Sunday Poster Session
Category: Biliary/Pancreas
P0248 - Drain Delays Diagnosis in Disconnected Pancreatic Duct Syndrome
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Narinderjeet Kaur, MD, MS (she/her/hers)
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
Narinderjeet Kaur, MD, MS1, Benjamin Silver, MD1, Anwar Uddin, MD1, Taha Shakarchi, MD2, Ishan Antony, MD2, Ritik M. Goyal, MBBS3, Rebhi Rabah, MD1, Selome Yewedalsew, MD1, Yitzhak Twersky, MD4
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2Beth Israel Lahey Health, Burlington, MA; 3Rutgers New Jersey Medical School, Newark, NJ; 4St John’s Episcopal Hospital, Far Rockaway, NY
Introduction: Disconnected pancreatic duct syndrome (DPDS) is a rare, often underdiagnosed condition involving complete disruption of the main pancreatic duct between viable pancreatic tissue and the duodenum. It can result from acute necrotizing or chronic pancreatitis, pancreatic surgery, trauma, or malignancy, and may present as recurrent fluid collections or pancreatico-cutaneous fistulas. We report a case of a 42-year-old man whose DPDS diagnosis was delayed due to the presence of a percutaneous peripancreatic drain.
Case Description/
Methods: A 42-year-old man with a history of alcohol abuse and acute necrotizing pancreatitis presented with two days of abdominal pain after drinking two beers, along with nausea, post-prandial steatorrhea, and cessation of pancreatic drain output. A year prior, he had necrotizing pancreatitis complicated by fluid collection, managed with a percutaneous drain after failed endoscopic transmural drainage, prompting multiple readmissions. On this admission, vitals were normal. Physical exam showed epigastric tenderness, and a midline drain with scant serosanguinous fluid. Labs revealed lipase of 3,000 U/L. Computed Tomography (CT) of the abdomen showed a dilated pancreatic duct in the body and tail (Figure 1), with abrupt ductal disconnection in the proximal body/neck (Figure 2), just posterior to the drain (Figure 3). Magnetic resonance cholangiopancreatography confirmed a 7 mm ductal dilatation with a transition at the body and an anterior exophytic cystic lesion communicating with the duct. The patient was treated with IV fluids, multimodal pain control, and transferred to a tertiary center for further management of DPDS.
Discussion: DPDS is a rare complication of a common disease in which the diagnosis is often missed. It is our opinion that the patient’s hospitalizations for recurrent pancreatitis were manifestations of DPDS. The diagnosis was delayed in part due to the drain preventing the accumulation of fluid, and a leak/DPDS was not considered. Treatment of DPDS can range from conservative monitoring, ERCP with transpapillary stenting with or without transgastric drainage of disconnected distal duct, Roux-en-Y pancreatectomy, or distal pancreatectomy. Untreated DPDS can lead to fistula formation and organ failure from enzymatic autodigestion. Due to its variable presentation and the need for advanced imaging, DPDS can be difficult to diagnose, often leading to delayed treatment, as in our patient, who was transferred out to a tertiary hospital for further management.
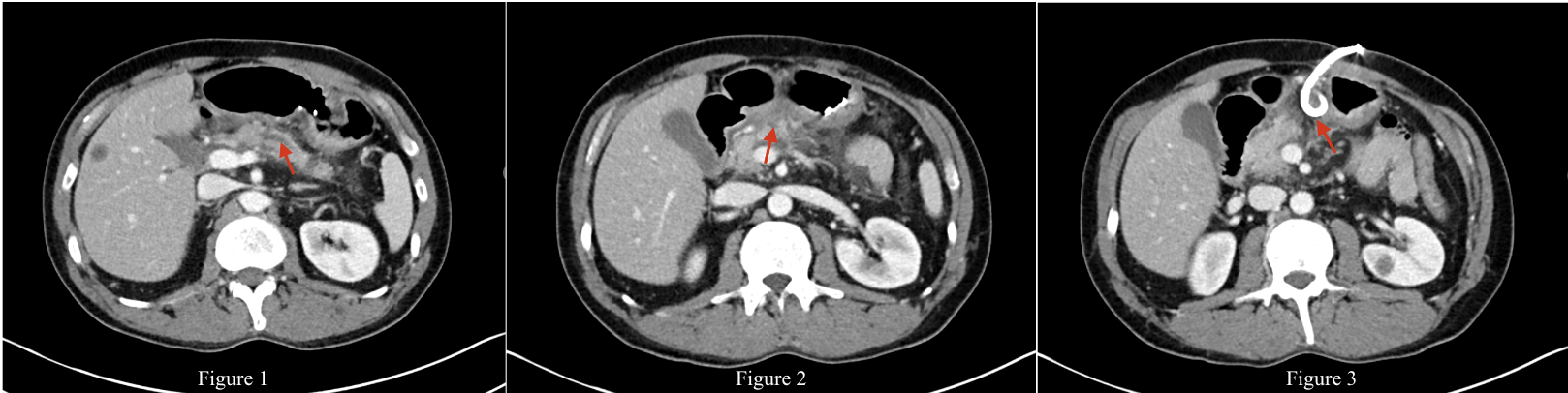
Figure: CT Abdomen Figure 1: Dilated pancreatic duct in the body and tail. Figure 2: Abrupt ductal disconnection in the proximal body/neck. Figure 3: Percutaneous drain in the pancreas.
Disclosures:
Narinderjeet Kaur indicated no relevant financial relationships.
Benjamin Silver indicated no relevant financial relationships.
Anwar Uddin indicated no relevant financial relationships.
Taha Shakarchi indicated no relevant financial relationships.
Ishan Antony indicated no relevant financial relationships.
Ritik M. Goyal indicated no relevant financial relationships.
Rebhi Rabah indicated no relevant financial relationships.
Selome Yewedalsew indicated no relevant financial relationships.
Yitzhak Twersky indicated no relevant financial relationships.
Narinderjeet Kaur, MD, MS1, Benjamin Silver, MD1, Anwar Uddin, MD1, Taha Shakarchi, MD2, Ishan Antony, MD2, Ritik M. Goyal, MBBS3, Rebhi Rabah, MD1, Selome Yewedalsew, MD1, Yitzhak Twersky, MD4. P0248 - Drain Delays Diagnosis in Disconnected Pancreatic Duct Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2Beth Israel Lahey Health, Burlington, MA; 3Rutgers New Jersey Medical School, Newark, NJ; 4St John’s Episcopal Hospital, Far Rockaway, NY
Introduction: Disconnected pancreatic duct syndrome (DPDS) is a rare, often underdiagnosed condition involving complete disruption of the main pancreatic duct between viable pancreatic tissue and the duodenum. It can result from acute necrotizing or chronic pancreatitis, pancreatic surgery, trauma, or malignancy, and may present as recurrent fluid collections or pancreatico-cutaneous fistulas. We report a case of a 42-year-old man whose DPDS diagnosis was delayed due to the presence of a percutaneous peripancreatic drain.
Case Description/
Methods: A 42-year-old man with a history of alcohol abuse and acute necrotizing pancreatitis presented with two days of abdominal pain after drinking two beers, along with nausea, post-prandial steatorrhea, and cessation of pancreatic drain output. A year prior, he had necrotizing pancreatitis complicated by fluid collection, managed with a percutaneous drain after failed endoscopic transmural drainage, prompting multiple readmissions. On this admission, vitals were normal. Physical exam showed epigastric tenderness, and a midline drain with scant serosanguinous fluid. Labs revealed lipase of 3,000 U/L. Computed Tomography (CT) of the abdomen showed a dilated pancreatic duct in the body and tail (Figure 1), with abrupt ductal disconnection in the proximal body/neck (Figure 2), just posterior to the drain (Figure 3). Magnetic resonance cholangiopancreatography confirmed a 7 mm ductal dilatation with a transition at the body and an anterior exophytic cystic lesion communicating with the duct. The patient was treated with IV fluids, multimodal pain control, and transferred to a tertiary center for further management of DPDS.
Discussion: DPDS is a rare complication of a common disease in which the diagnosis is often missed. It is our opinion that the patient’s hospitalizations for recurrent pancreatitis were manifestations of DPDS. The diagnosis was delayed in part due to the drain preventing the accumulation of fluid, and a leak/DPDS was not considered. Treatment of DPDS can range from conservative monitoring, ERCP with transpapillary stenting with or without transgastric drainage of disconnected distal duct, Roux-en-Y pancreatectomy, or distal pancreatectomy. Untreated DPDS can lead to fistula formation and organ failure from enzymatic autodigestion. Due to its variable presentation and the need for advanced imaging, DPDS can be difficult to diagnose, often leading to delayed treatment, as in our patient, who was transferred out to a tertiary hospital for further management.
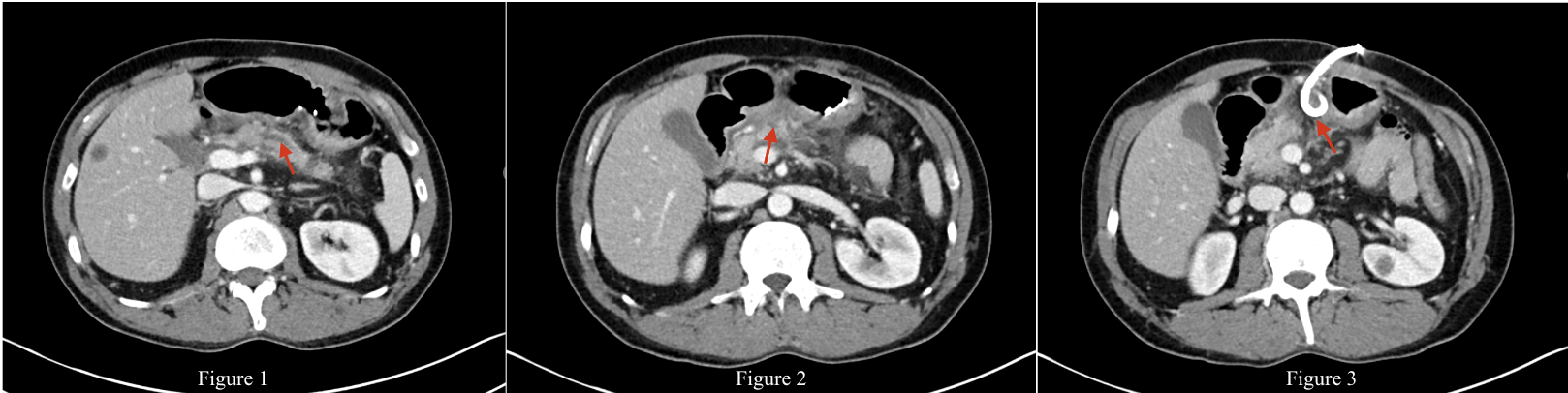
Figure: CT Abdomen Figure 1: Dilated pancreatic duct in the body and tail. Figure 2: Abrupt ductal disconnection in the proximal body/neck. Figure 3: Percutaneous drain in the pancreas.
Disclosures:
Narinderjeet Kaur indicated no relevant financial relationships.
Benjamin Silver indicated no relevant financial relationships.
Anwar Uddin indicated no relevant financial relationships.
Taha Shakarchi indicated no relevant financial relationships.
Ishan Antony indicated no relevant financial relationships.
Ritik M. Goyal indicated no relevant financial relationships.
Rebhi Rabah indicated no relevant financial relationships.
Selome Yewedalsew indicated no relevant financial relationships.
Yitzhak Twersky indicated no relevant financial relationships.
Narinderjeet Kaur, MD, MS1, Benjamin Silver, MD1, Anwar Uddin, MD1, Taha Shakarchi, MD2, Ishan Antony, MD2, Ritik M. Goyal, MBBS3, Rebhi Rabah, MD1, Selome Yewedalsew, MD1, Yitzhak Twersky, MD4. P0248 - Drain Delays Diagnosis in Disconnected Pancreatic Duct Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
