Sunday Poster Session
Category: Colon
P0325 - Post-Polypectomy Syndrome Presenting With Sepsis-Like Symptoms: A Rare Complication Mimicking Diverticulitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Deepak Kumar, MBBS, MD (he/him/his)
Northwell Health
Port Jefferson, NY
Presenting Author(s)
Deepak Kumar, MBBS, MD1, Kelash Rai Ukrani, MD2, Sunny Kumar, MD3, Janta Devi Ukrani, MBBS, MD1, Ronika Devi Ukrani, MD4, Osama Abdur Rehman, MD5, Aasta Kumari, MD6, Fnu Aakash, MD5
1Northwell Health, Port Jefferson, NY; 2Jefferson Health, Media, PA; 3Wright Center for Graduate Medical Education, Scranton, PA; 4University of Texas Southwestern, Dallas, TX; 5Florida State University, Cape Coral, FL; 6North Central Bronx Hospital, New York, NY
Introduction: Post-polypectomy coagulation syndrome (PPCS) is an uncommon complication following colonoscopic polypectomy, resulting from thermal injury to the colonic wall without frank perforation. It may mimic diverticulitis or perforation, presenting with abdominal pain, leukocytosis, and low-grade fevers. Awareness is crucial to avoid unnecessary surgical interventions.
Case Description/
Methods: A 73-year-old female with a history of left renal cell carcinoma (s/p resection in 2022), GERD, and sigmoid diverticulosis presented to the ED one day after outpatient colonoscopy, due to Four sessile polyps were removed, including a 10 mm sessile polyp in the ascending colon resected using hot snare cautery. She developed progressive right lower quadrant abdominal pain, subjective fevers (Tmax 101°F), and chills. On presentation, she was hemodynamically stable with localized tenderness. Laboratory evaluation revealed leukocytosis and hemoglobin of 11.1 g/dL. CT abdomen/pelvis demonstrated new pericolic fat stranding around the ascending colon without free air or fluid collection, raising concern for post-polypectomy coagulation syndrome (PPCS) versus acute diverticulitis or microperforation. She was empirically started on IV fluids, piperacillin-tazobactam, and antipyretics. Blood cultures remained negative. The patient defervesced and improved clinically with supportive care alone. Serial abdominal exams remained benign, and no signs of peritonitis developed. She was discharged in stable condition with outpatient gastroenterology follow-up.
Discussion: PPCS is thought to result from transmural thermal injury during electrocautery, leading to localized peritonitis without overt perforation. Risk factors include larger polyp size, nonpedunculated morphology, and use of electrocautery in the right colon, where the wall is thinner. This case highlights the importance of differentiating PPCS from diverticulitis or perforation, as misdiagnosis can lead to unnecessary surgery or prolonged antibiotic use. Supportive care, serial exams, and close monitoring are often sufficient for recovery. With increasing colonoscopy screening, awareness of PPCS is vital among hospitalists and gastroenterologists.
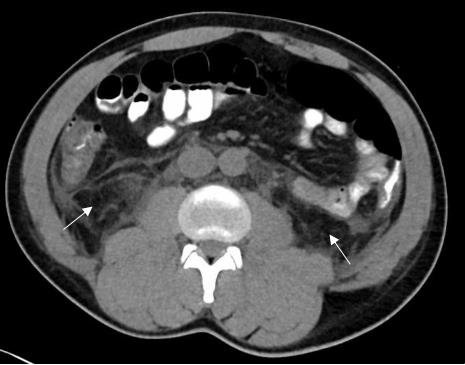
Figure: CT ABDOMEN/PELVIS: SHOWED NEW FAT STRANDING ALONG WITH THE ASCENDING COLON, WITHOUT EVIDENCE OF PERFORATION OR ABSCESS, RAISING CONCERN FOR IATROGENIC INJURY.
Disclosures:
Deepak Kumar indicated no relevant financial relationships.
Kelash Rai Ukrani indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Janta Devi Ukrani indicated no relevant financial relationships.
Ronika Devi Ukrani indicated no relevant financial relationships.
Osama Abdur Rehman indicated no relevant financial relationships.
Aasta Kumari indicated no relevant financial relationships.
Fnu Aakash indicated no relevant financial relationships.
Deepak Kumar, MBBS, MD1, Kelash Rai Ukrani, MD2, Sunny Kumar, MD3, Janta Devi Ukrani, MBBS, MD1, Ronika Devi Ukrani, MD4, Osama Abdur Rehman, MD5, Aasta Kumari, MD6, Fnu Aakash, MD5. P0325 - Post-Polypectomy Syndrome Presenting With Sepsis-Like Symptoms: A Rare Complication Mimicking Diverticulitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Northwell Health, Port Jefferson, NY; 2Jefferson Health, Media, PA; 3Wright Center for Graduate Medical Education, Scranton, PA; 4University of Texas Southwestern, Dallas, TX; 5Florida State University, Cape Coral, FL; 6North Central Bronx Hospital, New York, NY
Introduction: Post-polypectomy coagulation syndrome (PPCS) is an uncommon complication following colonoscopic polypectomy, resulting from thermal injury to the colonic wall without frank perforation. It may mimic diverticulitis or perforation, presenting with abdominal pain, leukocytosis, and low-grade fevers. Awareness is crucial to avoid unnecessary surgical interventions.
Case Description/
Methods: A 73-year-old female with a history of left renal cell carcinoma (s/p resection in 2022), GERD, and sigmoid diverticulosis presented to the ED one day after outpatient colonoscopy, due to Four sessile polyps were removed, including a 10 mm sessile polyp in the ascending colon resected using hot snare cautery. She developed progressive right lower quadrant abdominal pain, subjective fevers (Tmax 101°F), and chills. On presentation, she was hemodynamically stable with localized tenderness. Laboratory evaluation revealed leukocytosis and hemoglobin of 11.1 g/dL. CT abdomen/pelvis demonstrated new pericolic fat stranding around the ascending colon without free air or fluid collection, raising concern for post-polypectomy coagulation syndrome (PPCS) versus acute diverticulitis or microperforation. She was empirically started on IV fluids, piperacillin-tazobactam, and antipyretics. Blood cultures remained negative. The patient defervesced and improved clinically with supportive care alone. Serial abdominal exams remained benign, and no signs of peritonitis developed. She was discharged in stable condition with outpatient gastroenterology follow-up.
Discussion: PPCS is thought to result from transmural thermal injury during electrocautery, leading to localized peritonitis without overt perforation. Risk factors include larger polyp size, nonpedunculated morphology, and use of electrocautery in the right colon, where the wall is thinner. This case highlights the importance of differentiating PPCS from diverticulitis or perforation, as misdiagnosis can lead to unnecessary surgery or prolonged antibiotic use. Supportive care, serial exams, and close monitoring are often sufficient for recovery. With increasing colonoscopy screening, awareness of PPCS is vital among hospitalists and gastroenterologists.
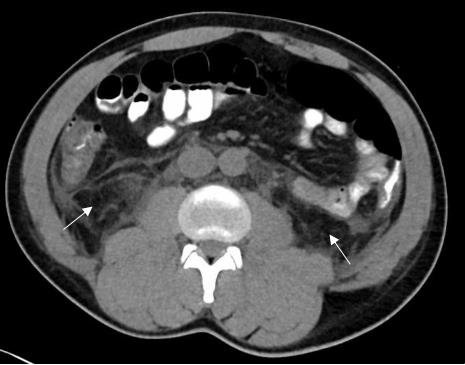
Figure: CT ABDOMEN/PELVIS: SHOWED NEW FAT STRANDING ALONG WITH THE ASCENDING COLON, WITHOUT EVIDENCE OF PERFORATION OR ABSCESS, RAISING CONCERN FOR IATROGENIC INJURY.
Disclosures:
Deepak Kumar indicated no relevant financial relationships.
Kelash Rai Ukrani indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Janta Devi Ukrani indicated no relevant financial relationships.
Ronika Devi Ukrani indicated no relevant financial relationships.
Osama Abdur Rehman indicated no relevant financial relationships.
Aasta Kumari indicated no relevant financial relationships.
Fnu Aakash indicated no relevant financial relationships.
Deepak Kumar, MBBS, MD1, Kelash Rai Ukrani, MD2, Sunny Kumar, MD3, Janta Devi Ukrani, MBBS, MD1, Ronika Devi Ukrani, MD4, Osama Abdur Rehman, MD5, Aasta Kumari, MD6, Fnu Aakash, MD5. P0325 - Post-Polypectomy Syndrome Presenting With Sepsis-Like Symptoms: A Rare Complication Mimicking Diverticulitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
