Sunday Poster Session
Category: Colorectal Cancer Prevention
P0471 - BRAF Mutations Indicate Poor Survival in Metastatic Colorectal Cancer: A Reconstructed Individual Patient Data Meta-Analysis of Randomized Controlled Trials
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- SK
Syeda Kanza Kazmi, MD (she/her/hers)
Penn State Health Milton S. Hershey Medical Center
Hershey, PA
Presenting Author(s)
Award: ACG Presidential Poster Award
Syeda Kanza Kazmi, MD1, Muhammad Abdul Rehman, MBBS2, Aqsa Kabir, MBBS3
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2Mayo Clinic, Byron, MN; 3Dow Medical College, Karachi, Sindh, Pakistan
Introduction: Metastatic colorectal cancer (mCRC) is a leading cause of cancer-related mortality. Among its subtypes, BRAF-mutated mCRC, particularly V600E, is associated with aggressive behavior and poor outcomes. Although anti-VEGF therapies are commonly used in mCRC, their role in the BRAF-mutated population remains uncertain. We aim to evaluate the survival outcomes of BRAF-mutated mCRC patients receiving anti-VEGF therapy compared to those with RAS mutations.
Methods: We searched MEDLINE from inception to May 2025 for randomized controlled trials (RCTs) reporting outcomes in BRAF-mutated mCRC treated with anti-VEGF agents. Time-to-event data were extracted from Kaplan-Meier curves, and individual patient data were reconstructed using R. Cox proportional hazards models estimated hazard ratios (HRs) and median overall (OS) and progression-free survival (PFS).
Results: Five RCTs were included. In the overall cohort, patients with BRAF-mutant mCRC (n = 171) had significantly worse OS compared to RAS-mutant patients (n = 936) [HR 2.11; 95% CI, 1.78–2.51; p < 0.0001], with a median OS of 10.1 vs 22.5 months. PFS was also inferior [HR 1.49; 95% CI, 1.19–1.87; p = 0.00037; median 5.0 vs 8.0 months]. After maintenance therapy, BRAF-mutant patients (n = 83) had significantly shorter OS [HR 1.78; 95% CI, 1.40–2.27; p < 0.0001], while PFS was similar [HR 0.71; 95% CI, 0.47–1.07; p = 0.12]. For treatment-naive patients receiving initial therapy, BRAF-mutant patients (n = 47) again had significantly worse OS [HR 1.92; 95% CI, 1.39–2.65; p < 0.0001] and PFS [HR 1.97; 95% CI, 1.30–3.00; p = 0.0012] compared to RAS-mutant patients (n = 403). In this subgroup, those treated with FOLFOXIRI (n = 14) had improved median OS (13.5 vs 10.9 months) and PFS (7.2 vs 6.8 months) compared to FOLFIRI (n = 33), though differences were not statistically significant.
Discussion: BRAF-mutant mCRC is associated with significantly worse survival compared to RAS-mutant disease across all treatment phases. These findings emphasize the need for early molecular profiling, consideration of intensified first-line regimens, and prompt initiation of BRAF-targeted strategies upon progression. Limitations include trial heterogeneity and small sample sizes. Modern BRAF-targeted therapies (e.g., encorafenib plus cetuximab) were not represented. Future studies should refine sequencing of triplet chemotherapy versus targeted agents, evaluate maintenance strategies, and explore subclass-specific responses (V600E vs non-V600E).
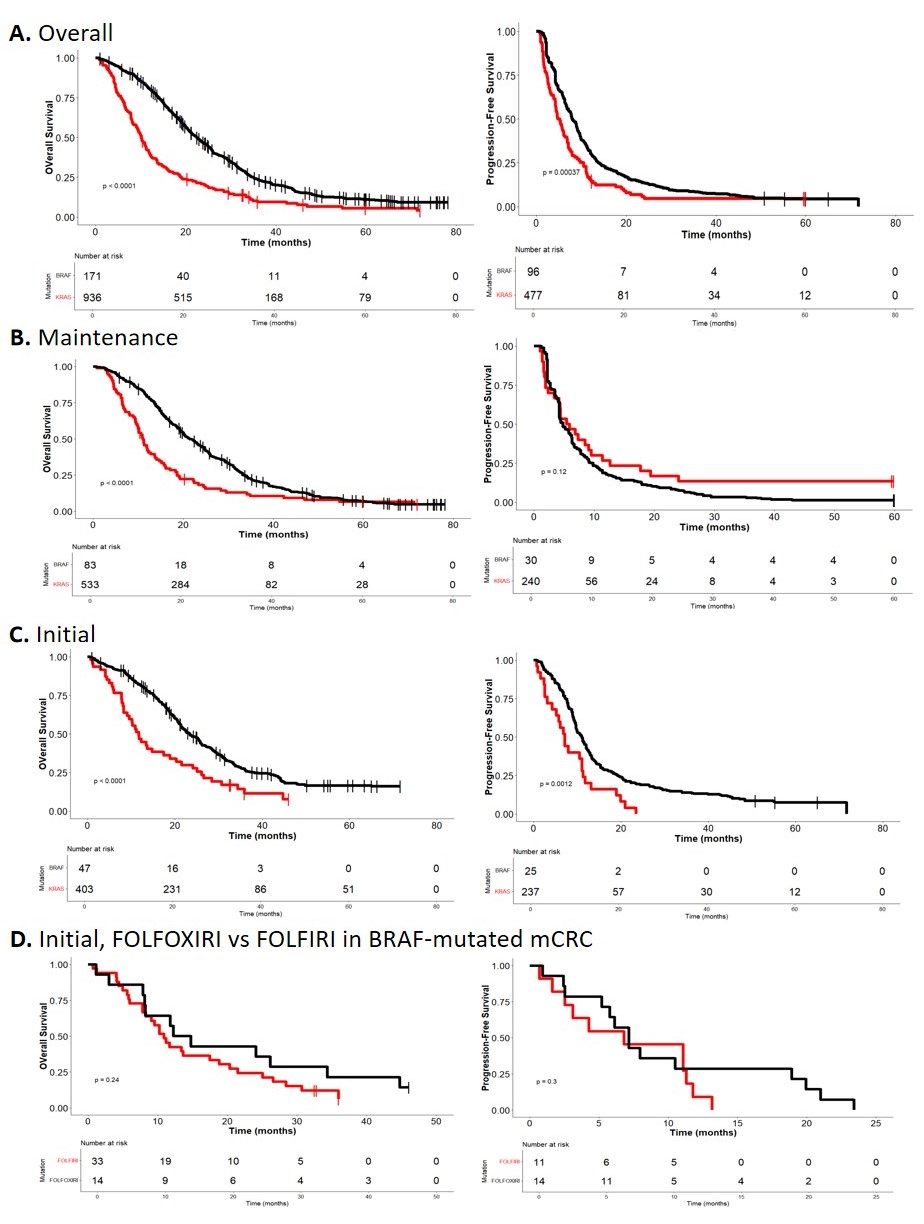
Figure: Table Showing Hazard Ratios (HR), P-Values and Median Survival from RAS- Mutated versus BRAF- Mutated mCRC Treated with Anti-VEGF Therapy.
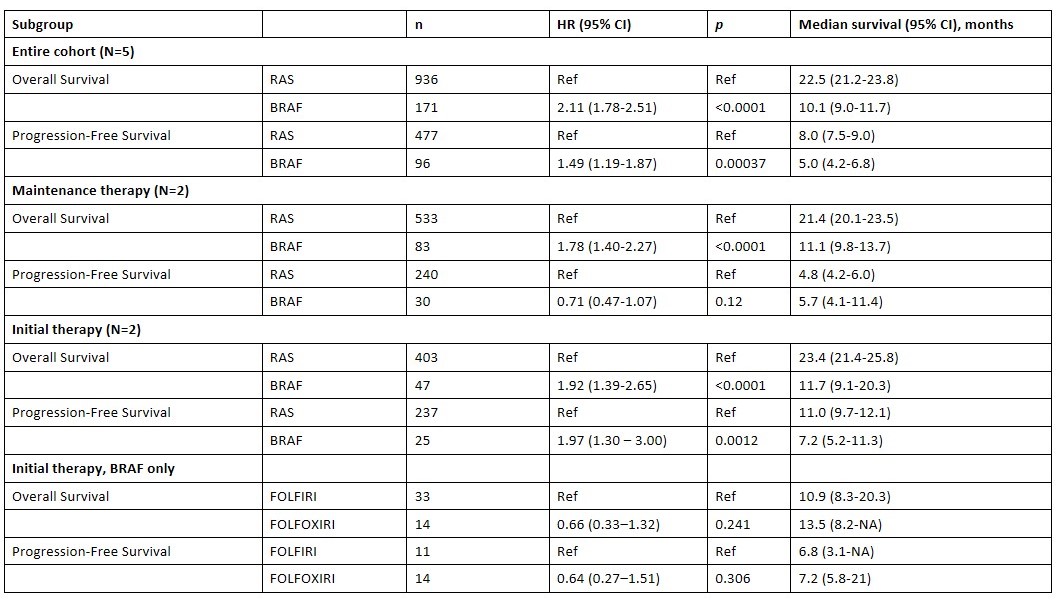
Figure: Overall survival and progression-free survival Kaplan-Meier Curves for both BRAF and RAS-mutated mCRC treated with anti-VEGF therapy.
Disclosures:
Syeda Kanza Kazmi indicated no relevant financial relationships.
Muhammad Abdul Rehman indicated no relevant financial relationships.
Aqsa Kabir indicated no relevant financial relationships.
Syeda Kanza Kazmi, MD1, Muhammad Abdul Rehman, MBBS2, Aqsa Kabir, MBBS3. P0471 - BRAF Mutations Indicate Poor Survival in Metastatic Colorectal Cancer: A Reconstructed Individual Patient Data Meta-Analysis of Randomized Controlled Trials, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Syeda Kanza Kazmi, MD1, Muhammad Abdul Rehman, MBBS2, Aqsa Kabir, MBBS3
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2Mayo Clinic, Byron, MN; 3Dow Medical College, Karachi, Sindh, Pakistan
Introduction: Metastatic colorectal cancer (mCRC) is a leading cause of cancer-related mortality. Among its subtypes, BRAF-mutated mCRC, particularly V600E, is associated with aggressive behavior and poor outcomes. Although anti-VEGF therapies are commonly used in mCRC, their role in the BRAF-mutated population remains uncertain. We aim to evaluate the survival outcomes of BRAF-mutated mCRC patients receiving anti-VEGF therapy compared to those with RAS mutations.
Methods: We searched MEDLINE from inception to May 2025 for randomized controlled trials (RCTs) reporting outcomes in BRAF-mutated mCRC treated with anti-VEGF agents. Time-to-event data were extracted from Kaplan-Meier curves, and individual patient data were reconstructed using R. Cox proportional hazards models estimated hazard ratios (HRs) and median overall (OS) and progression-free survival (PFS).
Results: Five RCTs were included. In the overall cohort, patients with BRAF-mutant mCRC (n = 171) had significantly worse OS compared to RAS-mutant patients (n = 936) [HR 2.11; 95% CI, 1.78–2.51; p < 0.0001], with a median OS of 10.1 vs 22.5 months. PFS was also inferior [HR 1.49; 95% CI, 1.19–1.87; p = 0.00037; median 5.0 vs 8.0 months]. After maintenance therapy, BRAF-mutant patients (n = 83) had significantly shorter OS [HR 1.78; 95% CI, 1.40–2.27; p < 0.0001], while PFS was similar [HR 0.71; 95% CI, 0.47–1.07; p = 0.12]. For treatment-naive patients receiving initial therapy, BRAF-mutant patients (n = 47) again had significantly worse OS [HR 1.92; 95% CI, 1.39–2.65; p < 0.0001] and PFS [HR 1.97; 95% CI, 1.30–3.00; p = 0.0012] compared to RAS-mutant patients (n = 403). In this subgroup, those treated with FOLFOXIRI (n = 14) had improved median OS (13.5 vs 10.9 months) and PFS (7.2 vs 6.8 months) compared to FOLFIRI (n = 33), though differences were not statistically significant.
Discussion: BRAF-mutant mCRC is associated with significantly worse survival compared to RAS-mutant disease across all treatment phases. These findings emphasize the need for early molecular profiling, consideration of intensified first-line regimens, and prompt initiation of BRAF-targeted strategies upon progression. Limitations include trial heterogeneity and small sample sizes. Modern BRAF-targeted therapies (e.g., encorafenib plus cetuximab) were not represented. Future studies should refine sequencing of triplet chemotherapy versus targeted agents, evaluate maintenance strategies, and explore subclass-specific responses (V600E vs non-V600E).
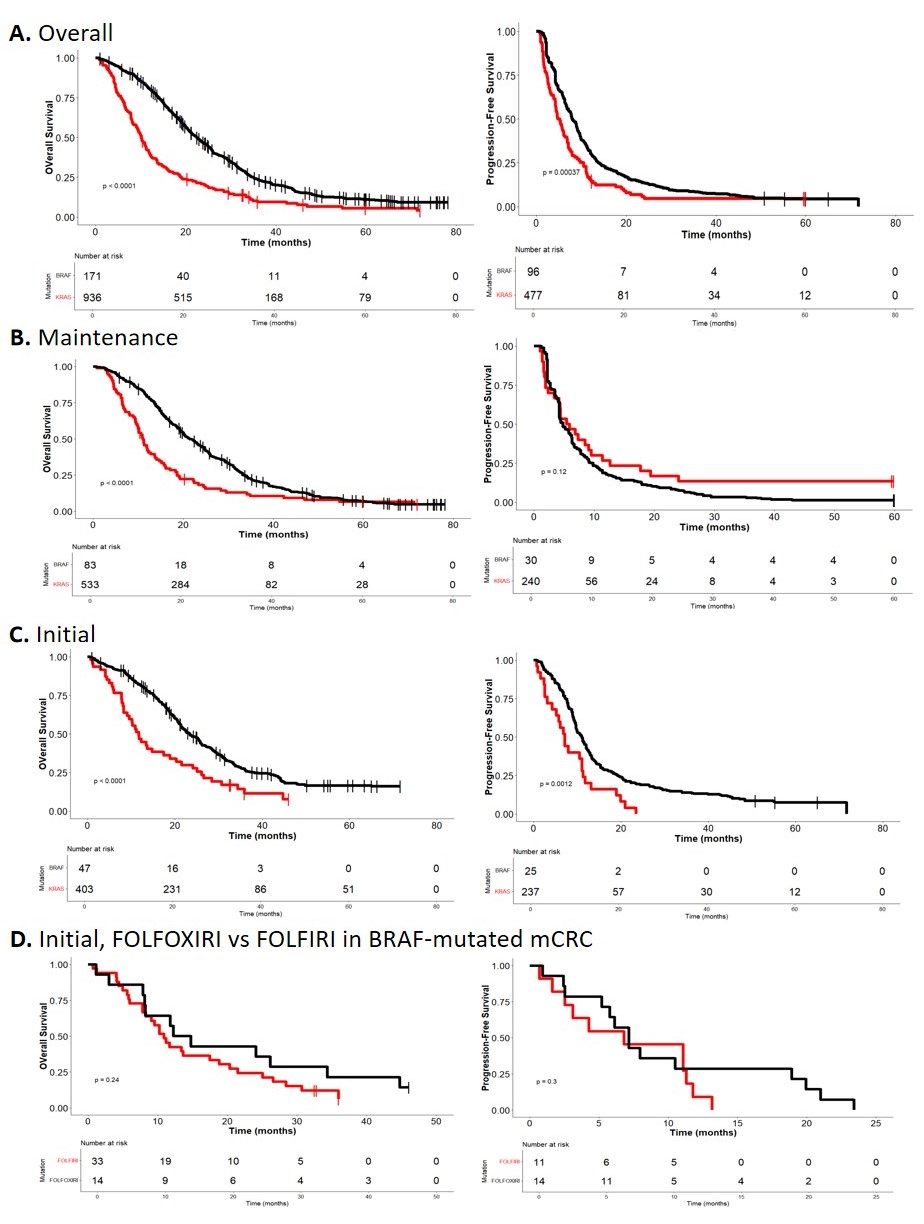
Figure: Table Showing Hazard Ratios (HR), P-Values and Median Survival from RAS- Mutated versus BRAF- Mutated mCRC Treated with Anti-VEGF Therapy.
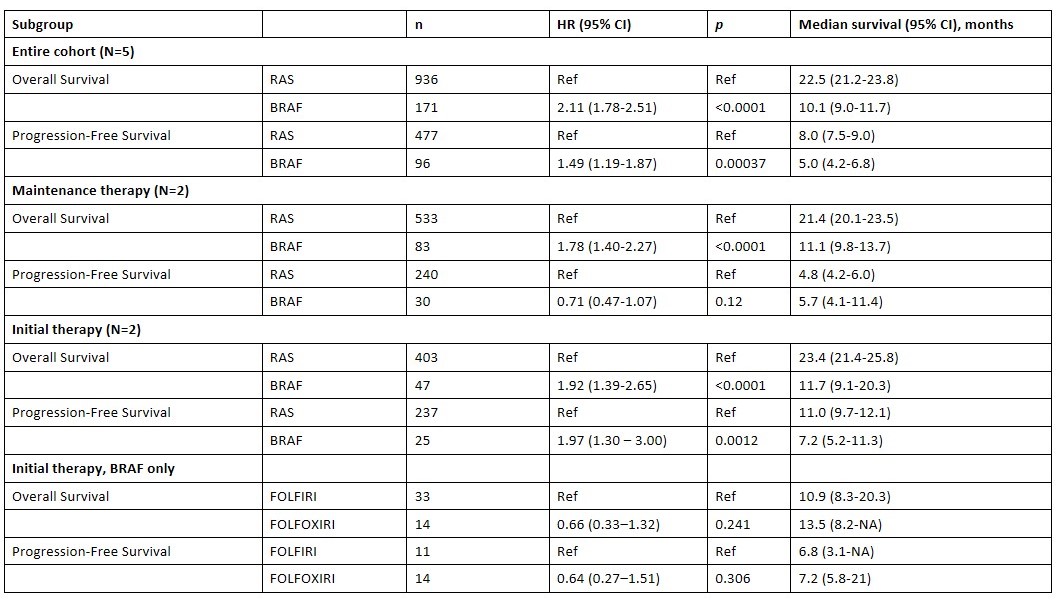
Figure: Overall survival and progression-free survival Kaplan-Meier Curves for both BRAF and RAS-mutated mCRC treated with anti-VEGF therapy.
Disclosures:
Syeda Kanza Kazmi indicated no relevant financial relationships.
Muhammad Abdul Rehman indicated no relevant financial relationships.
Aqsa Kabir indicated no relevant financial relationships.
Syeda Kanza Kazmi, MD1, Muhammad Abdul Rehman, MBBS2, Aqsa Kabir, MBBS3. P0471 - BRAF Mutations Indicate Poor Survival in Metastatic Colorectal Cancer: A Reconstructed Individual Patient Data Meta-Analysis of Randomized Controlled Trials, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

