Sunday Poster Session
Category: Colon
P0388 - The Intersection of CMV and IBD in an Immunosuppressed Host
Justin Lu, MS (he/him/his)
Northeast Ohio Medical University
Rootstown, OH
Presenting Author(s)
1Northeast Ohio Medical University, Rootstown, OH; 2Case Western Reserve University / MetroHealth, Cleveland, OH
Introduction:
Inflammatory bowel disease (IBD), comprising ulcerative colitis (UC) and Crohn’s disease (CD), is a chronic immune-mediated condition characterized by relapsing inflammation of the gastrointestinal tract. However, cytomegalovirus (CMV) poses a diagnostic challenge in patients with IBD due to its mimicking symptoms. We present a case of CMV colitis in an individual with no known prior IBD.
Case Description/
Methods: A 66-year-old woman with hyperlipidemia, hypertension, type 2 diabetes mellitus, and psoriatic arthritis on methotrexate, golimumab, and folate (previously Humira) presents with sudden explosive diarrhea and rectal bleeding. Prior colonoscopy screening in 2014 revealed normal mucosa with several tubular adenomas. CT scan showed colonic wall thickening and pericolonic inflammation, and she was treated empirically for infectious colitis. Persistent symptoms prompted re-evaluation with elevated calprotectin at 4230. A colonoscopy showed diffuse circumferential ulceration from the descending to distal sigmoid colon. Biopsies revealed acute inflammation of undetermined chronicity. A prednisone taper was started, but continued symptoms prompted readmission. Repeat calprotectin increased to >8000 mcg/g. Flexible sigmoidoscopy showed severe necrotic ulceration throughout the sigmoid colon. Biopsies revealed ulceration, granulation tissue, and lymphoplasmacytic infiltrate with epithelial atypia with suspicion of CMV. IV ganciclovir was initiated and transitioned to oral valganciclovir with partial improvement. Repeat colonoscopy one month later showed improved ulceration in the descending colon and sigmoid with ongoing friability. Biopsies showed chronic colitis with focal active inflammation, most pronounced in the descending colon. No features of microscopic or collagenous colitis noted. The terminal ileum showed chronic inflammation but no active enteritis. CMV immunohistochemistry was negative, consistent with transient CMV reactivation response. Thus, her Simponi (golimumab) frequency was increased to biweekly, leading to normalization of CRP and calprotectin improvement from 2800 to 2000. However, residual symptoms prompted a switch to Risankizumab.
Discussion:
This case illustrates the diagnostic and therapeutic challenges of distinguishing CMV colitis from IBD flare in immunosuppressed patients, the importance of tissue-based CMV testing, and the need for both antiviral and optimized immunosuppressive therapy to achieve remission.
Figure: Descending colon on initial colonoscopy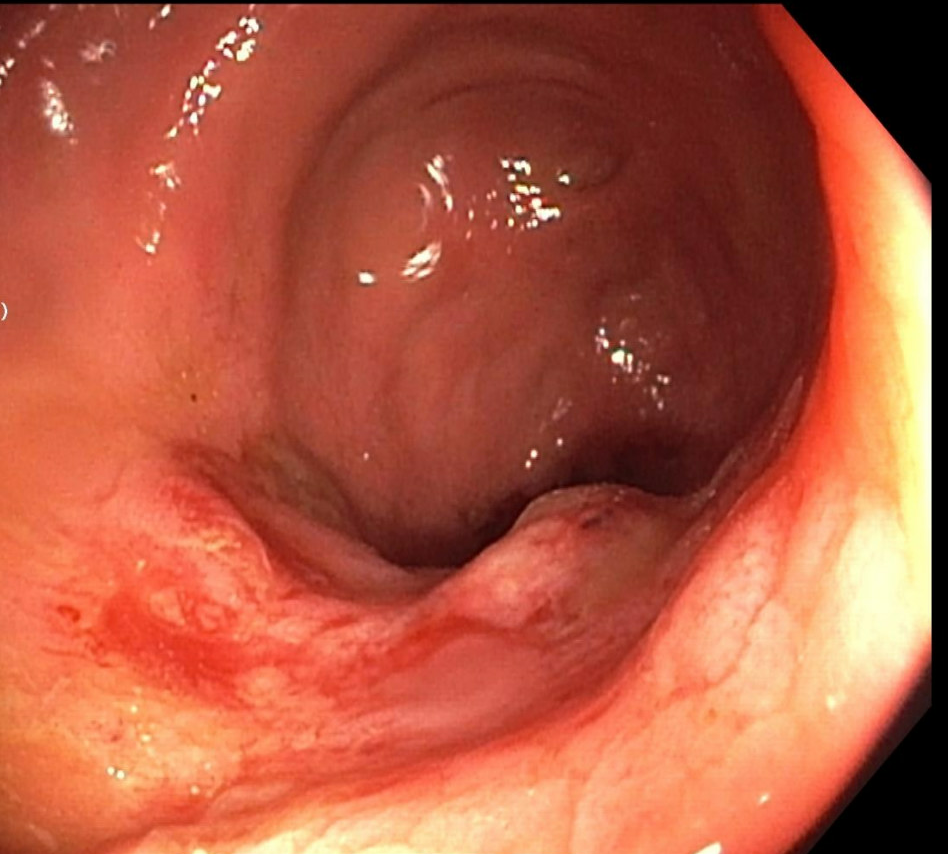
Figure: Descending colon after CMV treatment and increase in golimumab.
Disclosures:
Justin Lu indicated no relevant financial relationships.
Adrian Lindsey indicated no relevant financial relationships.
Justin Lu, MS1, Adrian S. Lindsey, MD2. P0388 - The Intersection of CMV and IBD in an Immunosuppressed Host, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
