Sunday Poster Session
Category: Colon
P0422 - Gutted by Proteins: A Rare Case of GI Amyloidosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Shreya Deshpande (she/her/hers)
SS Institute of Medical Sciences and Research Center, Davangere
Bangalore, Karnataka, India
Presenting Author(s)
Award: ACG Presidential Poster Award
Shreya Deshpande, 1, Nikita Desai, MD2, Dorian Willhite, MD2, Nikrad Shahnavaz, MD3
1SS Institute of Medical Sciences and Research Center, Davangere, Bangalore, Karnataka, India; 2Emory University School of Medicine, Atlanta, GA; 3Emory University, Atlanta, GA
Introduction: Amyloidosis is a rare disease involving deposition of abnormal proteins in various organs. Gastrointestinal (GI) amyloidosis is a rare manifestation of systemic amyloidosis. We report a patient presenting with rectal bleeding found to have large submucosal nodules in the right colon and terminal ileum consistent with GI amyloidosis.
Case Description/
Methods: A 51-year-old male with a history of cirrhosis and IgG lambda plasma cell dyscrasia presented with hematochezia and drop in hemoglobin. Colonoscopy demonstrated multiple large submucosal lesions in the right side of the colon and terminal ileum, some with superficial ulcerations occupying more than half of the lumen. Pathology revealed amorphous material consistent with amyloid confirmed by Congo red staining. Given the remote history of minimal alcohol consumption, other causes of liver disease were explored. Liver biopsy revealed advanced fibrosis with an atypical plasma cell infiltrate, positive for lambda, CD3 and CD20 L26 markers, suggesting the possibility of hepatic amyloidosis. A CT scan showed partially calcified lymphadenopathy and mass like thickening of the right colon, consistent with amyloid.
Discussion: Amyloidosis results from accumulation of abnormal extracellular proteins. Primary amyloidosis is associated with multiple myeloma, while secondary amyloidosis develops in response to chronic inflammation or infection. GI amyloidosis is exceedingly rare, with manifestations of GI bleeding, malabsorption and protein losing gastroenteropathy. Based on our review of existing literature, this is the first reported case of GI amyloidosis presenting with multiple large submucosal nodular lesions in the colon. GI involvement occurs in only 3-8% of AL amyloidosis. To date, there are no established treatment guidelines for this disease and multidisciplinary care with a hematologist is recommended. This case highlights the importance of considering atypical causes of GI bleeding in patients with a history of plasma cell disorders. A multidisciplinary approach with tissue confirmation of amyloidosis is most appropriate while managing these cases.
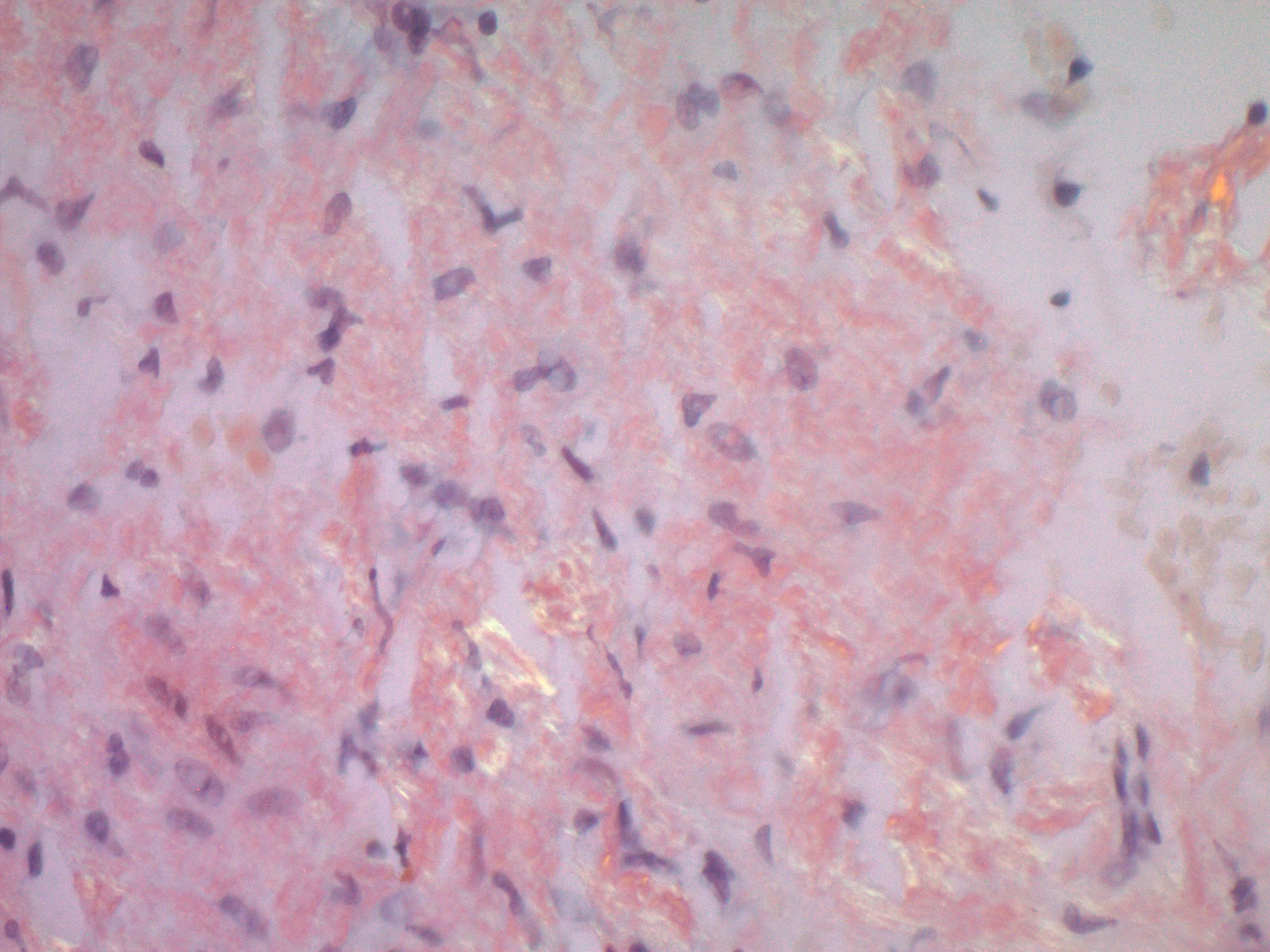
Figure: The H&E prepped slide showed fragments of benign colonic mucosa with an extracellular, amorphous, pale eosinophilic area of interest. The Congo Red stain in the same area shows reddish extracellular deposits, and with polarized light, the same deposits are highlighted by apple green birefringence. These findings are consistent with amyloid deposits.
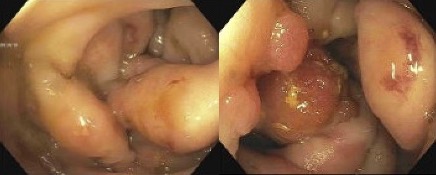
Figure: The colonoscopy images show multiple submucosal nodules in the terminal ileum and cecum to transverse colon; some with superficial ulcerations.
Disclosures:
Shreya Deshpande indicated no relevant financial relationships.
Nikita Desai indicated no relevant financial relationships.
Dorian Willhite indicated no relevant financial relationships.
Nikrad Shahnavaz indicated no relevant financial relationships.
Shreya Deshpande, 1, Nikita Desai, MD2, Dorian Willhite, MD2, Nikrad Shahnavaz, MD3. P0422 - Gutted by Proteins: A Rare Case of GI Amyloidosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Shreya Deshpande, 1, Nikita Desai, MD2, Dorian Willhite, MD2, Nikrad Shahnavaz, MD3
1SS Institute of Medical Sciences and Research Center, Davangere, Bangalore, Karnataka, India; 2Emory University School of Medicine, Atlanta, GA; 3Emory University, Atlanta, GA
Introduction: Amyloidosis is a rare disease involving deposition of abnormal proteins in various organs. Gastrointestinal (GI) amyloidosis is a rare manifestation of systemic amyloidosis. We report a patient presenting with rectal bleeding found to have large submucosal nodules in the right colon and terminal ileum consistent with GI amyloidosis.
Case Description/
Methods: A 51-year-old male with a history of cirrhosis and IgG lambda plasma cell dyscrasia presented with hematochezia and drop in hemoglobin. Colonoscopy demonstrated multiple large submucosal lesions in the right side of the colon and terminal ileum, some with superficial ulcerations occupying more than half of the lumen. Pathology revealed amorphous material consistent with amyloid confirmed by Congo red staining. Given the remote history of minimal alcohol consumption, other causes of liver disease were explored. Liver biopsy revealed advanced fibrosis with an atypical plasma cell infiltrate, positive for lambda, CD3 and CD20 L26 markers, suggesting the possibility of hepatic amyloidosis. A CT scan showed partially calcified lymphadenopathy and mass like thickening of the right colon, consistent with amyloid.
Discussion: Amyloidosis results from accumulation of abnormal extracellular proteins. Primary amyloidosis is associated with multiple myeloma, while secondary amyloidosis develops in response to chronic inflammation or infection. GI amyloidosis is exceedingly rare, with manifestations of GI bleeding, malabsorption and protein losing gastroenteropathy. Based on our review of existing literature, this is the first reported case of GI amyloidosis presenting with multiple large submucosal nodular lesions in the colon. GI involvement occurs in only 3-8% of AL amyloidosis. To date, there are no established treatment guidelines for this disease and multidisciplinary care with a hematologist is recommended. This case highlights the importance of considering atypical causes of GI bleeding in patients with a history of plasma cell disorders. A multidisciplinary approach with tissue confirmation of amyloidosis is most appropriate while managing these cases.
Figure: The H&E prepped slide showed fragments of benign colonic mucosa with an extracellular, amorphous, pale eosinophilic area of interest. The Congo Red stain in the same area shows reddish extracellular deposits, and with polarized light, the same deposits are highlighted by apple green birefringence. These findings are consistent with amyloid deposits.
Figure: The colonoscopy images show multiple submucosal nodules in the terminal ileum and cecum to transverse colon; some with superficial ulcerations.
Disclosures:
Shreya Deshpande indicated no relevant financial relationships.
Nikita Desai indicated no relevant financial relationships.
Dorian Willhite indicated no relevant financial relationships.
Nikrad Shahnavaz indicated no relevant financial relationships.
Shreya Deshpande, 1, Nikita Desai, MD2, Dorian Willhite, MD2, Nikrad Shahnavaz, MD3. P0422 - Gutted by Proteins: A Rare Case of GI Amyloidosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

