Sunday Poster Session
Category: Colon
P0262 - Joint Imaging Frequently Reveals Abnormalities in Inflammatory Bowel Disease-Associated Peripheral Spondyloarthropathy
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rashid Abdel-Razeq, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Rashid Abdel-Razeq, MD1, Lana Dardari, MD2, Michael Forney, MD3, Taha Qazi, MD1, Florian Rieder, MD1, Katherine Falloon, MD1
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Foundation, Westlake, OH; 3Cleveland Clinic, Cleveland, OH
Introduction: Inflammatory bowel disease (IBD) is a chronic inflammatory condition of the luminal gastrointestinal tract that can be associated with several extra-intestinal manifestations (EIMs). Though IBD-associated peripheral spondyloarthropathy (IBD-pSpA) is among the most prevalent of these EIMs, a clear diagnostic pathway for this condition is lacking. Notably, findings on joint imaging in patients with IBD-pSpA specifically have not been well characterized. This study aims to bridge this knowledge gap by evaluating imaging findings in patients with IBD-pSpA and assessing for any link between imaging findings and luminal inflammation.
Methods: We conducted a retrospective cohort study of patients with IBD-pSpA who underwent joint imaging. Inclusion criteria included a confirmed diagnosis of IBD, rheumatologist-confirmed diagnosis of IBD-pSpA and use of at least one joint imaging modality (ultrasound, X-ray, or magnetic resonance imaging (MRI)). Patients with any diagnosis of a non-IBD-related arthritis were excluded. Active luminal IBD was defined by endoscopic and laboratory findings.
Results: We screened 8,500 patients with IBD, of whom 80 met the inclusion criteria and were included in the final analysis. The cohort was 61.3% female and 33.8% male, with 82.5% identifying as white and 8.8% as black or African American. Crohn’s disease accounted for 61.3% of cases and ulcerative colitis for 39%. Mean age at pSpA diagnosis was 44.1 ± 15.4 years. On examination by rheumatology, 81.2% of patients had at least one abnormal joint finding, mostly tenderness (N=44, 55.0%) and swelling (N=22, 27.5%). Imaging-confirmed joint involvement was observed in 85.0% of the cohort. The most frequent imaging findings included joint space narrowing (N=28, 35.0%), effusion (N=10, 12.5%), bone marrow edema (N=10, 12.5%) and soft tissue swelling (N=8, 10.0%). 43.8% of patients had active luminal IBD. Although joint imaging findings were more common among patients with active IBD, the association did not reach statistical significance (OR 2.67, 95% CI 0.66–10.71; p = 0.212). After the diagnosis of pSpA, 70% of patients required treatment escalation.
Discussion: Joint abnormalities, especially joint space narrowing, were identified on imaging in most patients with IBD-pSpA, highlighting joint imaging as a key diagnostic tool. Prospective studies are needed to identify the optimal imaging modality for the diagnosis and to better understand the relationship between abnormal findings and luminal disease activity.
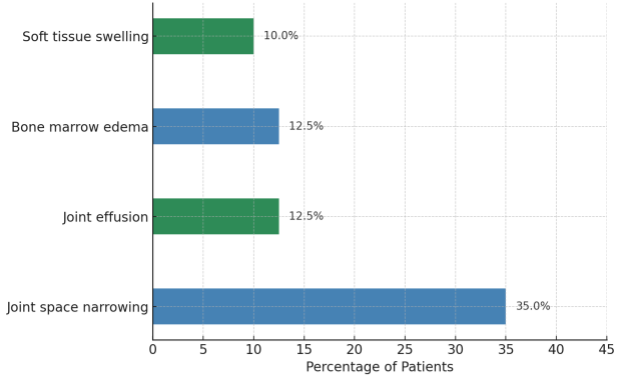
Figure: Figure 1: Bar graph illustrating joint imaging findings in patient with IBD-associated peripheral spondylopathy
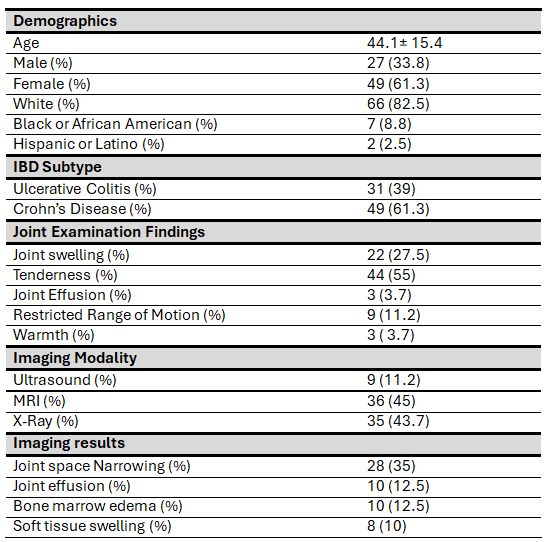
Figure: Table 1: Distribution of patient population
Disclosures:
Rashid Abdel-Razeq indicated no relevant financial relationships.
Lana Dardari indicated no relevant financial relationships.
Michael Forney indicated no relevant financial relationships.
Taha Qazi: Abbvie – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Celltirion – Grant/Research Support. Eli Lilly – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant. Johnson and Johnson – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant, Speakers Bureau. pfizer – Grant/Research Support.
Florian Rieder: Adiso – Advisory Committee/Board Member, Consultant. Adnovate, Agomab, Allergan, AbbVie, Arena, Astra Zeneca, Bausch & Lomb, Boehringer-Ingelheim, Celgene/BMS, Celltrion, CDISC, Celsius, Cowen, 89Bio – Advisory Committee/Board Member, Consultant. Eugit, Ferring, Galapagos, Galmed, Genentech, Gilead, Gossamer, Granite, Guidepoint, Helmsley, Horizon Therapeutics, Image Analysis Limited – Advisory Committee/Board Member, Consultant. Landos, Jannsen, Koutif, Mestag, Metacrine, Mirum, Mobius, Mopac, Morphic, Myka Labs, Organovo, Origo, Palisade, Pfizer, Pliant, Prometheus Bioscience – Advisory Committee/Board Member, Consultant. Receptos, RedX, Roche, Samsung, Sanofi, Surmodics, Surrozen, Takeda, Techlab, Teva, Theravance, Thetis, Tr1x Bio, UCB, Ysios – Advisory Committee/Board Member, Consultant.
Katherine Falloon: Cardinal Health, Inc. – Husband is employee. Janssen Pharmaceuticals, Inc. – Consultant. MD Education – Speaker. Pfizer – Grant/Research Support. Takeda Pharmaceuticals, Inc. – Speaker.
Rashid Abdel-Razeq, MD1, Lana Dardari, MD2, Michael Forney, MD3, Taha Qazi, MD1, Florian Rieder, MD1, Katherine Falloon, MD1. P0262 - Joint Imaging Frequently Reveals Abnormalities in Inflammatory Bowel Disease-Associated Peripheral Spondyloarthropathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Foundation, Westlake, OH; 3Cleveland Clinic, Cleveland, OH
Introduction: Inflammatory bowel disease (IBD) is a chronic inflammatory condition of the luminal gastrointestinal tract that can be associated with several extra-intestinal manifestations (EIMs). Though IBD-associated peripheral spondyloarthropathy (IBD-pSpA) is among the most prevalent of these EIMs, a clear diagnostic pathway for this condition is lacking. Notably, findings on joint imaging in patients with IBD-pSpA specifically have not been well characterized. This study aims to bridge this knowledge gap by evaluating imaging findings in patients with IBD-pSpA and assessing for any link between imaging findings and luminal inflammation.
Methods: We conducted a retrospective cohort study of patients with IBD-pSpA who underwent joint imaging. Inclusion criteria included a confirmed diagnosis of IBD, rheumatologist-confirmed diagnosis of IBD-pSpA and use of at least one joint imaging modality (ultrasound, X-ray, or magnetic resonance imaging (MRI)). Patients with any diagnosis of a non-IBD-related arthritis were excluded. Active luminal IBD was defined by endoscopic and laboratory findings.
Results: We screened 8,500 patients with IBD, of whom 80 met the inclusion criteria and were included in the final analysis. The cohort was 61.3% female and 33.8% male, with 82.5% identifying as white and 8.8% as black or African American. Crohn’s disease accounted for 61.3% of cases and ulcerative colitis for 39%. Mean age at pSpA diagnosis was 44.1 ± 15.4 years. On examination by rheumatology, 81.2% of patients had at least one abnormal joint finding, mostly tenderness (N=44, 55.0%) and swelling (N=22, 27.5%). Imaging-confirmed joint involvement was observed in 85.0% of the cohort. The most frequent imaging findings included joint space narrowing (N=28, 35.0%), effusion (N=10, 12.5%), bone marrow edema (N=10, 12.5%) and soft tissue swelling (N=8, 10.0%). 43.8% of patients had active luminal IBD. Although joint imaging findings were more common among patients with active IBD, the association did not reach statistical significance (OR 2.67, 95% CI 0.66–10.71; p = 0.212). After the diagnosis of pSpA, 70% of patients required treatment escalation.
Discussion: Joint abnormalities, especially joint space narrowing, were identified on imaging in most patients with IBD-pSpA, highlighting joint imaging as a key diagnostic tool. Prospective studies are needed to identify the optimal imaging modality for the diagnosis and to better understand the relationship between abnormal findings and luminal disease activity.
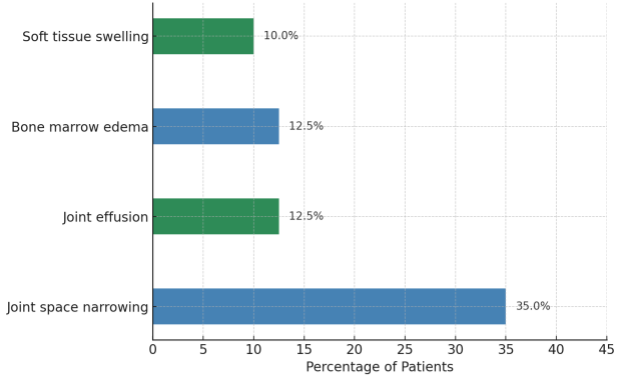
Figure: Figure 1: Bar graph illustrating joint imaging findings in patient with IBD-associated peripheral spondylopathy
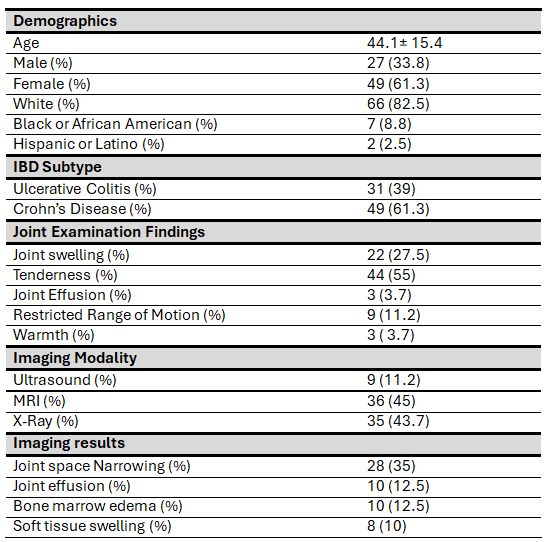
Figure: Table 1: Distribution of patient population
Disclosures:
Rashid Abdel-Razeq indicated no relevant financial relationships.
Lana Dardari indicated no relevant financial relationships.
Michael Forney indicated no relevant financial relationships.
Taha Qazi: Abbvie – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Celltirion – Grant/Research Support. Eli Lilly – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant. Johnson and Johnson – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant, Speakers Bureau. pfizer – Grant/Research Support.
Florian Rieder: Adiso – Advisory Committee/Board Member, Consultant. Adnovate, Agomab, Allergan, AbbVie, Arena, Astra Zeneca, Bausch & Lomb, Boehringer-Ingelheim, Celgene/BMS, Celltrion, CDISC, Celsius, Cowen, 89Bio – Advisory Committee/Board Member, Consultant. Eugit, Ferring, Galapagos, Galmed, Genentech, Gilead, Gossamer, Granite, Guidepoint, Helmsley, Horizon Therapeutics, Image Analysis Limited – Advisory Committee/Board Member, Consultant. Landos, Jannsen, Koutif, Mestag, Metacrine, Mirum, Mobius, Mopac, Morphic, Myka Labs, Organovo, Origo, Palisade, Pfizer, Pliant, Prometheus Bioscience – Advisory Committee/Board Member, Consultant. Receptos, RedX, Roche, Samsung, Sanofi, Surmodics, Surrozen, Takeda, Techlab, Teva, Theravance, Thetis, Tr1x Bio, UCB, Ysios – Advisory Committee/Board Member, Consultant.
Katherine Falloon: Cardinal Health, Inc. – Husband is employee. Janssen Pharmaceuticals, Inc. – Consultant. MD Education – Speaker. Pfizer – Grant/Research Support. Takeda Pharmaceuticals, Inc. – Speaker.
Rashid Abdel-Razeq, MD1, Lana Dardari, MD2, Michael Forney, MD3, Taha Qazi, MD1, Florian Rieder, MD1, Katherine Falloon, MD1. P0262 - Joint Imaging Frequently Reveals Abnormalities in Inflammatory Bowel Disease-Associated Peripheral Spondyloarthropathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
