Sunday Poster Session
Category: Colon
P0419 - Enterocolonic Fistulization in Advanced Colon Adenocarcinoma: A Case Report
- NN
Nora Novikova, BA
Creighton University School of Medicine
Phoenix, AZ
Presenting Author(s)
1Creighton University School of Medicine, Phoenix, AZ; 2Creighton University School of Medicine, Mesa, AZ; 3Dignity Health, Phoenix, AZ
Introduction: Colorectal cancer (CRC) has many complications including bowel obstruction, however fistula formation is not a common finding. Fistulas may develop post operatively, or as a result of cancer therapies, such as anti-angiogenic agents like Bevacizumab which impairs tissue healing. Clinically, this presents as specific symptoms depending on the organ it is forming a tract with. We present a rare case of CRC with an enterocolonic fistula discovered at the time of diagnosis.
Case Description/
Methods:
A 77-year-old woman with no significant medical history presented to the emergency department with ten days of nausea, vomiting, and non-bloody diarrhea. She had an unremarkable colonoscopy approximately five years prior and denied recent hospitalizations, antibiotic use, unintentional weight loss, changes in stool caliber, or a family history of CRC. On arrival, her vitals were stable, and pertinent labs include a WBC 20.3 cells/uL, and hemoglobin 9.2 g/dL. Computed tomography (CT) of the abdomen and pelvis revealed a large proximal transverse colonic mass, measuring 12 x 10.7 x 7.8 cm. There was no evidence of free fluid or lymphadenopathy, and CT chest was negative for metastasis. Colonoscopy revealed a long segment of circumferential deep colonic ulceration with irregular mucosa, and necrotic areas extending from the splenic to the hepatic flexure. Proximal to the ulcerated area, there was an abnormal connection between the colon and small bowel, consistent with an enterocolonic fistula. The cecum and ascending colon appeared normal. The patient underwent an extended right colectomy with primary anastomosis and small bowel resection. Intraoperatively, the mass showed fistulization to the jejunum, extended into the base of the small bowel mesentery, and showed dense adherence along the greater curvature of the stomach. Pathology confirmed invasive adenocarcinoma with mucinous features. Unfortunately, repeat imaging revealed concern for hepatic metastasis and the patient is awaiting chemotherapy.
Discussion: Fistula formation as an initial presentation of colon cancer is rare, and associated with significant morbidity, infection, and malnutrition. This occurs primarily through direct invasion of the tumor. Additionally, other published cases report fistulization between other organs such as the bladder and skin, and less commonly between two segments of bowel. In these instances, fistula formation should be recognized as a perforation or locally advanced cancer.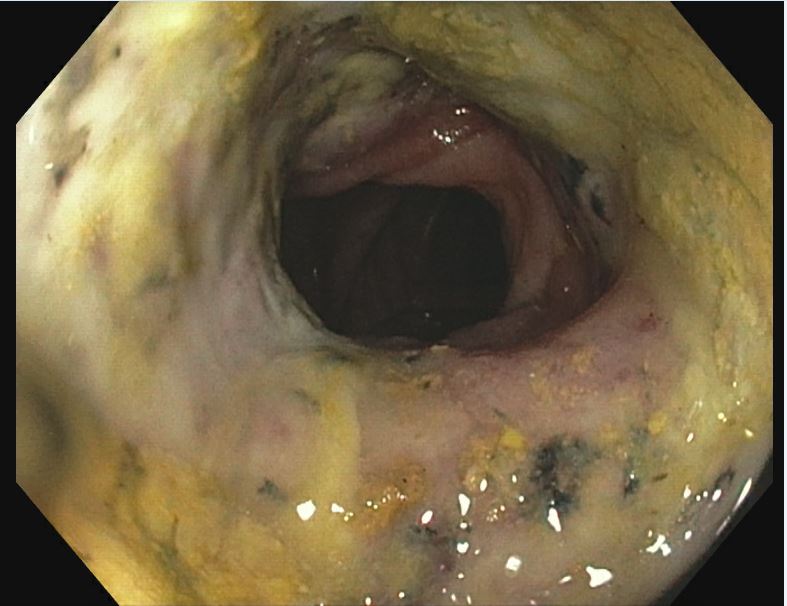
Figure: Colonoscopy showing deep ulceration and necrosis in the transverse colon.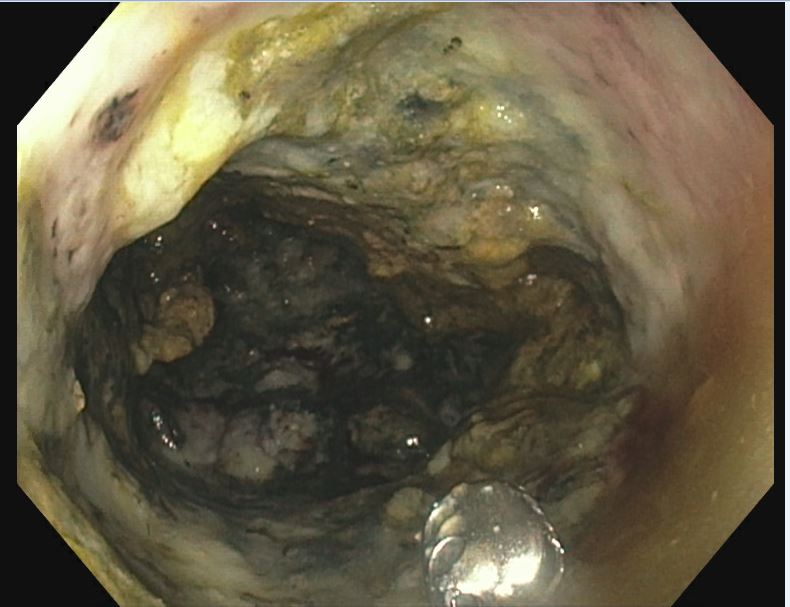
Figure: Colonoscopy showing an abnormal opening in the colonic wall, consistent with an enterocolonic fistula.
Disclosures:
Nora Novikova indicated no relevant financial relationships.
Ericka Charley indicated no relevant financial relationships.
Shahab Aftahi indicated no relevant financial relationships.
Aida Rezaie indicated no relevant financial relationships.
Nora Novikova, BA1, Ericka Charley, MD2, Shahab Aftahi, MD3, Aida Rezaie, MD1. P0419 - Enterocolonic Fistulization in Advanced Colon Adenocarcinoma: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
