Sunday Poster Session
Category: Colon
P0347 - Colonic Ischemia Without Mesenteric Occlusion: A Case Implicating Interferon-β

Alexander F. Siegel, MD
Creighton University Medical Center
Omaha, NE
Presenting Author(s)
Alexander Siegel, MD1, Kyaw Min Tun, DO2, Robert Kizer, MD2
1CHI Health Creighton University Medical Center, Elkhorn, NE; 2Creighton University Medical Center, Omaha, NE
Introduction:
Type I interferons, consisting primarily of interferon-alpha (IFN-α) and interferon-beta (IFN-β), are cytokines critical to the innate immune response against viral pathogens. Clinically, IFN-α is FDA-approved for chronic hepatitis, while IFN-β is approved for relapsing forms of multiple sclerosis (MS). Although uncommon, IFN-α has a well-documented association with the development of ischemic colitis. In contrast, the association between IFN-β and ischemic colitis is far less established.
Case Description/
Methods:
A 66-year-old female presented with an acute onset of right-sided abdominal pain and profuse watery diarrhea for two days. Medical history was notable for MS treated with chronic IFN-β therapy, methylenetetrahydrofolate reductase gene mutation with prior deep vein thrombosis (DVT), hypertension, and GERD. CT imaging demonstrated colonic wall thickening of the cecum and ascending colon, cecal pneumatosis, and a small focus of gas within the right hepatic lobe. The patient also had a significant leukocytosis of 38 K/uL with a normal lactate. The patient denied recent medication changes, risk factors for dehydration, or use of NSAIDs. She was admitted and broad-spectrum antibiotics were initiated. Infectious workup, including Clostridioides difficile toxin testing and gastrointestinal (GI) pathogen panel, was negative. Colonoscopy performed on hospital day two demonstrated confluent ulceration of the cecum and patchy ulcerations in the ascending colon, which were biopsied extensively. Histology was consistent with ischemic colitis. Given the patient's positive MTHFR gene mutation and history of DVT, CT angiogram was performed and confirmed patent mesenteric vasculature. After consultation with neurology IFN-β was discontinued. At two-week follow-up she reported resolution of symptoms. Repeat CT showed near resolution of prior inflammatory changes.
Discussion:
This case highlights a rare, but important link between IFN-β and GI ischemia. Though the precise mechanism remains unclear, it is thought that IFN-β induces endothelial cell dysfunction, leading to impaired mesenteric perfusion and pro-thrombotic events. Despite no vascular occlusion on imaging, clinical, endoscopic and histologic findings were consistent with ischemic colitis. Symptom resolution after IFN-β withdrawal further supports a drug induced pathology. Prior reports of IFN-β-induced ischemic colitis remain sparse, and this case contributes to the growing awareness of this potential adverse effect.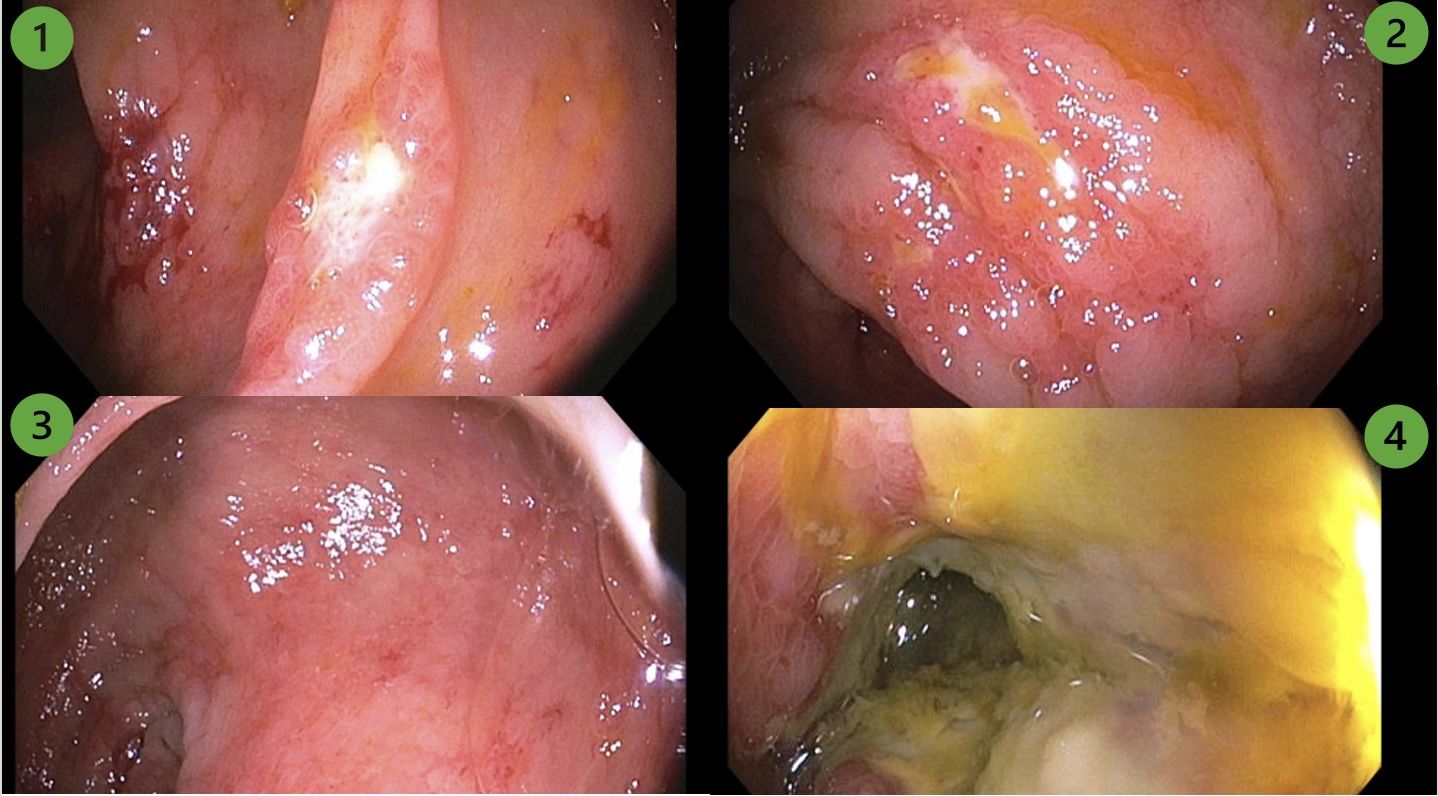
Figure: Colonoscopy images: (1–2) Patchy ulcerations and erythematous mucosa in the ascending colon; (3) similar findings at the hepatic flexure; and (4) severe, confluent ulcerations with pale mucosa in the cecum.
Figure: Abdominal CT images: (1) Initial presentation showing inflammatory changes in the cecum, and (2) two-week follow-up demonstrating near-complete resolution of prior cecal inflammation.
Disclosures:
Alexander Siegel indicated no relevant financial relationships.
Kyaw Min Tun indicated no relevant financial relationships.
Robert Kizer indicated no relevant financial relationships.
Alexander Siegel, MD1, Kyaw Min Tun, DO2, Robert Kizer, MD2. P0347 - Colonic Ischemia Without Mesenteric Occlusion: A Case Implicating Interferon-β, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

