Sunday Poster Session
Category: Colon
P0381 - Gastrointestinal Mantle Cell Lymphoma: Diagnostic Value of Endoscopic and Histologic Correlation
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Sarah Rahni, DO, MBA
Westchester Medical Center
Valhalla, NY
Presenting Author(s)
Sarah Rahni, DO, MBA, Patrick Yang, MD, Naveena Sunkara, MD, Beth Schorr-Lesnick, MD, FACG
Westchester Medical Center, Valhalla, NY
Introduction: Mantle cell lymphoma (MCL) is a rare, aggressive B-cell non-Hodgkin lymphoma that can involve the gastrointestinal (GI) tract. GI presentations are often asymptomatic or mimic other conditions, complicating diagnosis. We present a case highlighting the diagnostic challenges and endoscopic findings of GI MCL.
Case Description/
Methods: A 77-year-old male presented with over 6 weeks of postprandial diarrhea ( >10 loose stools/day), with nausea, early satiety, epigastric abdominal pain, intermittent hematochezia, and significant weight loss. He denied fevers, chills, or night sweats. Family history was notable for colon cancer in his brother, unsure of age at time of diagnosis. CT abdomen revealed thickened bowel wall from the terminal ileum to ascending colon, extensive lymphadenopathy, and hepatosplenomegaly. Colonoscopy revealed submucosal masses in the right colon and ileocecal valve as well as thickened folds/bulky submucosal lesions. Pathology revealed atypical lymphoid cell proliferation. Immunohistochemical study revealed the lymphoid cells were positive for CD20, CD79a, CD5, CD43, BCL-2 and Cyclin D1. Bone marrow biopsy was performed and confirmed a surface lambda light chain restricted B cell population expressing CD19, CD20, and CD22, and co-expressing CD5, which is consistent with CD5 positive mature B cell non-Hodgkin lymphoma.
Discussion: MCL is a rare subtype of B-cell non-Hodgkin lymphoma, accounting for about 6% of cases. GI involvement occurs in up to 30% of patients, often presenting with nonspecific symptoms like diarrhea, weight loss, or GI bleeding, which may delay diagnosis. One of the most common primary GI presentations of MCL is lymphomatous polyposis, which typically manifests in the ascending colon, ileum and ileocecal region. These polyps may be sessile, polypoid, or mixed, and have ulceration; rarely, numerous polyps are present throughout the entire GI tract. In this case, endoscopic biopsies confirmed MCL, emphasizing the importance of thorough histologic evaluation when lymphoid infiltrates are present. MCL commonly involves the ileocecal region, as seen here, and may mimic inflammatory or infectious conditions. Prompt recognition and tissue diagnosis are critical, as MCL is aggressive and requires timely systemic therapy. This case underscores the need for high suspicion and comprehensive evaluation in elderly patients with atypical GI symptoms.
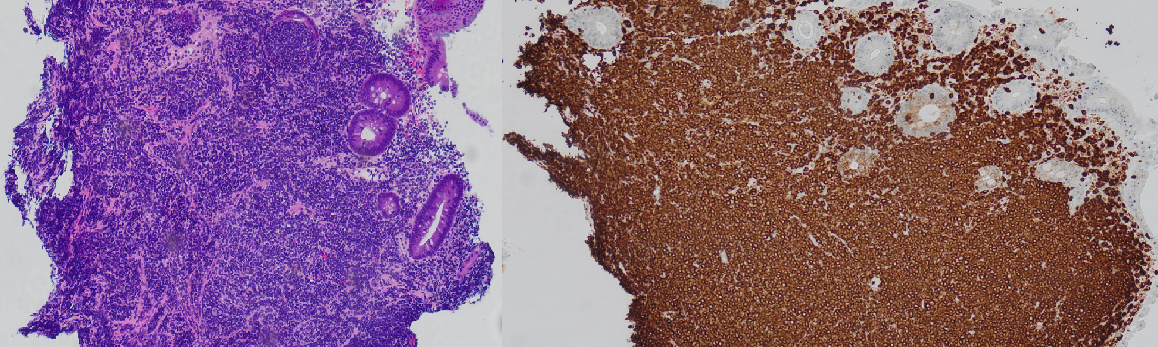
Figure: Hematoxylin and eosin stain [left] and BCL2 immunohistochemical stain [right] of cecum biopsies of the bulky submucosal lesion
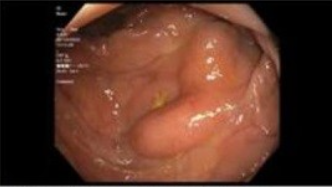
Figure: Bulky submucosal lesion in cecum on EGD
Disclosures:
Sarah Rahni indicated no relevant financial relationships.
Patrick Yang indicated no relevant financial relationships.
Naveena Sunkara indicated no relevant financial relationships.
Beth Schorr-Lesnick indicated no relevant financial relationships.
Sarah Rahni, DO, MBA, Patrick Yang, MD, Naveena Sunkara, MD, Beth Schorr-Lesnick, MD, FACG. P0381 - Gastrointestinal Mantle Cell Lymphoma: Diagnostic Value of Endoscopic and Histologic Correlation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Westchester Medical Center, Valhalla, NY
Introduction: Mantle cell lymphoma (MCL) is a rare, aggressive B-cell non-Hodgkin lymphoma that can involve the gastrointestinal (GI) tract. GI presentations are often asymptomatic or mimic other conditions, complicating diagnosis. We present a case highlighting the diagnostic challenges and endoscopic findings of GI MCL.
Case Description/
Methods: A 77-year-old male presented with over 6 weeks of postprandial diarrhea ( >10 loose stools/day), with nausea, early satiety, epigastric abdominal pain, intermittent hematochezia, and significant weight loss. He denied fevers, chills, or night sweats. Family history was notable for colon cancer in his brother, unsure of age at time of diagnosis. CT abdomen revealed thickened bowel wall from the terminal ileum to ascending colon, extensive lymphadenopathy, and hepatosplenomegaly. Colonoscopy revealed submucosal masses in the right colon and ileocecal valve as well as thickened folds/bulky submucosal lesions. Pathology revealed atypical lymphoid cell proliferation. Immunohistochemical study revealed the lymphoid cells were positive for CD20, CD79a, CD5, CD43, BCL-2 and Cyclin D1. Bone marrow biopsy was performed and confirmed a surface lambda light chain restricted B cell population expressing CD19, CD20, and CD22, and co-expressing CD5, which is consistent with CD5 positive mature B cell non-Hodgkin lymphoma.
Discussion: MCL is a rare subtype of B-cell non-Hodgkin lymphoma, accounting for about 6% of cases. GI involvement occurs in up to 30% of patients, often presenting with nonspecific symptoms like diarrhea, weight loss, or GI bleeding, which may delay diagnosis. One of the most common primary GI presentations of MCL is lymphomatous polyposis, which typically manifests in the ascending colon, ileum and ileocecal region. These polyps may be sessile, polypoid, or mixed, and have ulceration; rarely, numerous polyps are present throughout the entire GI tract. In this case, endoscopic biopsies confirmed MCL, emphasizing the importance of thorough histologic evaluation when lymphoid infiltrates are present. MCL commonly involves the ileocecal region, as seen here, and may mimic inflammatory or infectious conditions. Prompt recognition and tissue diagnosis are critical, as MCL is aggressive and requires timely systemic therapy. This case underscores the need for high suspicion and comprehensive evaluation in elderly patients with atypical GI symptoms.
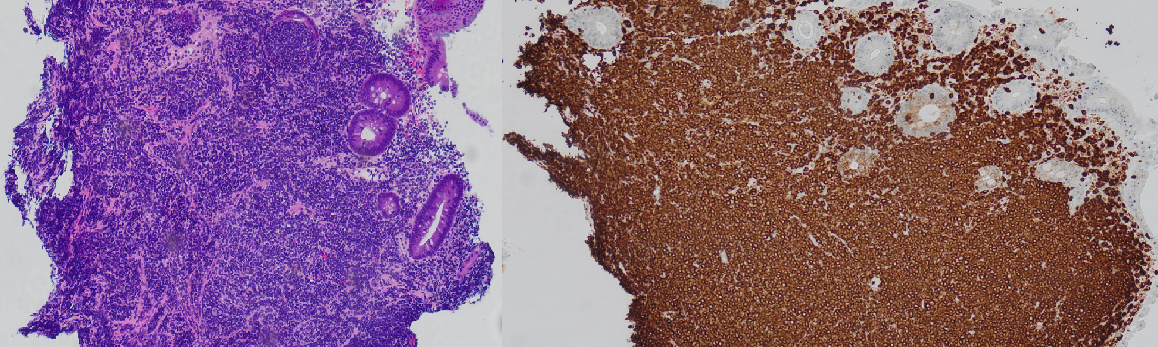
Figure: Hematoxylin and eosin stain [left] and BCL2 immunohistochemical stain [right] of cecum biopsies of the bulky submucosal lesion
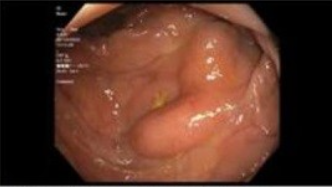
Figure: Bulky submucosal lesion in cecum on EGD
Disclosures:
Sarah Rahni indicated no relevant financial relationships.
Patrick Yang indicated no relevant financial relationships.
Naveena Sunkara indicated no relevant financial relationships.
Beth Schorr-Lesnick indicated no relevant financial relationships.
Sarah Rahni, DO, MBA, Patrick Yang, MD, Naveena Sunkara, MD, Beth Schorr-Lesnick, MD, FACG. P0381 - Gastrointestinal Mantle Cell Lymphoma: Diagnostic Value of Endoscopic and Histologic Correlation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
