advanced pathology (including malignancy) based on observed demographic categories, including age (p=0.701), sex (p=0.067), race (p=0.798), ethnicity (p=0.333). Medicare patients were more likely to have advanced pathology compared to Medicaid or commercial insurance (48.8% vs 25.7% vs 14.3%, p=0.05).
Discussion: Our data did not show significant differences in the rate of completed colonoscopy based on patient demographics or the Distressed Communities Index. Importantly, patient demographics other than insurance type did not affect the rate of advanced pathology. As use of two-step stool-based screening for CRC increases, it is vital to identify barriers to completion of colonoscopy. Screening tests without appropriate follow-up occurred at a high rate in this cohort, suggesting that new methods to identify those at risk of failing the two-step CRC screen are needed.
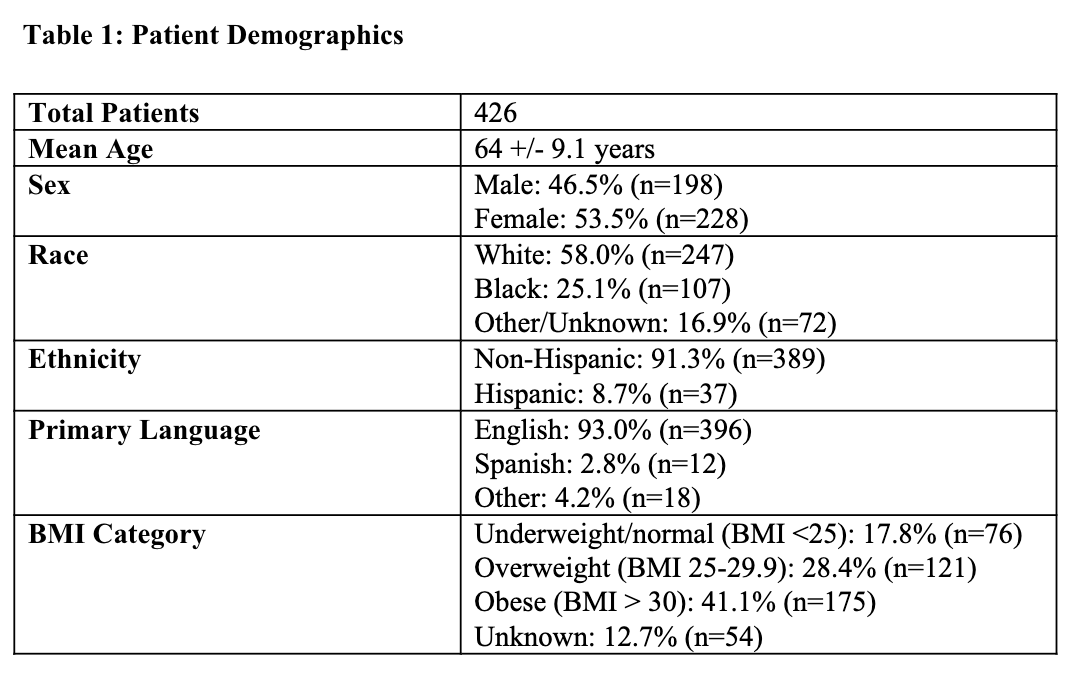
Figure: Table 1: Patient Demographics
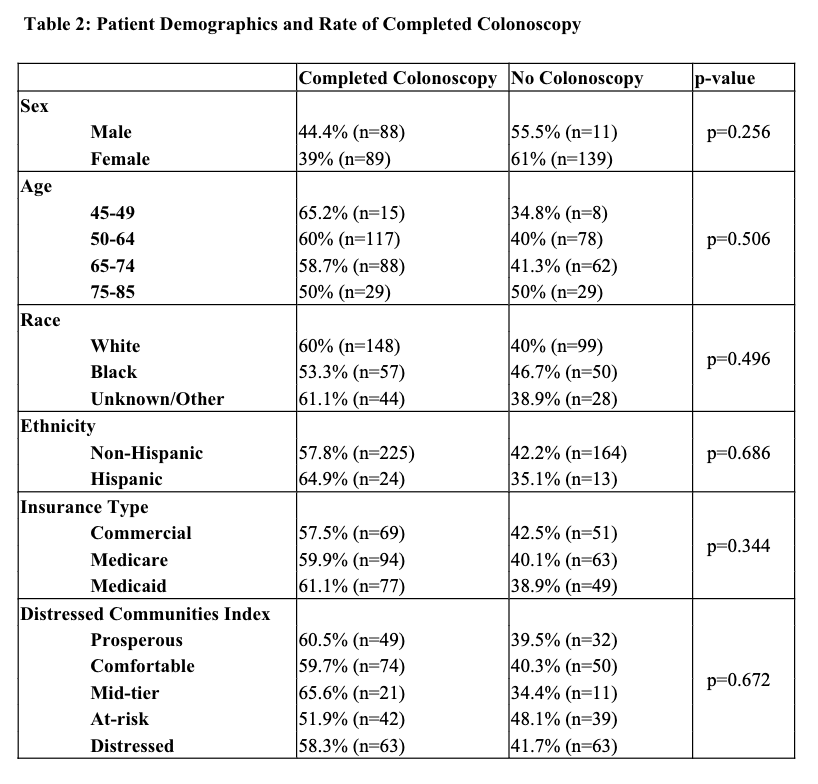
Figure: Table 2: Patient Characteristics and Rate of Completed Colonoscopy
Disclosures:
Neha Narayan indicated no relevant financial relationships.
Elizabeth Li indicated no relevant financial relationships.
Jessica Thelemaque indicated no relevant financial relationships.
Sara Colyer indicated no relevant financial relationships.
Adam Ehrlich: Abbvie – Consultant, Speakers Bureau. Bristol Meyers Squibb – Advisory Committee/Board Member, Speakers Bureau. Eli Lilly – Advisory Committee/Board Member, Speakers Bureau. Guardant – Advisory Committee/Board Member. J&J – Consultant.
Holly Greenwald indicated no relevant financial relationships.
Neha Narayan, MD1, Elizabeth Li, MD1, Jessica Luce. Thelemaque, BS2, Sara B. Colyer, MD1, Adam C.. Ehrlich, MD, MPH1, Holly Greenwald, MD1. P0498 - Conventional Patient Demographics Do Not Predict Completion of Two-Step Colorectal Cancer Screening, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Temple University Hospital, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: There are multiple screening modalities for colorectal cancer (CRC), including stool-based options such as fecal immunochemical testing and multitarget stool DNA. The use of these non-invasive options is a two-step process requiring a colonoscopy, if positive. This study aims to identify patient and systemic factors that influence time to follow-up colonoscopy after a positive stool-based screening test in our urban, tertiary-care center.
Methods: Our electronic health record (EHR) was queried for individuals aged 45-85 years old who had a positive stool-based CRC screening test between 7/1/2021 and 1/1/2024. Charts were reviewed for patient demographic data, whether a follow-up colonoscopy was completed, and colonoscopy results, including pathology. As a surrogate for economic disparity, each patient was assigned a value corresponding to the Distressed Communities Index (DCI), which stratifies U.S. zip codes based on economic health.
Results: Demographics are summarized in Table 1. Out of 426 patients, 53.5% were female with a mean age of 64 (+/- 9.1) years; 58% identified as white, and 93% were primarily English-speaking. In this cohort, 58.5% (n=249) of patients had a confirmed follow-up colonoscopy, with 56.5% of these completed within 90 days of a positive test. Overall, 25.4% of patients lived in a ‘distressed’ area and 19% in an ‘at-risk’ area based on DCI. There was no difference in the rate of follow-up colonoscopy based on a variety of factors, including sex, age, race, ethnicity, insurance type, or DCI (Table 2). Lastly, there was no significant difference in the rate of advanced pathology (including malignancy) based on observed demographic categories, including age (p=0.701), sex (p=0.067), race (p=0.798), ethnicity (p=0.333). Medicare patients were more likely to have advanced pathology compared to Medicaid or commercial insurance (48.8% vs 25.7% vs 14.3%, p=0.05).
Discussion: Our data did not show significant differences in the rate of completed colonoscopy based on patient demographics or the Distressed Communities Index. Importantly, patient demographics other than insurance type did not affect the rate of advanced pathology. As use of two-step stool-based screening for CRC increases, it is vital to identify barriers to completion of colonoscopy. Screening tests without appropriate follow-up occurred at a high rate in this cohort, suggesting that new methods to identify those at risk of failing the two-step CRC screen are needed.
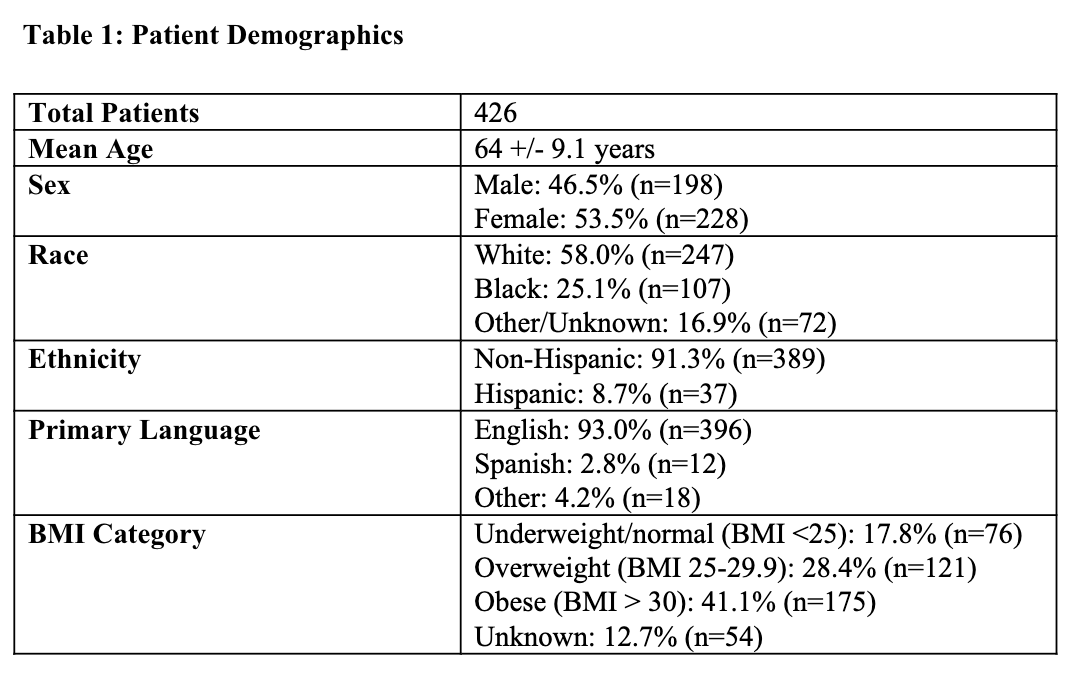
Figure: Table 1: Patient Demographics
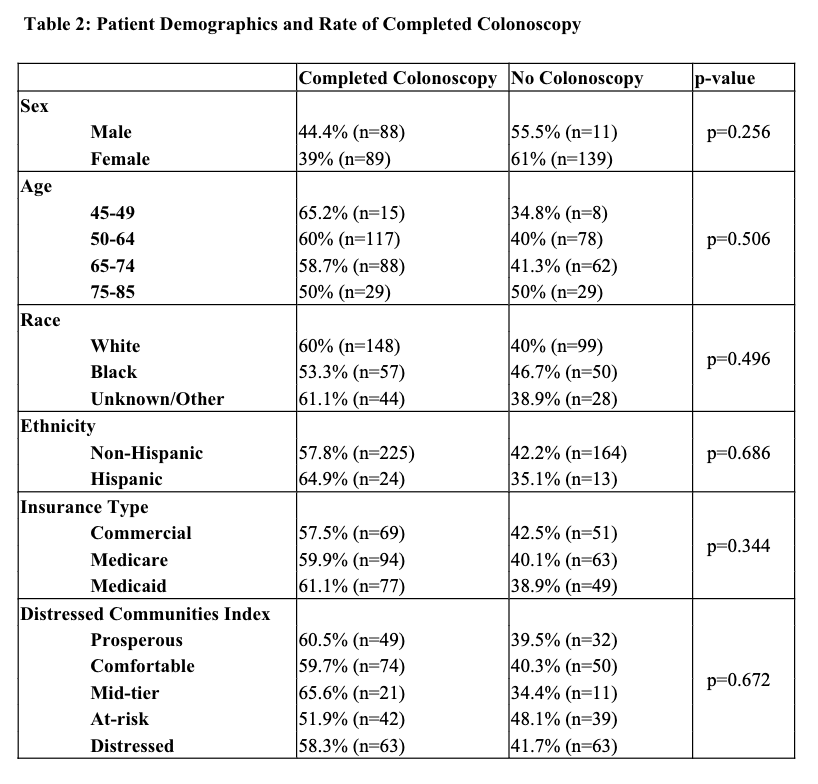
Figure: Table 2: Patient Characteristics and Rate of Completed Colonoscopy
Disclosures:
Neha Narayan indicated no relevant financial relationships.
Elizabeth Li indicated no relevant financial relationships.
Jessica Thelemaque indicated no relevant financial relationships.
Sara Colyer indicated no relevant financial relationships.
Adam Ehrlich: Abbvie – Consultant, Speakers Bureau. Bristol Meyers Squibb – Advisory Committee/Board Member, Speakers Bureau. Eli Lilly – Advisory Committee/Board Member, Speakers Bureau. Guardant – Advisory Committee/Board Member. J&J – Consultant.
Holly Greenwald indicated no relevant financial relationships.
Neha Narayan, MD1, Elizabeth Li, MD1, Jessica Luce. Thelemaque, BS2, Sara B. Colyer, MD1, Adam C.. Ehrlich, MD, MPH1, Holly Greenwald, MD1. P0498 - Conventional Patient Demographics Do Not Predict Completion of Two-Step Colorectal Cancer Screening, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
