Sunday Poster Session
Category: Colorectal Cancer Prevention
P0465 - Rising Colorectal Cancer Mortality Among US Adults Aged 35-54 (1999-2020): A Nationwide Analysis of Disparities by Race, Region, and Urbanization
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Zainab Rafaqat, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Zainab Rafaqat, MD1, Umar Abdul Rehman Khalid, MBBS2, Ali Akram Qureshi, MBBS2, Muhammad Faiq Akram, MBBS3, Christopher Bouvette, MD4, Jalal Gondal, MD4, Ijlal Akbar. Ali, MD5
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3Allama Iqbal Medical College, Lahore, Lahore, Punjab, Pakistan; 4College of Medicine, University of Oklahoma Health Sciences Center, Oklahoma City, OK; 5University of Oklahoma, Oklahoma City, OK
Introduction: Colorectal cancer (CRC) is the second leading cause of cancer-related death in the United States. Once considered a disease of older adults, CRC is now increasingly affecting younger individuals. Recent epidemiological data reveal an unsettling rise in CRC incidence and mortality among midlife adults, prompting a re-evaluation of current screening guidelines and health equity strategies. This study examines national mortality trends in adults aged 35–54 and evaluates disparities based on sex, race, geographic region, and urbanization.
Methods: We analyzed CRC mortality data (ICD-10 codes C18–C20) from the CDC WONDER database (1999–2020). Age-adjusted mortality rates (AAMRs) per 100,000 were calculated for adults aged 35–54 and stratified by sex, race/ethnicity, urban-rural status, state, and census region. Temporal trends were evaluated using Joinpoint regression to estimate annual percent changes (APCs) with 95% confidence intervals (CI).
Results: Between 1999 and 2020, 136,325 CRC-related deaths occurred among adults aged 35–54. AAMR initially increased (1999–2001; APC: 1.8%), declined (2001–2005; APC: -2.95%), then rose again (2005–2020; APC: 0.9%). Males consistently exhibited higher AAMRs than females (Average APC: 0.7 vs. 0.19). Rural males had the highest AAMR (9.4), while urban females had the lowest (5.8). Racial disparities were stark: non-Hispanic Black males had the highest AAMR (12.3), followed by NH Black females (9.3). States with the highest mortality included Mississippi (11.2), Arkansas (9.4), Louisiana (9.3), and Oklahoma (9.0).
Discussion: The rising CRC mortality among adults in midlife reflects a concerning trend that may be driven by multiple structural and behavioral determinants. The disproportionate burden observed in southern and rural states suggests a correlation with reduced health literacy, delayed symptom recognition, and inadequate access to advanced care. These barriers likely contribute to late-stage diagnosis and poor outcomes. Public health efforts must prioritize early education, improved healthcare infrastructure, and more equitable access to screening. Further studies are needed to understand these trends and guide effective intervention strategies to reverse rising mortality rates.
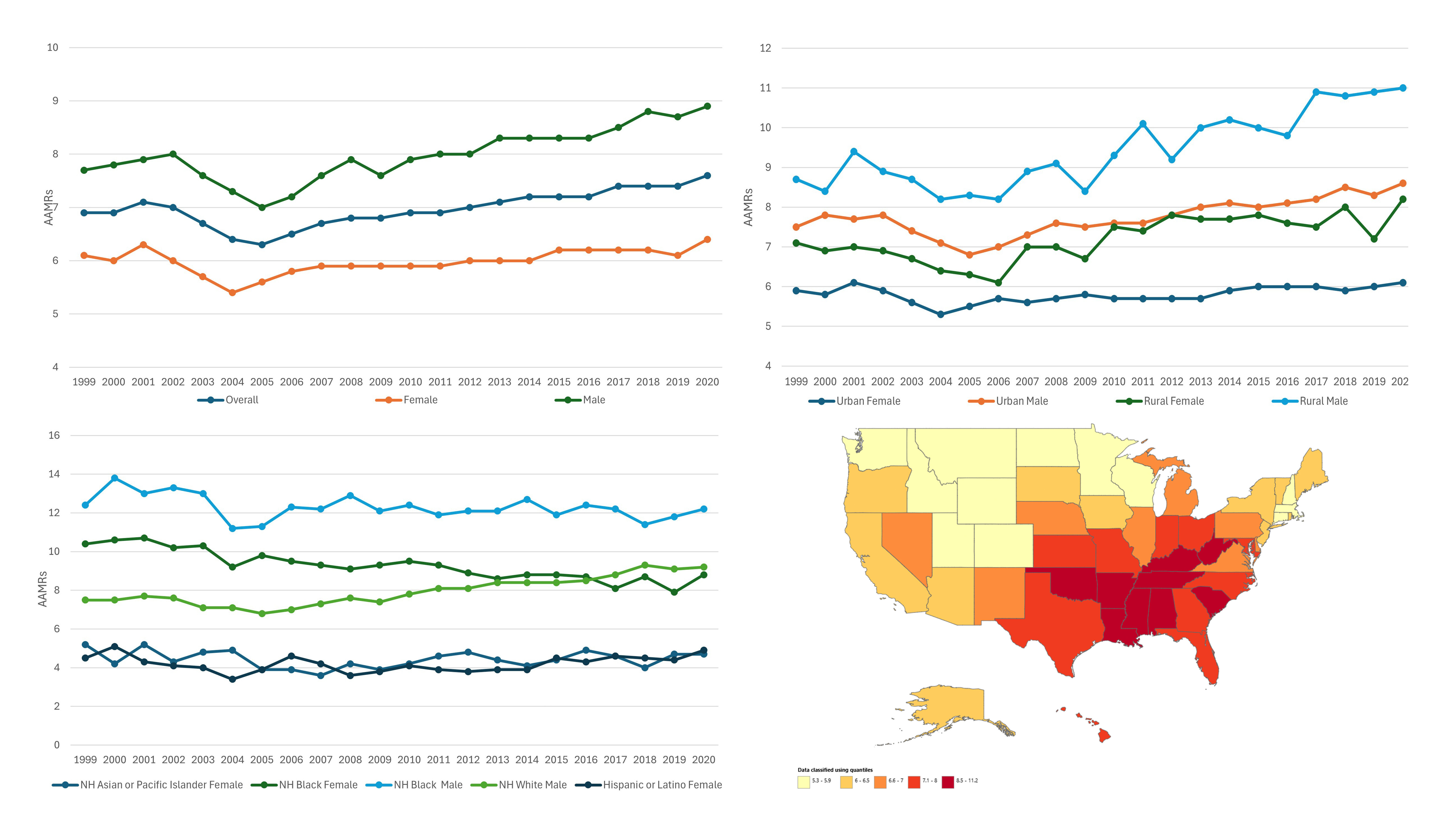
Figure: Graphical representation of Age Adjusted mortality based of CRC
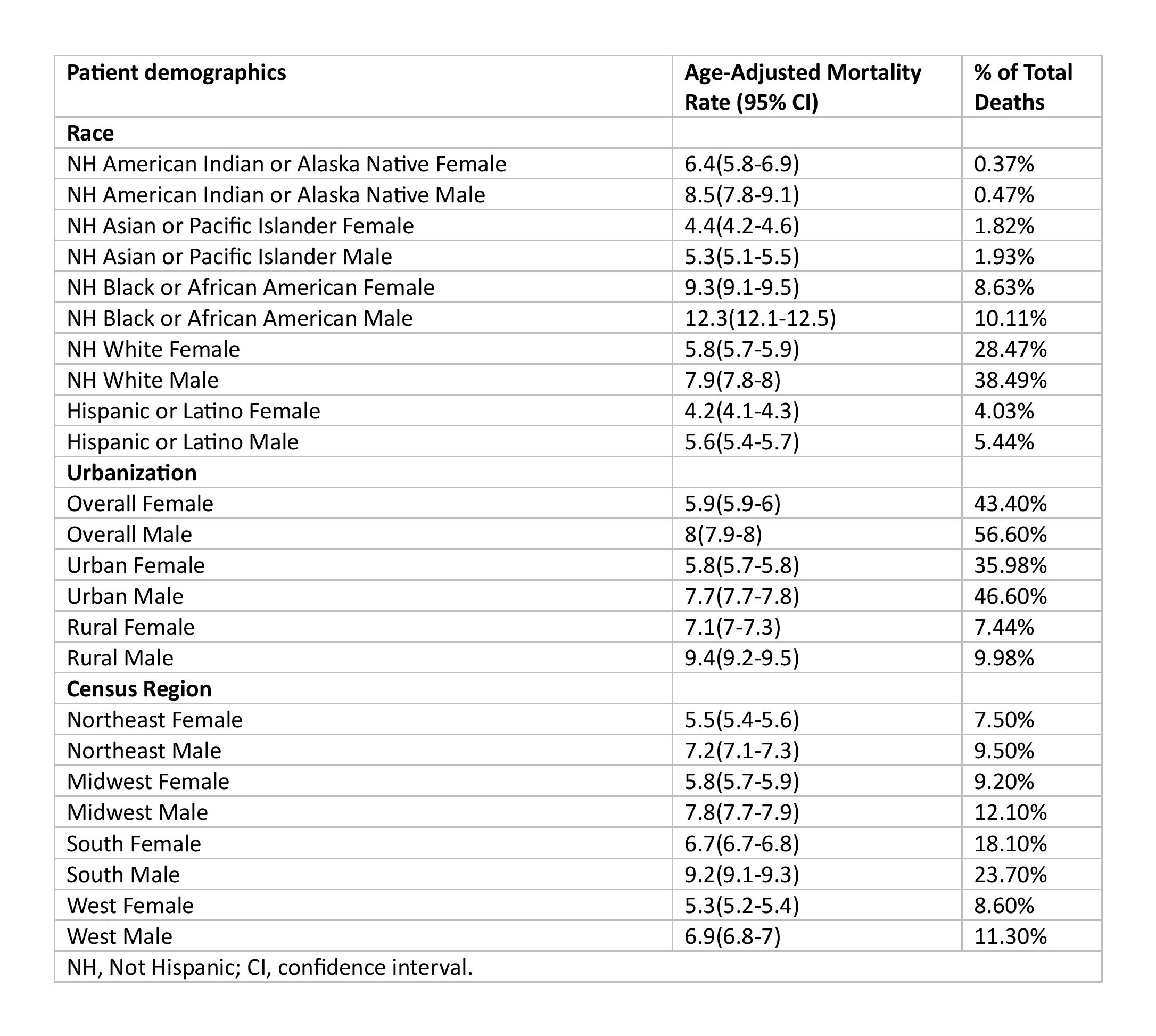
Figure: Age Adjusted Mortality based on race, geographical distribution, urbanization and gender
Disclosures:
Zainab Rafaqat indicated no relevant financial relationships.
Umar Abdul Rehman Khalid indicated no relevant financial relationships.
Ali Akram Qureshi indicated no relevant financial relationships.
Muhammad Faiq Akram indicated no relevant financial relationships.
Christopher Bouvette indicated no relevant financial relationships.
Jalal Gondal indicated no relevant financial relationships.
Ijlal Ali indicated no relevant financial relationships.
Zainab Rafaqat, MD1, Umar Abdul Rehman Khalid, MBBS2, Ali Akram Qureshi, MBBS2, Muhammad Faiq Akram, MBBS3, Christopher Bouvette, MD4, Jalal Gondal, MD4, Ijlal Akbar. Ali, MD5. P0465 - Rising Colorectal Cancer Mortality Among US Adults Aged 35-54 (1999-2020): A Nationwide Analysis of Disparities by Race, Region, and Urbanization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3Allama Iqbal Medical College, Lahore, Lahore, Punjab, Pakistan; 4College of Medicine, University of Oklahoma Health Sciences Center, Oklahoma City, OK; 5University of Oklahoma, Oklahoma City, OK
Introduction: Colorectal cancer (CRC) is the second leading cause of cancer-related death in the United States. Once considered a disease of older adults, CRC is now increasingly affecting younger individuals. Recent epidemiological data reveal an unsettling rise in CRC incidence and mortality among midlife adults, prompting a re-evaluation of current screening guidelines and health equity strategies. This study examines national mortality trends in adults aged 35–54 and evaluates disparities based on sex, race, geographic region, and urbanization.
Methods: We analyzed CRC mortality data (ICD-10 codes C18–C20) from the CDC WONDER database (1999–2020). Age-adjusted mortality rates (AAMRs) per 100,000 were calculated for adults aged 35–54 and stratified by sex, race/ethnicity, urban-rural status, state, and census region. Temporal trends were evaluated using Joinpoint regression to estimate annual percent changes (APCs) with 95% confidence intervals (CI).
Results: Between 1999 and 2020, 136,325 CRC-related deaths occurred among adults aged 35–54. AAMR initially increased (1999–2001; APC: 1.8%), declined (2001–2005; APC: -2.95%), then rose again (2005–2020; APC: 0.9%). Males consistently exhibited higher AAMRs than females (Average APC: 0.7 vs. 0.19). Rural males had the highest AAMR (9.4), while urban females had the lowest (5.8). Racial disparities were stark: non-Hispanic Black males had the highest AAMR (12.3), followed by NH Black females (9.3). States with the highest mortality included Mississippi (11.2), Arkansas (9.4), Louisiana (9.3), and Oklahoma (9.0).
Discussion: The rising CRC mortality among adults in midlife reflects a concerning trend that may be driven by multiple structural and behavioral determinants. The disproportionate burden observed in southern and rural states suggests a correlation with reduced health literacy, delayed symptom recognition, and inadequate access to advanced care. These barriers likely contribute to late-stage diagnosis and poor outcomes. Public health efforts must prioritize early education, improved healthcare infrastructure, and more equitable access to screening. Further studies are needed to understand these trends and guide effective intervention strategies to reverse rising mortality rates.
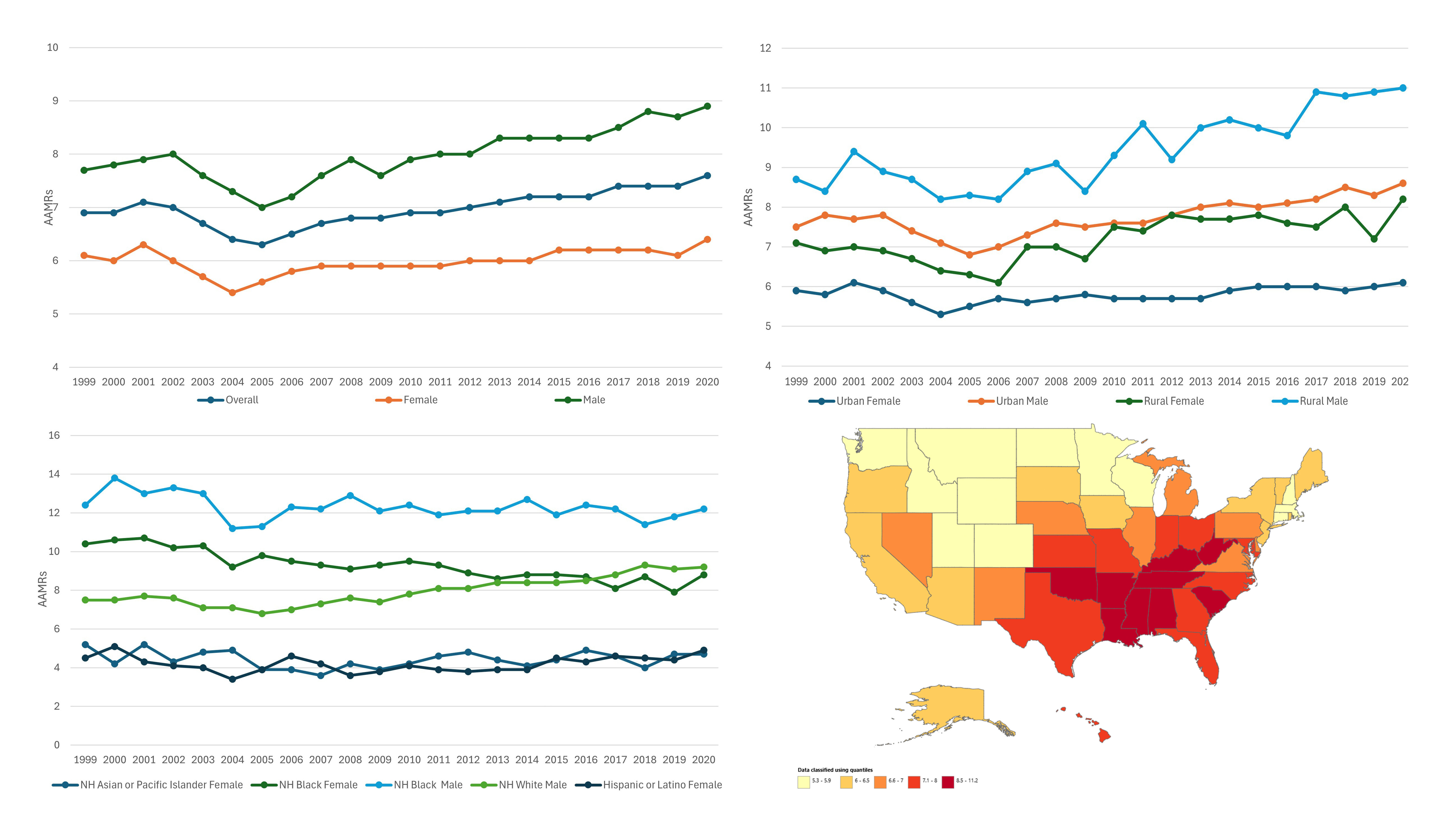
Figure: Graphical representation of Age Adjusted mortality based of CRC
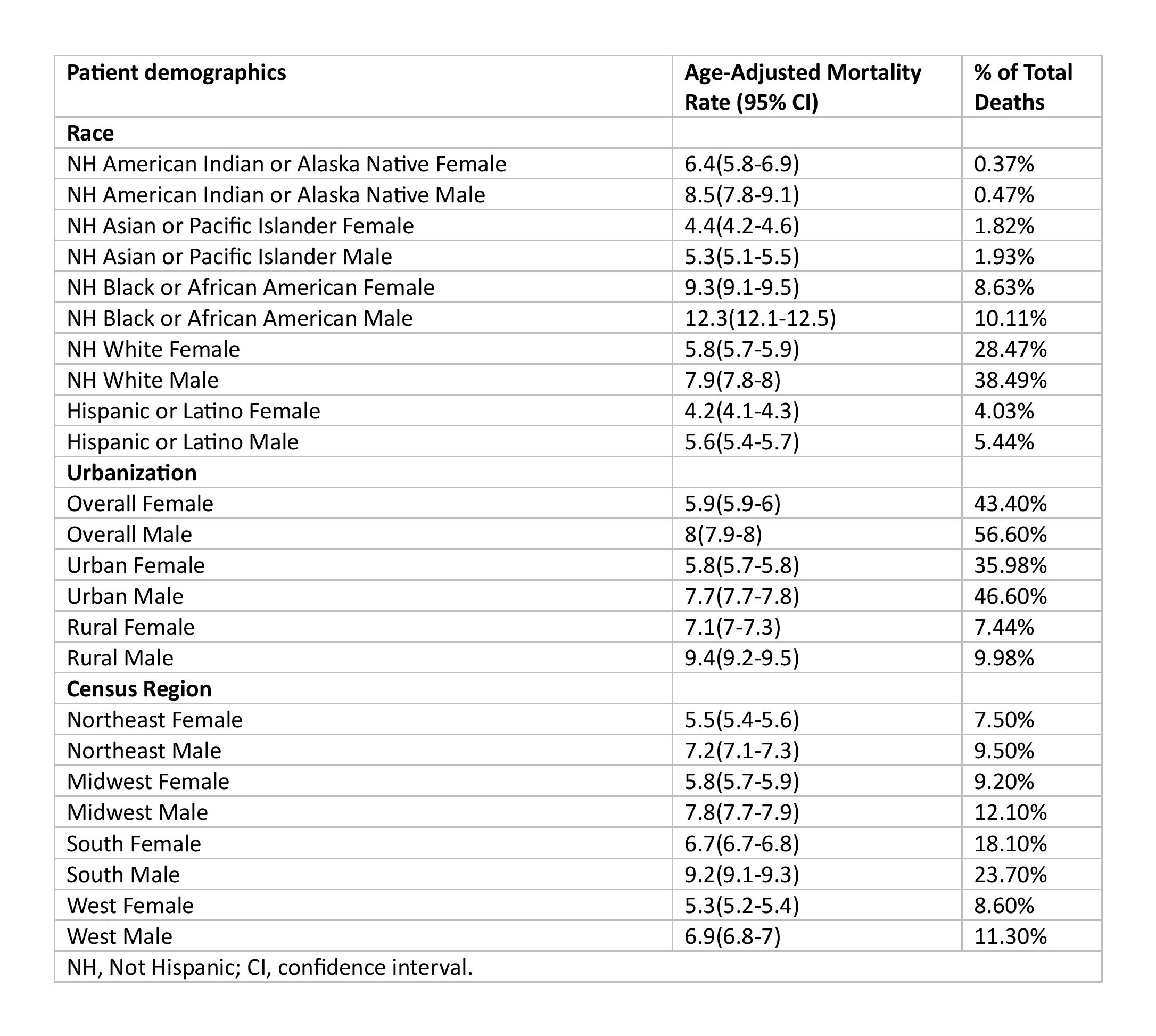
Figure: Age Adjusted Mortality based on race, geographical distribution, urbanization and gender
Disclosures:
Zainab Rafaqat indicated no relevant financial relationships.
Umar Abdul Rehman Khalid indicated no relevant financial relationships.
Ali Akram Qureshi indicated no relevant financial relationships.
Muhammad Faiq Akram indicated no relevant financial relationships.
Christopher Bouvette indicated no relevant financial relationships.
Jalal Gondal indicated no relevant financial relationships.
Ijlal Ali indicated no relevant financial relationships.
Zainab Rafaqat, MD1, Umar Abdul Rehman Khalid, MBBS2, Ali Akram Qureshi, MBBS2, Muhammad Faiq Akram, MBBS3, Christopher Bouvette, MD4, Jalal Gondal, MD4, Ijlal Akbar. Ali, MD5. P0465 - Rising Colorectal Cancer Mortality Among US Adults Aged 35-54 (1999-2020): A Nationwide Analysis of Disparities by Race, Region, and Urbanization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
