Sunday Poster Session
Category: Colon
P0382 - When Immunosuppression Turns Inflammatory: Eosinophilic Colitis from Tacrolimus in a Liver Transplant Recipient
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Sarah Rahni, DO, MBA
Westchester Medical Center
Valhalla, NY
Presenting Author(s)
Sarah Rahni, DO, MBA1, Naveena Sunkara, MD1, Tsipora Huisman, MD2
1Westchester Medical Center, Valhalla, NY; 2WMC, New Rochelle, NY
Introduction: Eosinophilic colitis (EC) is an uncommon eosinophilic gastrointestinal disorder (EGID). The pathogenesis of EC is associated with eosinophilic dysregulation of T cell responses. EC has been described to occur with higher incidence after pediatric liver transplantation via an association with tacrolimus. This case describes an atypical presentation of colitis in an adult liver transplant recipient while on tacrolimus consistent with EGID.
Case Description/
Methods: A 49-year-old who underwent liver transplant 10 months prior presented with anemia noted in outpatient labs. He denied hematochezia, melena, shortness of breath, or lightheadedness. Further work up revealed a positive fecal occult blood test and hemoglobin of 5.8 g/dL (baseline 8.5 g/dL). Colonoscopy showed granular mucosa in the cecum and ascending colon. Pathology showed 150 eosinophils/HPF involving the lamina propria, intraepithelial eosinophils, and eosinophilic crypt abscesses in the cecum and ascending colon, up to 70 eosinophils/HPF involving the lamina propria and superficial muscularis mucosae in the sigmoid colon. No other abnormalities were found. The patient was discharged and readmitted 1 week later for shortness of breath, nausea, diarrhea, abdominal bloating, and discomfort. Blood work revealed an elevated peripheral eosinophil count of 8.5%. Work-up for other infectious or inflammatory processes was negative. Tacrolimus and prednisone were empirically discontinued and replaced by cyclosporine and mycophenolate. The patient’s symptoms resolved within one week. Five months later, repeat colonoscopy with biopsies showed normal colonic mucosa and pathology was negative for eosinophils.
Discussion: Our case underscores the need for awareness of tacrolimus’ potential to induce EGIDs. While this has been previously described in pediatric post-transplant patients, this case highlights the possible occurrence in adult patients on tacrolimus. Similarly to the pediatric population, discontinuation of tacrolimus resolved symptoms. Paradoxically, tacrolimus has been proposed as a potential therapy for steroid-refractory or diet-refractory EGIDs. Further research is needed to elucidate the mechanisms underlying tacrolimus-associated EC and to develop strategies for managing this condition in affected patient including resumption and choice of immunosuppressive therapies, as well as definitive endoscopic surveillance guidelines for EGIDs.
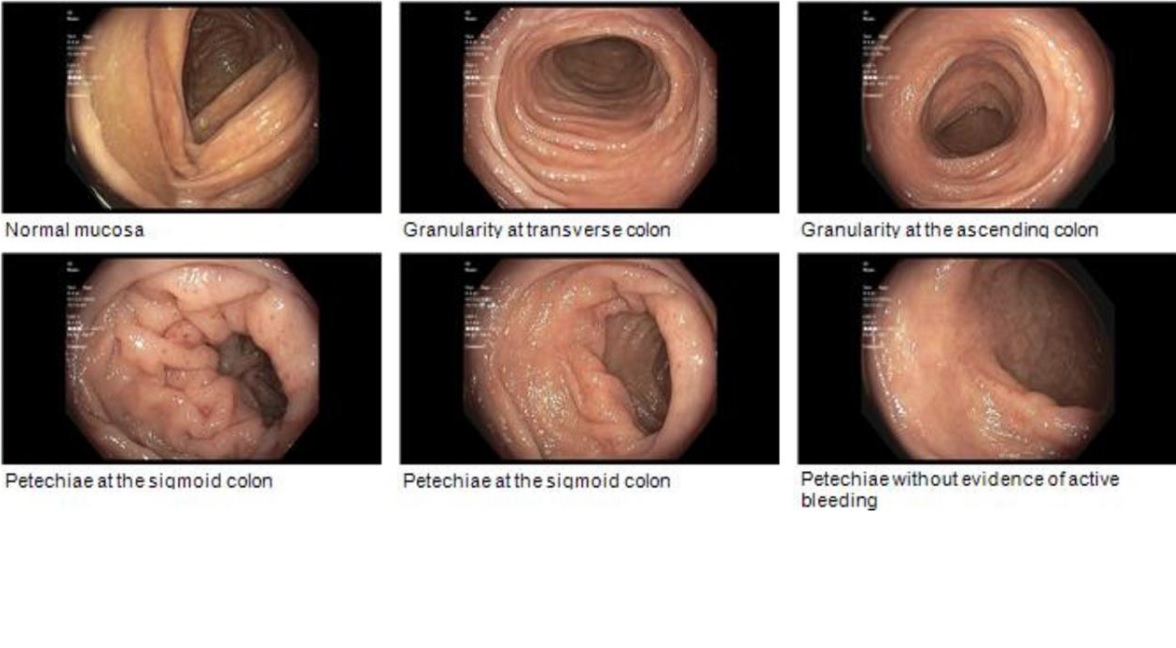
Figure: Appearance of granularity and petechiae on initial colonoscopy
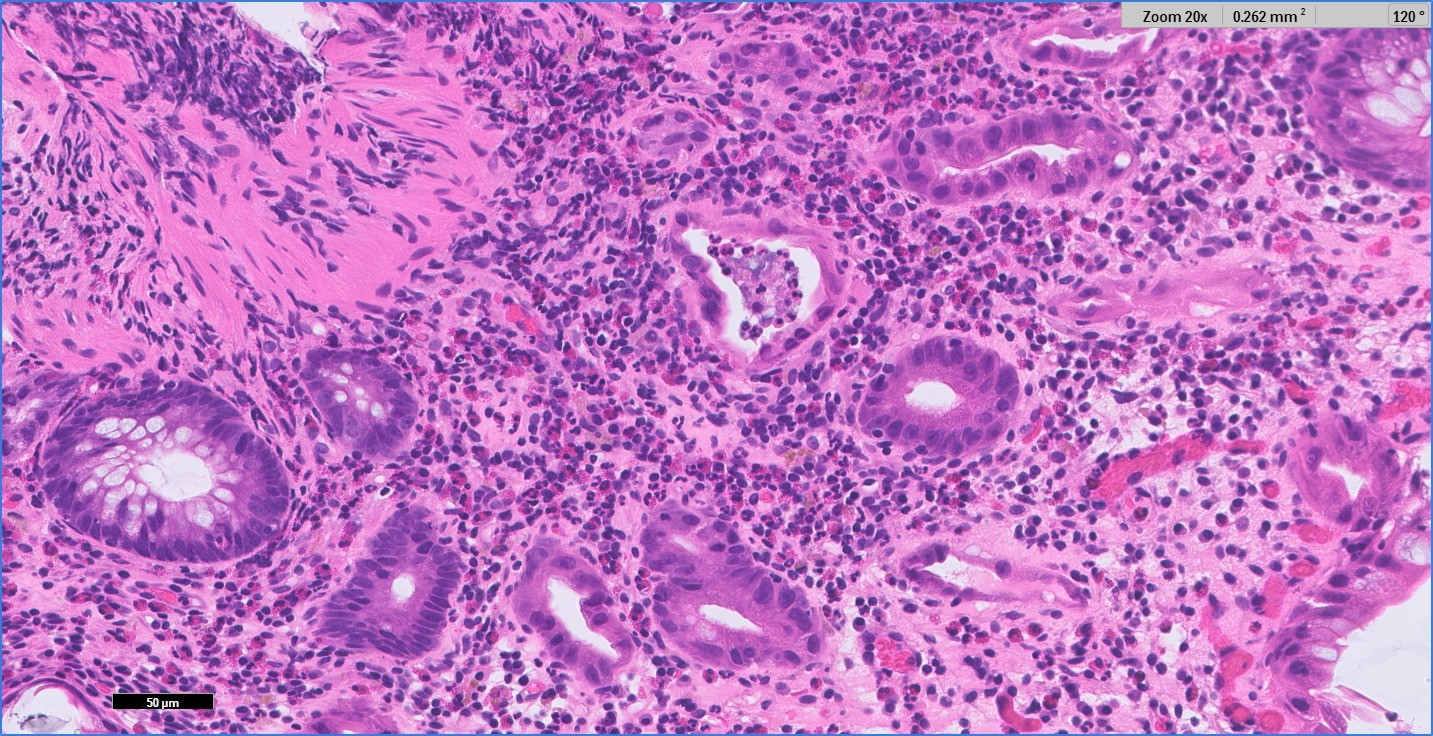
Figure: Pathology of biopsy showing diffuse eosinophilic infiltration
Disclosures:
Sarah Rahni indicated no relevant financial relationships.
Naveena Sunkara indicated no relevant financial relationships.
Tsipora Huisman indicated no relevant financial relationships.
Sarah Rahni, DO, MBA1, Naveena Sunkara, MD1, Tsipora Huisman, MD2. P0382 - When Immunosuppression Turns Inflammatory: Eosinophilic Colitis from Tacrolimus in a Liver Transplant Recipient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Westchester Medical Center, Valhalla, NY; 2WMC, New Rochelle, NY
Introduction: Eosinophilic colitis (EC) is an uncommon eosinophilic gastrointestinal disorder (EGID). The pathogenesis of EC is associated with eosinophilic dysregulation of T cell responses. EC has been described to occur with higher incidence after pediatric liver transplantation via an association with tacrolimus. This case describes an atypical presentation of colitis in an adult liver transplant recipient while on tacrolimus consistent with EGID.
Case Description/
Methods: A 49-year-old who underwent liver transplant 10 months prior presented with anemia noted in outpatient labs. He denied hematochezia, melena, shortness of breath, or lightheadedness. Further work up revealed a positive fecal occult blood test and hemoglobin of 5.8 g/dL (baseline 8.5 g/dL). Colonoscopy showed granular mucosa in the cecum and ascending colon. Pathology showed 150 eosinophils/HPF involving the lamina propria, intraepithelial eosinophils, and eosinophilic crypt abscesses in the cecum and ascending colon, up to 70 eosinophils/HPF involving the lamina propria and superficial muscularis mucosae in the sigmoid colon. No other abnormalities were found. The patient was discharged and readmitted 1 week later for shortness of breath, nausea, diarrhea, abdominal bloating, and discomfort. Blood work revealed an elevated peripheral eosinophil count of 8.5%. Work-up for other infectious or inflammatory processes was negative. Tacrolimus and prednisone were empirically discontinued and replaced by cyclosporine and mycophenolate. The patient’s symptoms resolved within one week. Five months later, repeat colonoscopy with biopsies showed normal colonic mucosa and pathology was negative for eosinophils.
Discussion: Our case underscores the need for awareness of tacrolimus’ potential to induce EGIDs. While this has been previously described in pediatric post-transplant patients, this case highlights the possible occurrence in adult patients on tacrolimus. Similarly to the pediatric population, discontinuation of tacrolimus resolved symptoms. Paradoxically, tacrolimus has been proposed as a potential therapy for steroid-refractory or diet-refractory EGIDs. Further research is needed to elucidate the mechanisms underlying tacrolimus-associated EC and to develop strategies for managing this condition in affected patient including resumption and choice of immunosuppressive therapies, as well as definitive endoscopic surveillance guidelines for EGIDs.
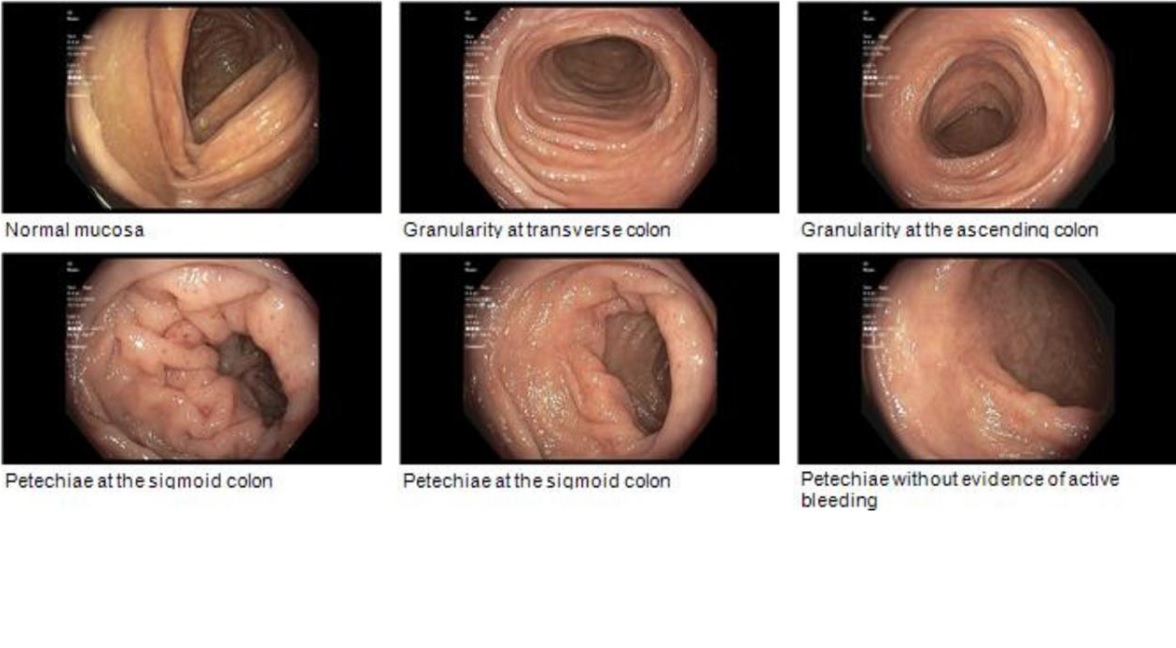
Figure: Appearance of granularity and petechiae on initial colonoscopy
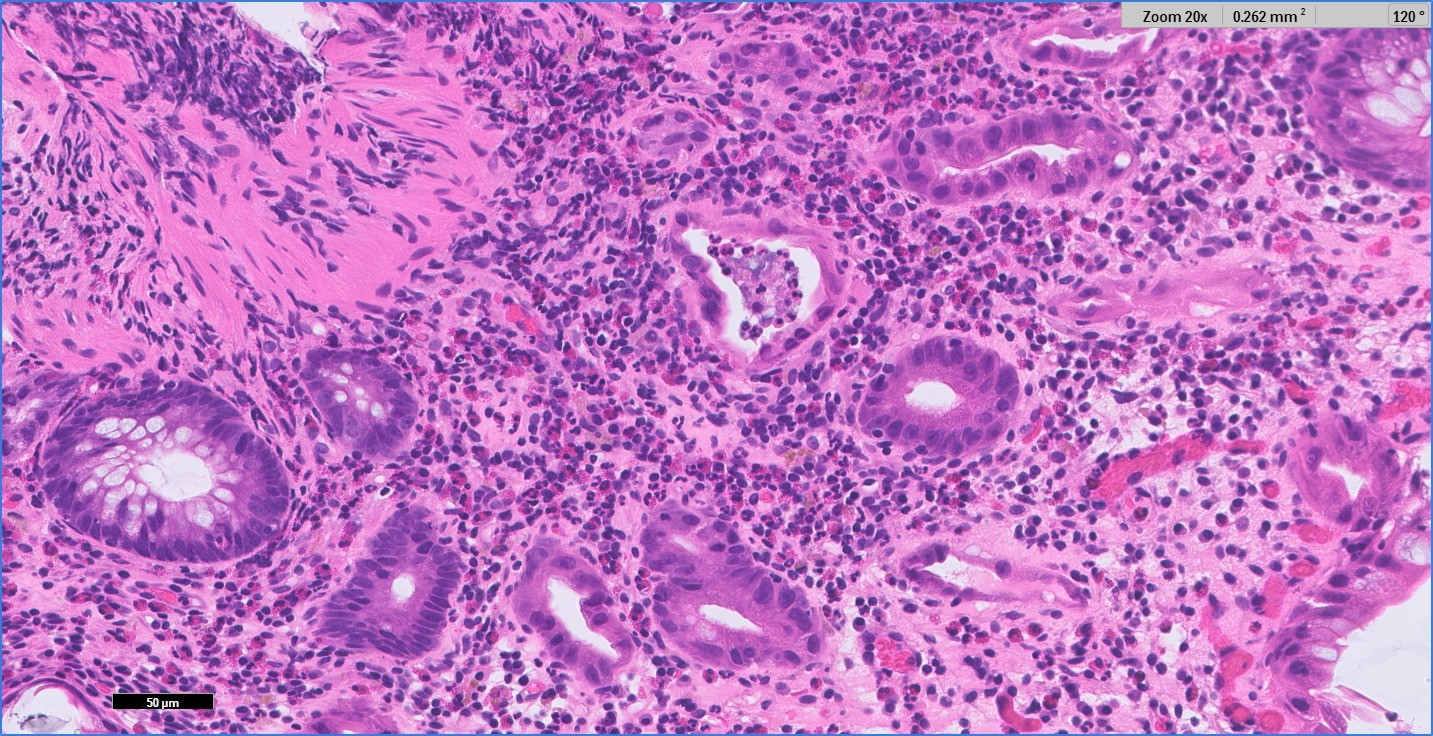
Figure: Pathology of biopsy showing diffuse eosinophilic infiltration
Disclosures:
Sarah Rahni indicated no relevant financial relationships.
Naveena Sunkara indicated no relevant financial relationships.
Tsipora Huisman indicated no relevant financial relationships.
Sarah Rahni, DO, MBA1, Naveena Sunkara, MD1, Tsipora Huisman, MD2. P0382 - When Immunosuppression Turns Inflammatory: Eosinophilic Colitis from Tacrolimus in a Liver Transplant Recipient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
