Sunday Poster Session
Category: Biliary/Pancreas
P0244 - Acute Pancreatitis After Percutaneous Mechanical Thrombectomy of a Thrombosed Arteriovenous Fistula
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- IT
Ian Tobal, DO
Ochsner Medical Center
New Orleans, LA
Presenting Author(s)
Ian Tobal, DO, Andrew J. Guthrie, MD
Ochsner Medical Center, New Orleans, LA
Introduction: In the US, there are roughly 250,000 cases of acute pancreatitis diagnosed annually, with that number currently on the rise. Acute pancreatitis is the leading gastrointestinal cause of hospitalization. The most common etiologies include gallstones and alcohol use. However, other recognized causes include medications, elevated triglyceride levels, trauma, and autoimmune disorders. This condition is characterized by abdominal pain, elevated lipase levels, and findings of pancreatic inflammation on imaging. Treatment may vary by etiology but routinely consists of IV hydration and bowel rest. While most cases are readily explained, there remains a portion of patients with inconspicuous etiologies. This case highlights and discusses an unusual cause of acute pancreatitis in an elderly female.
Case Description/
Methods: A 69-year-old female with a past medical history of ESRD on HD and CHF presented with abdominal pain, nausea, vomiting, and diarrhea after undergoing a fistulogram with percutaneous mechanical thrombectomy (PMT) of a stenosed AVF earlier that same day. On arrival, physical exam showed an ill appearing women with significant epigastric abdominal pain and distention. She denied recent alcohol use or history of cholelithiasis. Initial lab workup was notable for a leukocytosis of 13.84 and a lipase of 1,453. CT A/P was obtained and showed diffuse peripancreatic fat stranding, consistent with interstitial pancreatitis; no gallstones or pancreatic fluid collections were seen. Her symptoms improved with bowel rest, pain management, and IVF. She was discharged 3 days later.
Discussion: Acute pancreatitis following PMT is an extremely rare cause of a common presentation. Most literature on this topic is limited to small case series. During PMT, intravascular hemolysis occurs and leads to the development and accumulation of free hemoglobin. Free hemoglobin can activate an inflammatory response, upregulate acute phase reactants, promote free oxygen radical formation, and damage the microvasculature of the pancreas. Risk factors to contribute to development of pancreatitis after PMT include large thrombus size and central vasculature involvement. Typically, symptoms present within 24 hours of PMT. Management of post-PTM pancreatitis includes the routine practices of IVF, pain control, and bowel rest. Promptly recognizing post-PMT pancreatitis can spare these patients extensive work ups and does not include more than a physical exam, a serum lipase, and pancreatic imaging.
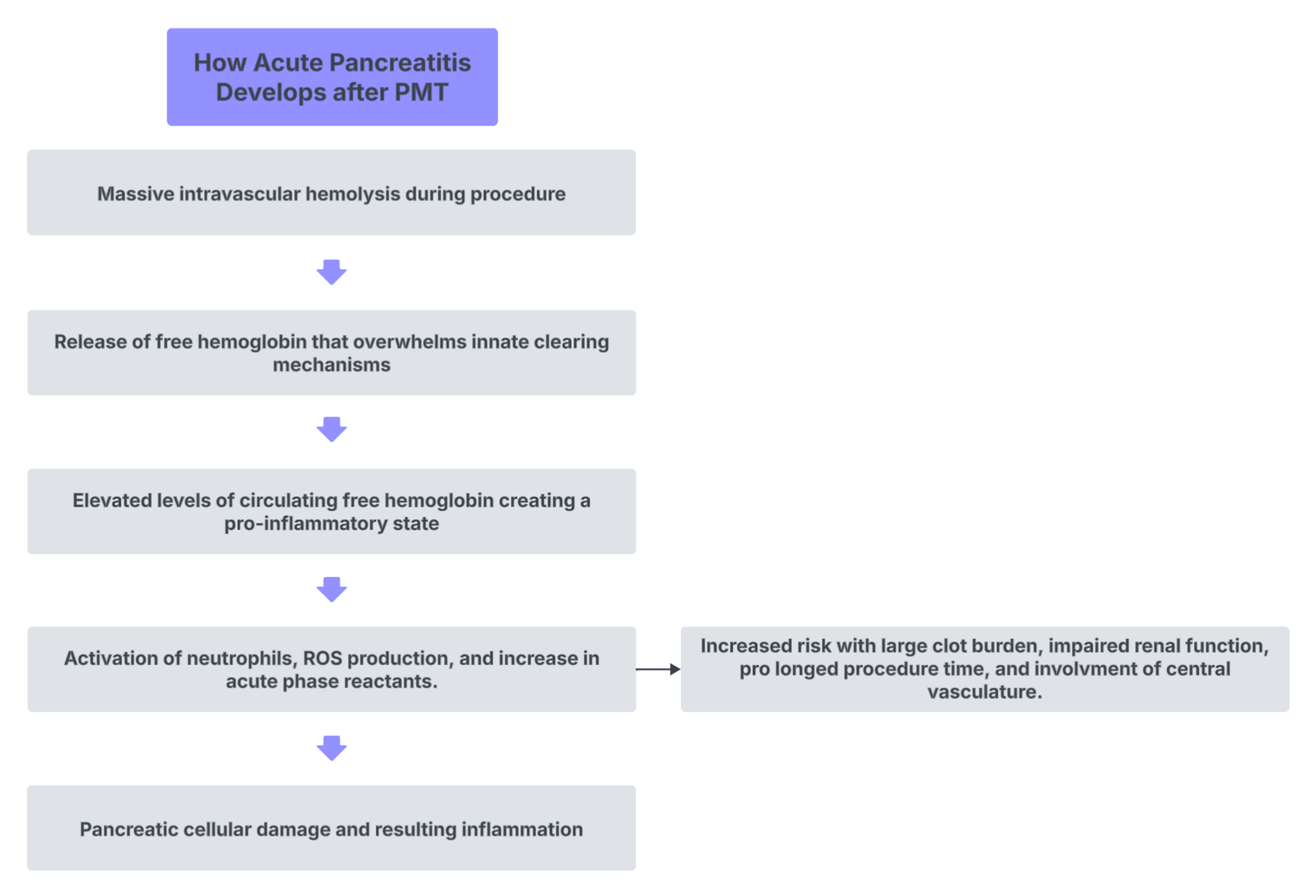
Figure: Flowchart describing development of acute pancreatitis after PMT.
Disclosures:
Ian Tobal indicated no relevant financial relationships.
Andrew Guthrie indicated no relevant financial relationships.
Ian Tobal, DO, Andrew J. Guthrie, MD. P0244 - Acute Pancreatitis After Percutaneous Mechanical Thrombectomy of a Thrombosed Arteriovenous Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Ochsner Medical Center, New Orleans, LA
Introduction: In the US, there are roughly 250,000 cases of acute pancreatitis diagnosed annually, with that number currently on the rise. Acute pancreatitis is the leading gastrointestinal cause of hospitalization. The most common etiologies include gallstones and alcohol use. However, other recognized causes include medications, elevated triglyceride levels, trauma, and autoimmune disorders. This condition is characterized by abdominal pain, elevated lipase levels, and findings of pancreatic inflammation on imaging. Treatment may vary by etiology but routinely consists of IV hydration and bowel rest. While most cases are readily explained, there remains a portion of patients with inconspicuous etiologies. This case highlights and discusses an unusual cause of acute pancreatitis in an elderly female.
Case Description/
Methods: A 69-year-old female with a past medical history of ESRD on HD and CHF presented with abdominal pain, nausea, vomiting, and diarrhea after undergoing a fistulogram with percutaneous mechanical thrombectomy (PMT) of a stenosed AVF earlier that same day. On arrival, physical exam showed an ill appearing women with significant epigastric abdominal pain and distention. She denied recent alcohol use or history of cholelithiasis. Initial lab workup was notable for a leukocytosis of 13.84 and a lipase of 1,453. CT A/P was obtained and showed diffuse peripancreatic fat stranding, consistent with interstitial pancreatitis; no gallstones or pancreatic fluid collections were seen. Her symptoms improved with bowel rest, pain management, and IVF. She was discharged 3 days later.
Discussion: Acute pancreatitis following PMT is an extremely rare cause of a common presentation. Most literature on this topic is limited to small case series. During PMT, intravascular hemolysis occurs and leads to the development and accumulation of free hemoglobin. Free hemoglobin can activate an inflammatory response, upregulate acute phase reactants, promote free oxygen radical formation, and damage the microvasculature of the pancreas. Risk factors to contribute to development of pancreatitis after PMT include large thrombus size and central vasculature involvement. Typically, symptoms present within 24 hours of PMT. Management of post-PTM pancreatitis includes the routine practices of IVF, pain control, and bowel rest. Promptly recognizing post-PMT pancreatitis can spare these patients extensive work ups and does not include more than a physical exam, a serum lipase, and pancreatic imaging.
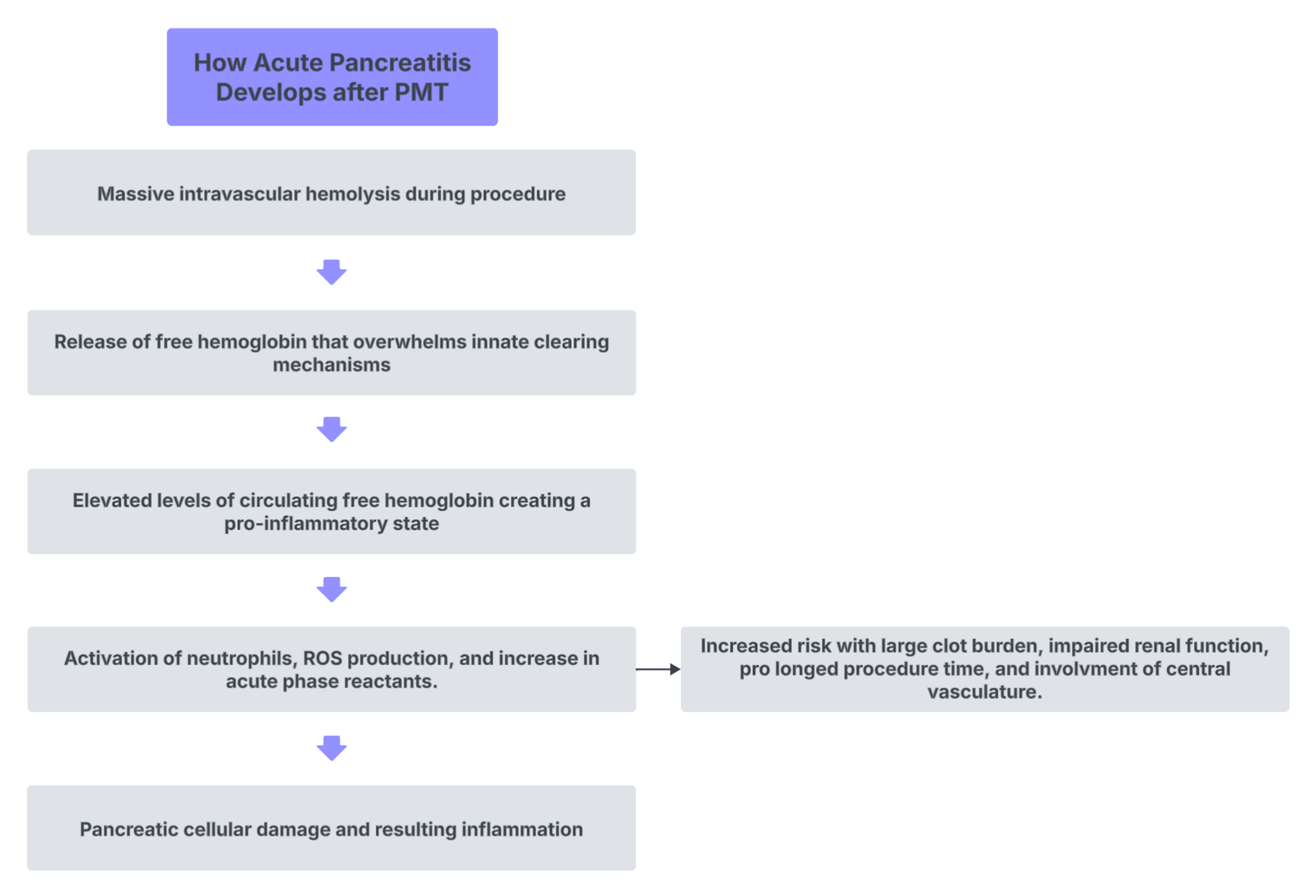
Figure: Flowchart describing development of acute pancreatitis after PMT.
Disclosures:
Ian Tobal indicated no relevant financial relationships.
Andrew Guthrie indicated no relevant financial relationships.
Ian Tobal, DO, Andrew J. Guthrie, MD. P0244 - Acute Pancreatitis After Percutaneous Mechanical Thrombectomy of a Thrombosed Arteriovenous Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

