Sunday Poster Session
Category: Colon
Disseminated <i>Myobacterium</i> Tuberculosis With Gastrointestinal Involvement: A Case Report of Colonic Tuberculoma
P0387 - Disseminated Myobacterium Tuberculosis With Gastrointestinal Involvement: A Case Report of Colonic Tuberculoma
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JT
Julianna Tantum, DO
Lankenau Medical Center
Wynnewood, PA
Presenting Author(s)
Julianna Tantum, DO, Erin Hollis, DO, Lauren Davis, DO, Nicole Albert, DO
Lankenau Medical Center, Wynnewood, PA
Introduction: Mycobacterium tuberculosis (TB) most commonly affects the lungs, and involvement of the GI tract is rare, with the terminal ileum the most affected site. Colonic involvement most commonly affects the right colon and can be seen as an isolated disease or a part of a disseminated infection.
Case Description/
Methods: This is a 38-year-old female with no PMH who presented with dry cough, painful axillary lymphadenopathy, weight loss, night sweats, fevers and anorexia. No changes in bowel movements or history of colon cancer. No prior endoscopic evaluation. She immigrated to the US from Africa about 10 years prior. On presentation, patient febrile to 100.3 F but otherwise stable. Labs notable for hemoglobin 9.7 (MCV 76.2), iron saturation 9, total protein 10.5, albumin 3.8, normal liver enzymes. CT chest abdomen pelvis with IV contrast showed mediastinal, bilateral hilar, axillary, supraclavicular lymphadenopathy, multiple pulmonary nodules, along with thickening of the cecal wall with suggestion of an underlying mass measuring 4.2 x 3.7 x 3.9 cm. She underwent sputum analysis and right axillary lymph node excision showing necrotizing granulomas with acid fast microorganisms consistent with TB. She started TB therapy. Labs also positive for HIV. She underwent colonoscopy revealing a large fungating, non-obstructing mass in the cecum (Image 1A). Biopsies showed moderate active and chronic colitis with focal crypt abscess and poorly formed granuloma with acid fast rods, no evidence of malignancy (Images 1B-D). She was discharged with HIV and TB therapy with close follow up with plan for repeat imaging to ensure resolution of mass after TB treatment.
Discussion: Colonic TB is rare and can be seen in isolated or disseminated TB. Patients may have systemic symptoms such as fevers, chills, and night sweats or abdominal specific symptoms of changes in bowel habits and abdominal pain. Colonic TB can be seen on imaging as an isolated mass, wall thickening or structuring disease and can easily be mistaken for malignancy, IBD, infectious or ischemic colitis, making direct visualization with colonoscopy and biopsy imperative. Histologically, nonspecific inflammation, granulomas, and acid-fast bacilli can help confirm the diagnosis and help differentiate from malignancy. Treatment involves therapy for TB with most cases resolving after a course of TB treatment. Repeat imaging and colonoscopy can be considered to ensure resolution, but specific guidelines on follow up are not well established.
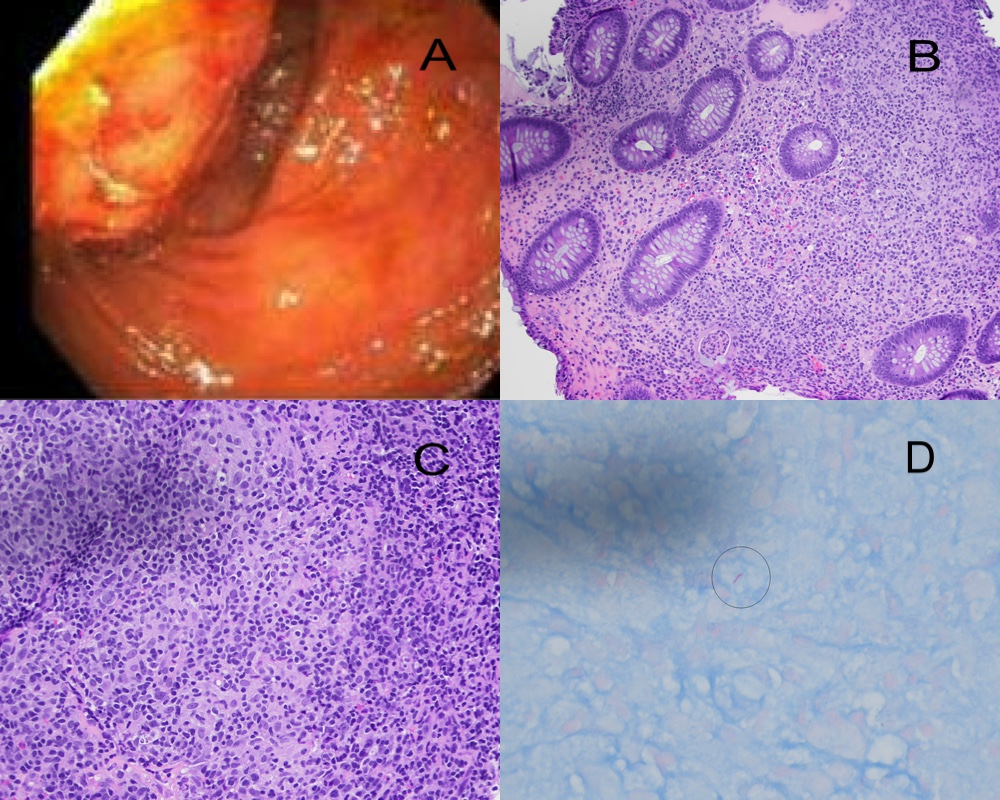
Figure: Image 1. A. Image from colonoscopy showing a large fungating, non-obstructing cecal mass. B. Cecal mass histology on H&E stain showing moderate active/chronic colitis with focal crypt abscess. C. Histology on H&E stain showing poorly formed granulomas. D. AFB stain showing rare acid-fast rods.
Disclosures:
Julianna Tantum indicated no relevant financial relationships.
Erin Hollis indicated no relevant financial relationships.
Lauren Davis indicated no relevant financial relationships.
Nicole Albert indicated no relevant financial relationships.
Julianna Tantum, DO, Erin Hollis, DO, Lauren Davis, DO, Nicole Albert, DO. P0387 - Disseminated <i>Myobacterium</i> Tuberculosis With Gastrointestinal Involvement: A Case Report of Colonic Tuberculoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Lankenau Medical Center, Wynnewood, PA
Introduction: Mycobacterium tuberculosis (TB) most commonly affects the lungs, and involvement of the GI tract is rare, with the terminal ileum the most affected site. Colonic involvement most commonly affects the right colon and can be seen as an isolated disease or a part of a disseminated infection.
Case Description/
Methods: This is a 38-year-old female with no PMH who presented with dry cough, painful axillary lymphadenopathy, weight loss, night sweats, fevers and anorexia. No changes in bowel movements or history of colon cancer. No prior endoscopic evaluation. She immigrated to the US from Africa about 10 years prior. On presentation, patient febrile to 100.3 F but otherwise stable. Labs notable for hemoglobin 9.7 (MCV 76.2), iron saturation 9, total protein 10.5, albumin 3.8, normal liver enzymes. CT chest abdomen pelvis with IV contrast showed mediastinal, bilateral hilar, axillary, supraclavicular lymphadenopathy, multiple pulmonary nodules, along with thickening of the cecal wall with suggestion of an underlying mass measuring 4.2 x 3.7 x 3.9 cm. She underwent sputum analysis and right axillary lymph node excision showing necrotizing granulomas with acid fast microorganisms consistent with TB. She started TB therapy. Labs also positive for HIV. She underwent colonoscopy revealing a large fungating, non-obstructing mass in the cecum (Image 1A). Biopsies showed moderate active and chronic colitis with focal crypt abscess and poorly formed granuloma with acid fast rods, no evidence of malignancy (Images 1B-D). She was discharged with HIV and TB therapy with close follow up with plan for repeat imaging to ensure resolution of mass after TB treatment.
Discussion: Colonic TB is rare and can be seen in isolated or disseminated TB. Patients may have systemic symptoms such as fevers, chills, and night sweats or abdominal specific symptoms of changes in bowel habits and abdominal pain. Colonic TB can be seen on imaging as an isolated mass, wall thickening or structuring disease and can easily be mistaken for malignancy, IBD, infectious or ischemic colitis, making direct visualization with colonoscopy and biopsy imperative. Histologically, nonspecific inflammation, granulomas, and acid-fast bacilli can help confirm the diagnosis and help differentiate from malignancy. Treatment involves therapy for TB with most cases resolving after a course of TB treatment. Repeat imaging and colonoscopy can be considered to ensure resolution, but specific guidelines on follow up are not well established.
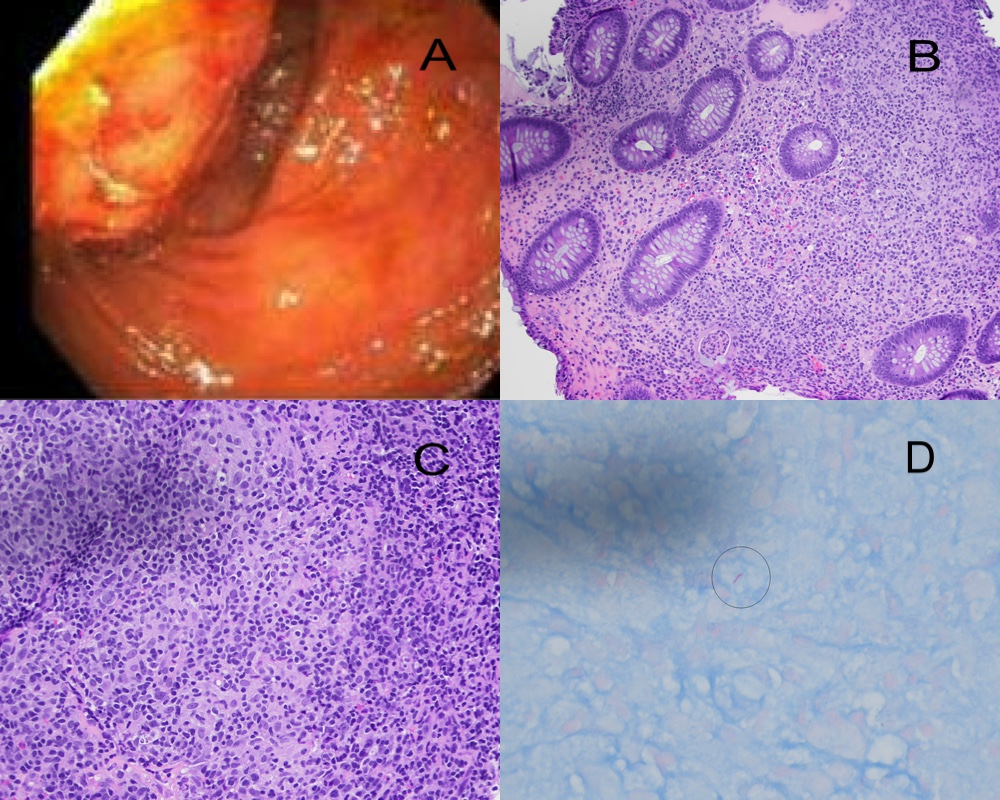
Figure: Image 1. A. Image from colonoscopy showing a large fungating, non-obstructing cecal mass. B. Cecal mass histology on H&E stain showing moderate active/chronic colitis with focal crypt abscess. C. Histology on H&E stain showing poorly formed granulomas. D. AFB stain showing rare acid-fast rods.
Disclosures:
Julianna Tantum indicated no relevant financial relationships.
Erin Hollis indicated no relevant financial relationships.
Lauren Davis indicated no relevant financial relationships.
Nicole Albert indicated no relevant financial relationships.
Julianna Tantum, DO, Erin Hollis, DO, Lauren Davis, DO, Nicole Albert, DO. P0387 - Disseminated <i>Myobacterium</i> Tuberculosis With Gastrointestinal Involvement: A Case Report of Colonic Tuberculoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
