Sunday Poster Session
Category: Colorectal Cancer Prevention
P0479 - Sociodemographic Disparities in Colorectal Cancer Screening Nonadherence: Insights From Behavioral Risk Factor Surveillance System (BRFSS) 2022-2023
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AA
Adedeji Adenusi, MD, MPH
One Brooklyn Health-Interfaith Medical Center
Brooklyn, NY
Presenting Author(s)
Award: ACG Presidential Poster Award
Adedeji Adenusi, MD, MPH1, Samuel Sule-Saa, MBChB1, Olamide Asifat, MD, MPH2, Mehakgul Mastoi, MD1, Emeka S. Obi, MBBS3, Aasma Shaukat, MD, MPH, FACG4
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2Georgia Southern University, Statesboro, GA; 3One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 4NYU Grossman School of Medicine, Division of Gastroenterology and Hepatology, New York, NY
Introduction: Colorectal cancer (CRC) remains a leading cause of cancer-related morbidity and mortality in the United States, despite the availability of effective screening tools. Adherence to screening recommendations is a major challenge influenced by various sociodemographic elements. This study investigates determinants and disparities in CRC screening nonadherence across various screening modalities.
Methods: We included respondents aged 45 to 75 years from the BRFSS dataset of 2022-2023. Key variables extracted included CRC screening modalities and frequency (colonoscopy, sigmoidoscopy, stool testing, and virtual colonoscopy), and socio-demographics. Multivariate Logistic regression was performed to explore associations between social determinants and CRC screening nonadherence.
Results: A total of 239,512,188 respondents, of which majority were White (63.90%), female (51.92%), had an annual income ≥$50,000 (60.65%), had access to a primary care physician (90.55%), were married (62.17%), and resided in urban areas (93.03%). Screening rates were high with colonoscopy (99.32%) and stool-based test. (80.67%) reported.
The odds of colonoscopy nonadherence were significantly lower among Black non-Hispanic (aOR=0.539 (0.456-0.637), p < .0001) or those with access to PCP (0.469 (0.397-0.554), < .0001) or urban residents, 0.849 (0.748-0.962), 0.0105). Conversely, it was higher in individuals who earned < $50k per annum (1.264 (1.138-1.405), < .0001) or were divorced (1.206 (1.077-1.350), 0.0012) or Widowed (1.190 (1.021-1.388), 0.0265).
Odds of Sigmoidoscopy nonadherence were lower among Black non-Hispanic (0.138 (0.063-0.304), < .0001) or Hispanic (0.209 (0.074-0.589), 0.0032) or individuals who earned < $50k per annum, 0.496 (0.320-0.769), 0.0018), but it was higher in urban residents (1.723 (1.061-2.796), 0.0279).
Lastly, the odds of stool test nonadherence were lower among Hispanic (0.732 (0.552-0.970), 0.0296) or those with access to PCP (0.612 (0.453-0.827), 0.0014) or Divorced (0.869 (0.758-0.996), 0.0.431) or uneducated (0.635 (0.463-0.869), 0.0046). However, it was higher in males (1.163 (1.044-1.294), 0.0059).
Discussion: Black, Hispanic, and American Indian/Alaskan Native groups showed better use of screening methods. This challenges the belief of non-adherence among these minority groups. Our study highlights the importance of creating specific, culturally aware programs to overcome obstacles and improve screening adherence for different communities.
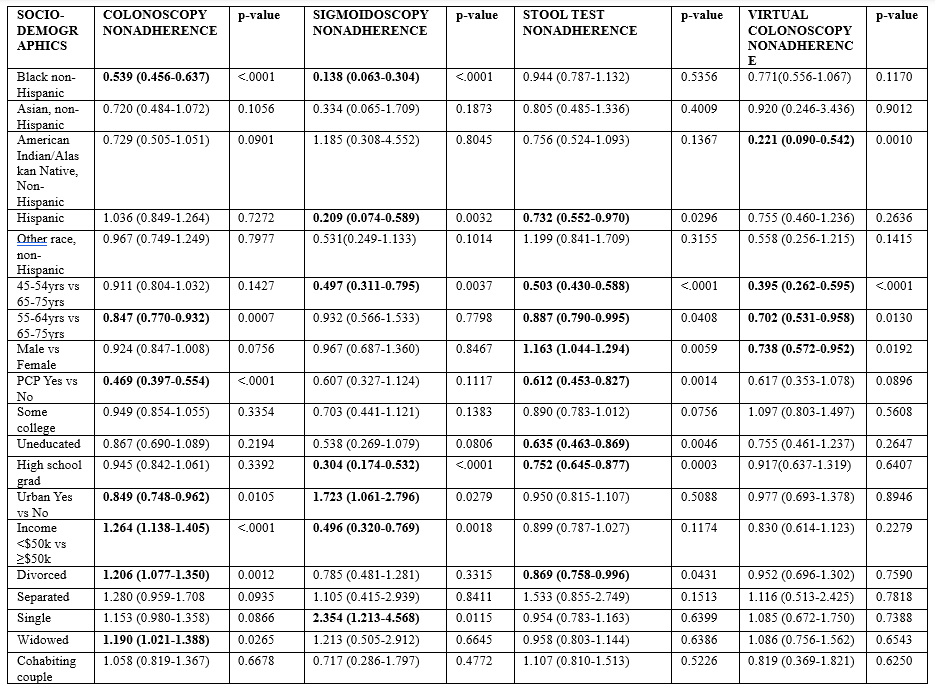
Figure: Multivariable Logistic Regression Analysis of Sociodemographic Determinants of CRC Screening Non-adherence
Disclosures:
Adedeji Adenusi indicated no relevant financial relationships.
Samuel Sule-Saa indicated no relevant financial relationships.
Olamide Asifat indicated no relevant financial relationships.
Mehakgul Mastoi indicated no relevant financial relationships.
Emeka Obi indicated no relevant financial relationships.
Aasma Shaukat: Freenome inc – Consultant.
Adedeji Adenusi, MD, MPH1, Samuel Sule-Saa, MBChB1, Olamide Asifat, MD, MPH2, Mehakgul Mastoi, MD1, Emeka S. Obi, MBBS3, Aasma Shaukat, MD, MPH, FACG4. P0479 - Sociodemographic Disparities in Colorectal Cancer Screening Nonadherence: Insights From Behavioral Risk Factor Surveillance System (BRFSS) 2022-2023, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Adedeji Adenusi, MD, MPH1, Samuel Sule-Saa, MBChB1, Olamide Asifat, MD, MPH2, Mehakgul Mastoi, MD1, Emeka S. Obi, MBBS3, Aasma Shaukat, MD, MPH, FACG4
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2Georgia Southern University, Statesboro, GA; 3One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 4NYU Grossman School of Medicine, Division of Gastroenterology and Hepatology, New York, NY
Introduction: Colorectal cancer (CRC) remains a leading cause of cancer-related morbidity and mortality in the United States, despite the availability of effective screening tools. Adherence to screening recommendations is a major challenge influenced by various sociodemographic elements. This study investigates determinants and disparities in CRC screening nonadherence across various screening modalities.
Methods: We included respondents aged 45 to 75 years from the BRFSS dataset of 2022-2023. Key variables extracted included CRC screening modalities and frequency (colonoscopy, sigmoidoscopy, stool testing, and virtual colonoscopy), and socio-demographics. Multivariate Logistic regression was performed to explore associations between social determinants and CRC screening nonadherence.
Results: A total of 239,512,188 respondents, of which majority were White (63.90%), female (51.92%), had an annual income ≥$50,000 (60.65%), had access to a primary care physician (90.55%), were married (62.17%), and resided in urban areas (93.03%). Screening rates were high with colonoscopy (99.32%) and stool-based test. (80.67%) reported.
The odds of colonoscopy nonadherence were significantly lower among Black non-Hispanic (aOR=0.539 (0.456-0.637), p < .0001) or those with access to PCP (0.469 (0.397-0.554), < .0001) or urban residents, 0.849 (0.748-0.962), 0.0105). Conversely, it was higher in individuals who earned < $50k per annum (1.264 (1.138-1.405), < .0001) or were divorced (1.206 (1.077-1.350), 0.0012) or Widowed (1.190 (1.021-1.388), 0.0265).
Odds of Sigmoidoscopy nonadherence were lower among Black non-Hispanic (0.138 (0.063-0.304), < .0001) or Hispanic (0.209 (0.074-0.589), 0.0032) or individuals who earned < $50k per annum, 0.496 (0.320-0.769), 0.0018), but it was higher in urban residents (1.723 (1.061-2.796), 0.0279).
Lastly, the odds of stool test nonadherence were lower among Hispanic (0.732 (0.552-0.970), 0.0296) or those with access to PCP (0.612 (0.453-0.827), 0.0014) or Divorced (0.869 (0.758-0.996), 0.0.431) or uneducated (0.635 (0.463-0.869), 0.0046). However, it was higher in males (1.163 (1.044-1.294), 0.0059).
Discussion: Black, Hispanic, and American Indian/Alaskan Native groups showed better use of screening methods. This challenges the belief of non-adherence among these minority groups. Our study highlights the importance of creating specific, culturally aware programs to overcome obstacles and improve screening adherence for different communities.
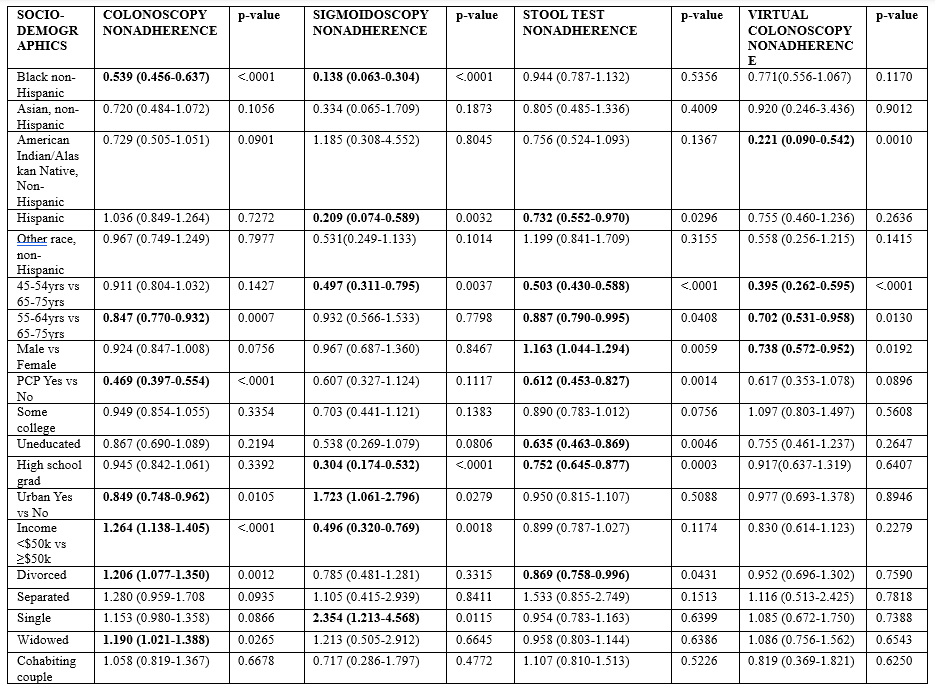
Figure: Multivariable Logistic Regression Analysis of Sociodemographic Determinants of CRC Screening Non-adherence
Disclosures:
Adedeji Adenusi indicated no relevant financial relationships.
Samuel Sule-Saa indicated no relevant financial relationships.
Olamide Asifat indicated no relevant financial relationships.
Mehakgul Mastoi indicated no relevant financial relationships.
Emeka Obi indicated no relevant financial relationships.
Aasma Shaukat: Freenome inc – Consultant.
Adedeji Adenusi, MD, MPH1, Samuel Sule-Saa, MBChB1, Olamide Asifat, MD, MPH2, Mehakgul Mastoi, MD1, Emeka S. Obi, MBBS3, Aasma Shaukat, MD, MPH, FACG4. P0479 - Sociodemographic Disparities in Colorectal Cancer Screening Nonadherence: Insights From Behavioral Risk Factor Surveillance System (BRFSS) 2022-2023, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

