Sunday Poster Session
Category: Colon
P0384 - Metastatic High-Grade Neuroendocrine Tumor of the Colon: A Rare Disease With Poor Outcome
- RR
Rehan Rafiq, MD, FACG (he/him/his)
Mercy Hospital Jefferson
Festus, MO
Presenting Author(s)
1Mercy Hospital Jefferson, Festus, MO; 2Maryville University, Chesterfield, MO; 3Parkway West High School, Ballwin MO, Chesterfield, MO; 4Department of Pathology, Christian Hospital Northeast, St. Louis, MO; 5University of Missouri Columbia, Columbia, MO
Introduction: Neuroendocrine carcinoma of colorectum (NET) is rare. It arises from gut, pancreas and lung cells1, 2. Clery et al. first reported high grade neuroendocrine carcinoma (HGNEC) of colorectum 3. Incidence is 2 per million person-years4. Classification is based on mitotic rate and/or Ki-67 labeling index4. 20 mitoses/ 10 high power fields or Ki- 67 index of more than 20% indicates poorly differentiated NET 5. Treatment includes surgery and chemoradiation for localized disease and chemotherapy for metastatic disease6-8. Median survival is 14.74. We present a case of HGNEC of the colon metastatic to the liver.
Case Description/
Methods:
A 53-year-old African American man presented with abdominal pain, diarrhea and weight loss. Personal and family history was unremarkable. He never had a screening colonoscopy. Physical examination was unremarkable. Labs showed anemia, leukocytosis, and elevated alkaline phosphatase. A CT scan showed liver metastasis. Colonoscopy showed an obstructing mass in the splenic flexure. Biopsy showed HGNEC. Tumor stained for cam 5.2, synaptophysin and chromogranin. Ki-I 67 was 90%. Left hemicolectomy and biopsy of hepatic metastasis was performed. He received platinum-based chemotherapy. Patient developed hyperbilirubinemia with significant metastatic disease on repeat CT. Patient pursued comfort care, and he passed away.
Discussion:
HGNEC constitutes 0.6% of all malignant colorectal cancers9. The median age at diagnosis is 65 years, predominantly in Caucasians10. Our patient was African American and presented at a younger age. Histologically, they are similar to small cell lung cancer (SCLC)4. Unlike SCLC, smoking is not a risk factor4. They are non-hormone producing and present with metastatic disease 11. They may be associated with an adenoma and familial adenomatous polyposis4,12. Early-stage tumors are treated with surgery and chemotherapy13. Advanced stages treated with combined chemotherapy and surgical resection shows better outcome10. Our patient did poorly with this therapeutic approach. The chemotherapeutic regimen is platinum-based14, 15. Lower Ki-67 (< 55%) are associated with poor response to chemotherapy10. Liver metastases are treated with surgery, trans arterial treatments16. Our patient responded poorly despite having high Ki-67 levels ( >90%). Patient and tumor factors may be important in response to chemotherapy. A screening colonoscopy might have changed the patient's outcome. A dedicated database regarding this disease may improve patient's outcome.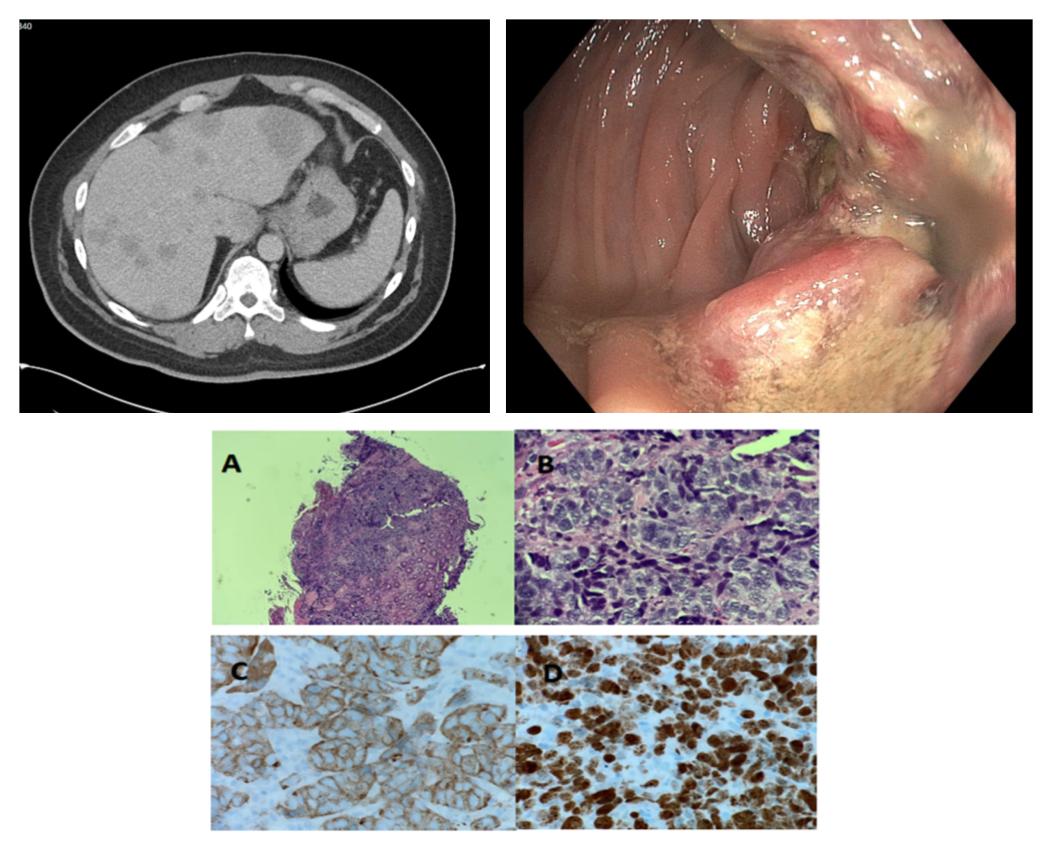
Figure: Figure 1 (top left): CT scan showing liver metastasis.
Figure 2 (top right): colonoscopy showing splenic flexure mass.
Figure 3 (below):
[A] biopsy of colon mass showing a poorly differentiated aggressive appearing cellular infiltrate (40x).
[B]: high-power view of infiltrate showing poorly formed cohesive nests of epithelioid malignant cells with enlarged nuclei and dispersed chromatin (400x).
[C]: synaptophysin immunohistochemical stain showing fairty strong cytoplasmic positivity (400x).
[D]: Ki-67 immunohistochemical stain with a high proliferative index at 90-95% (400x).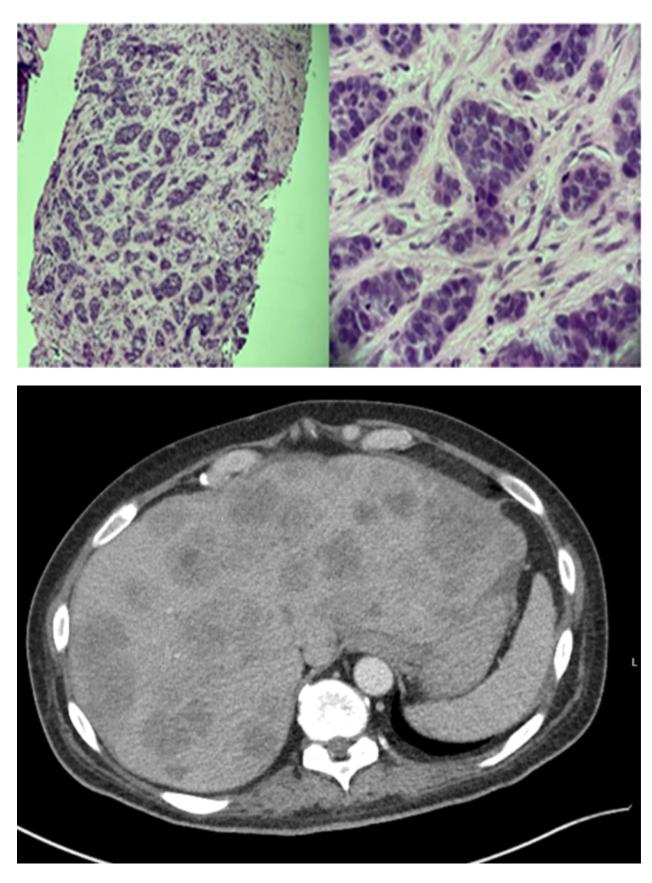
Figure: Figure 4 (top): liver biopsy showing an infiltrative carcinoma with a similar histology to the previous colon mass biopsy consistent with metastatic high grade neuroendocrine carcinoma (100x and 400x).
Figure 5 (bottom): post-chemotheropy CT scan showing progression of liver metastasis.
Disclosures:
Rehan Rafiq indicated no relevant financial relationships.
Ahmad Rafiq indicated no relevant financial relationships.
Umar Rafiq indicated no relevant financial relationships.
Michael VanVrancken indicated no relevant financial relationships.
Muhammad Yousaf indicated no relevant financial relationships.
Rehan Rafiq, MD, FACG1, Ahmad Rafiq, 2, Umar Rafiq, 3, Michael VanVrancken, MD4, Muhammad Yousaf, MD5. P0384 - Metastatic High-Grade Neuroendocrine Tumor of the Colon: A Rare Disease With Poor Outcome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
