Sunday Poster Session
Category: Biliary/Pancreas
P0239 - Evolution From a Large Intraductal Papillary Mucinous Neoplasm to Pseudocyst After Endoscopic Ultrasound-Guided Chemoablation
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- QA
Qusai Almasad, MD
Roger Williams Medical Center
Providence, RI
Presenting Author(s)
Qusai AlMasad, MD1, Zaid Ansari, MD2, Akram Ahmad, MD2, Tilak Shah, MD2
1Roger Williams Medical Center, Providence, RI; 2Cleveland Clinic Florida, Weston, FL
Introduction: Endoscopic ultrasound (EUS) guided chemoablation has emerged as an option for treatment of intermediate-risk side branch intraductal papillary mucinous neoplasms (IPMNs), i.e. – IPMNs 2 – 5 cm in cross section and without mural nodules or main pancreatic duct dilation. In the CHARM and CHARM2 trials, chemoablation with paclitaxel and gemcitabine was associated with a durable response in about two-thirds of patients. The optimal workup and management of non-responders and those with interval growth who are not optimal surgical candidates is not well studied. We describe a patient with apparent interval growth after chemoablation, in whom cyst fluid analysis demonstrated replacement of mucinous cyst fluid with fluid more consistent with a benign pancreatic juice.
Case Description/
Methods: During routine surveillance, a 82-year-old woman was noted to have progressive increase in size of a cystic lesion in the pancreatic body from 1.5 cm to 4 cm over several years. EUS-guided cyst aspiration showed amylase 334 and CEA 155,785 consistent with a side branch IPMN. After discussion at the multidisciplinary pancreas tumor board, the patient underwent EUS guided chemoablation. Three months later, the cyst had decreased in size to 32 mm, so EUS guided chemoablation was repeated (cyst fluid CEA 432, glucose < 2, amylase 334). Two years later, MRI reported that cyst size was 4 cm. Layering internal debris was also noted. Repeat EUS-guided cyst fluid analysis showed amylase 32,421, glucose 77, and CEA 54. Based on layering debris and cyst fluid analysis, benign pancreatic juice was believed to be more likely than interval IPMN growth.
Discussion: We hypothesize that the patient had a complete or near complete response to chemoablation, but the large cyst cavity filled with pancreatic juice given its direct communication with a pancreatic duct sidebranch. EUS-guided chemoablation has only recently been incorporated in select tertiary centers. Our case highlights an important teaching point that has not been previously described. In “non-responders” or those with interval growth of a larger cyst, careful assessment of imaging features and repeat cyst fluid analysis can distinguish a “non-responder” from refill of the cavity with benign pancreatic juice.
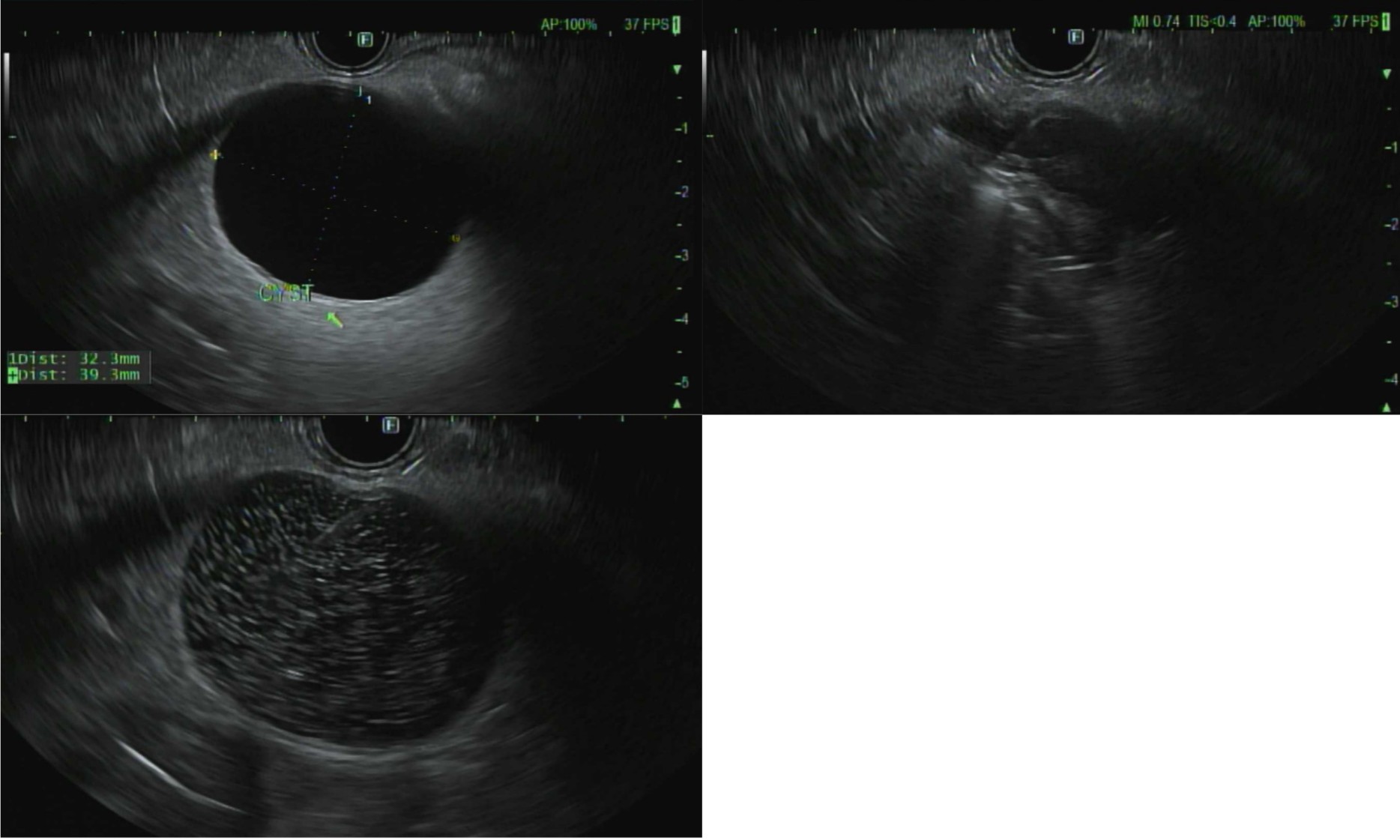
Figure: FIGURE 1A: Unilocular 4 cm cyst in pancreas body ;
1B near complete aspiration followed by 1C injection of an equal volume of paclitaxel and gemcitabine with
characteristic “snow-globe” appearance
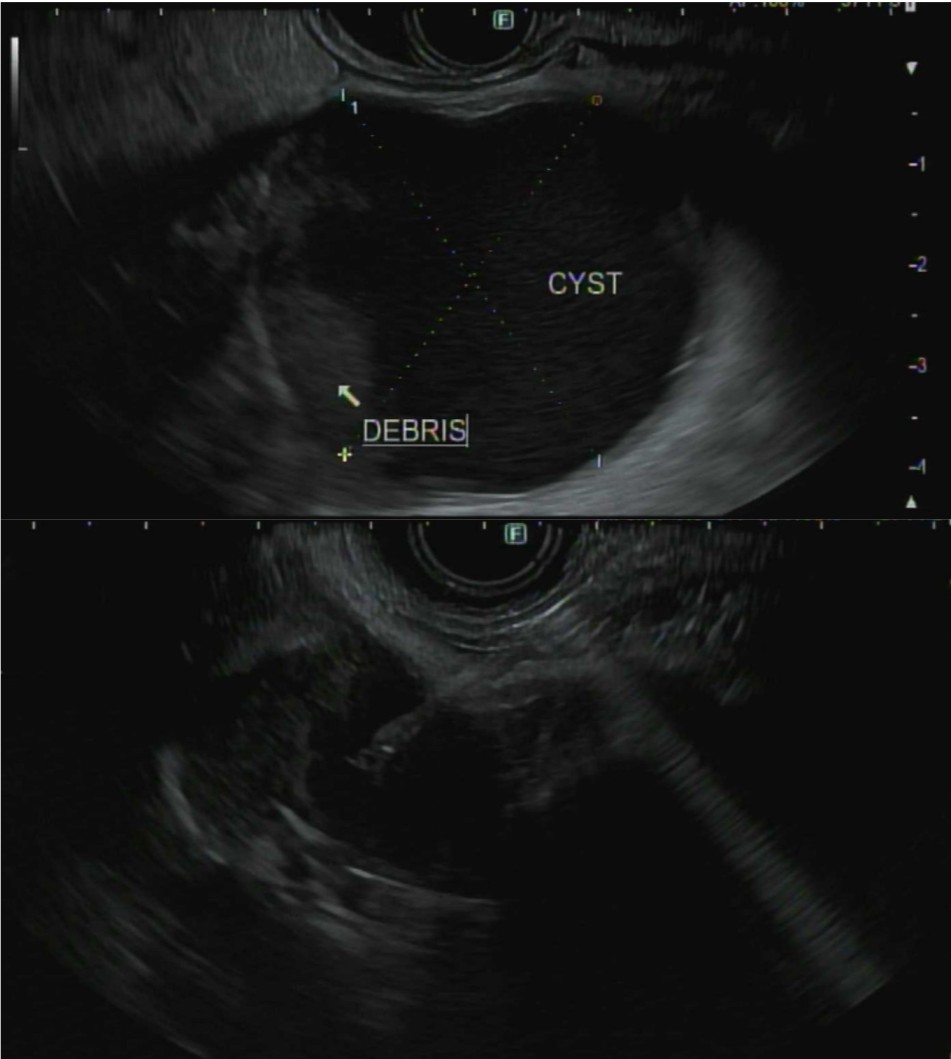
Figure: FIGURE 2A: 42 m cyst with debris, FIGURE 2B cyst fluid aspiration
Disclosures:
Qusai AlMasad indicated no relevant financial relationships.
Zaid Ansari indicated no relevant financial relationships.
Akram Ahmad indicated no relevant financial relationships.
Tilak Shah: Steris – Consultant.
Qusai AlMasad, MD1, Zaid Ansari, MD2, Akram Ahmad, MD2, Tilak Shah, MD2. P0239 - Evolution From a Large Intraductal Papillary Mucinous Neoplasm to Pseudocyst After Endoscopic Ultrasound-Guided Chemoablation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Roger Williams Medical Center, Providence, RI; 2Cleveland Clinic Florida, Weston, FL
Introduction: Endoscopic ultrasound (EUS) guided chemoablation has emerged as an option for treatment of intermediate-risk side branch intraductal papillary mucinous neoplasms (IPMNs), i.e. – IPMNs 2 – 5 cm in cross section and without mural nodules or main pancreatic duct dilation. In the CHARM and CHARM2 trials, chemoablation with paclitaxel and gemcitabine was associated with a durable response in about two-thirds of patients. The optimal workup and management of non-responders and those with interval growth who are not optimal surgical candidates is not well studied. We describe a patient with apparent interval growth after chemoablation, in whom cyst fluid analysis demonstrated replacement of mucinous cyst fluid with fluid more consistent with a benign pancreatic juice.
Case Description/
Methods: During routine surveillance, a 82-year-old woman was noted to have progressive increase in size of a cystic lesion in the pancreatic body from 1.5 cm to 4 cm over several years. EUS-guided cyst aspiration showed amylase 334 and CEA 155,785 consistent with a side branch IPMN. After discussion at the multidisciplinary pancreas tumor board, the patient underwent EUS guided chemoablation. Three months later, the cyst had decreased in size to 32 mm, so EUS guided chemoablation was repeated (cyst fluid CEA 432, glucose < 2, amylase 334). Two years later, MRI reported that cyst size was 4 cm. Layering internal debris was also noted. Repeat EUS-guided cyst fluid analysis showed amylase 32,421, glucose 77, and CEA 54. Based on layering debris and cyst fluid analysis, benign pancreatic juice was believed to be more likely than interval IPMN growth.
Discussion: We hypothesize that the patient had a complete or near complete response to chemoablation, but the large cyst cavity filled with pancreatic juice given its direct communication with a pancreatic duct sidebranch. EUS-guided chemoablation has only recently been incorporated in select tertiary centers. Our case highlights an important teaching point that has not been previously described. In “non-responders” or those with interval growth of a larger cyst, careful assessment of imaging features and repeat cyst fluid analysis can distinguish a “non-responder” from refill of the cavity with benign pancreatic juice.
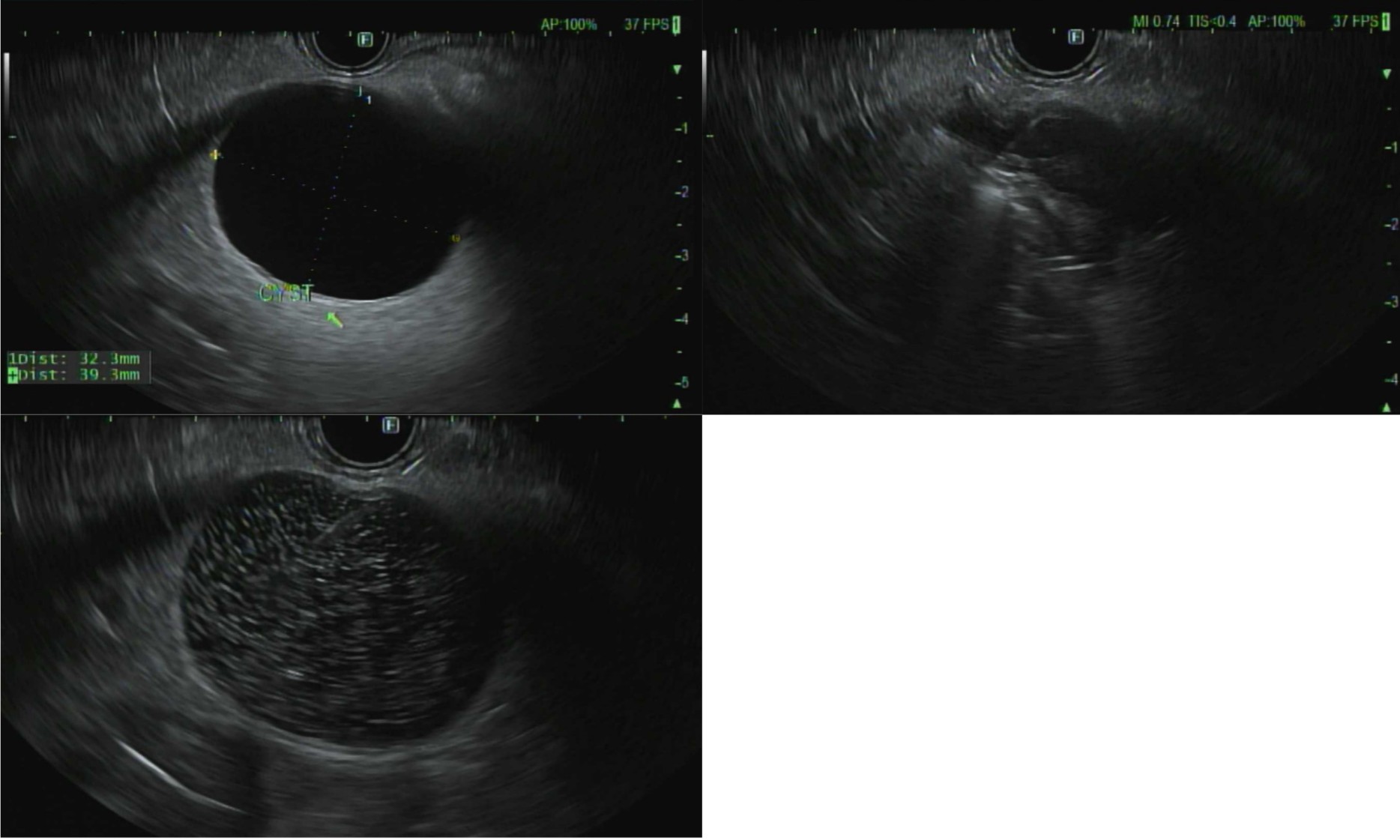
Figure: FIGURE 1A: Unilocular 4 cm cyst in pancreas body ;
1B near complete aspiration followed by 1C injection of an equal volume of paclitaxel and gemcitabine with
characteristic “snow-globe” appearance
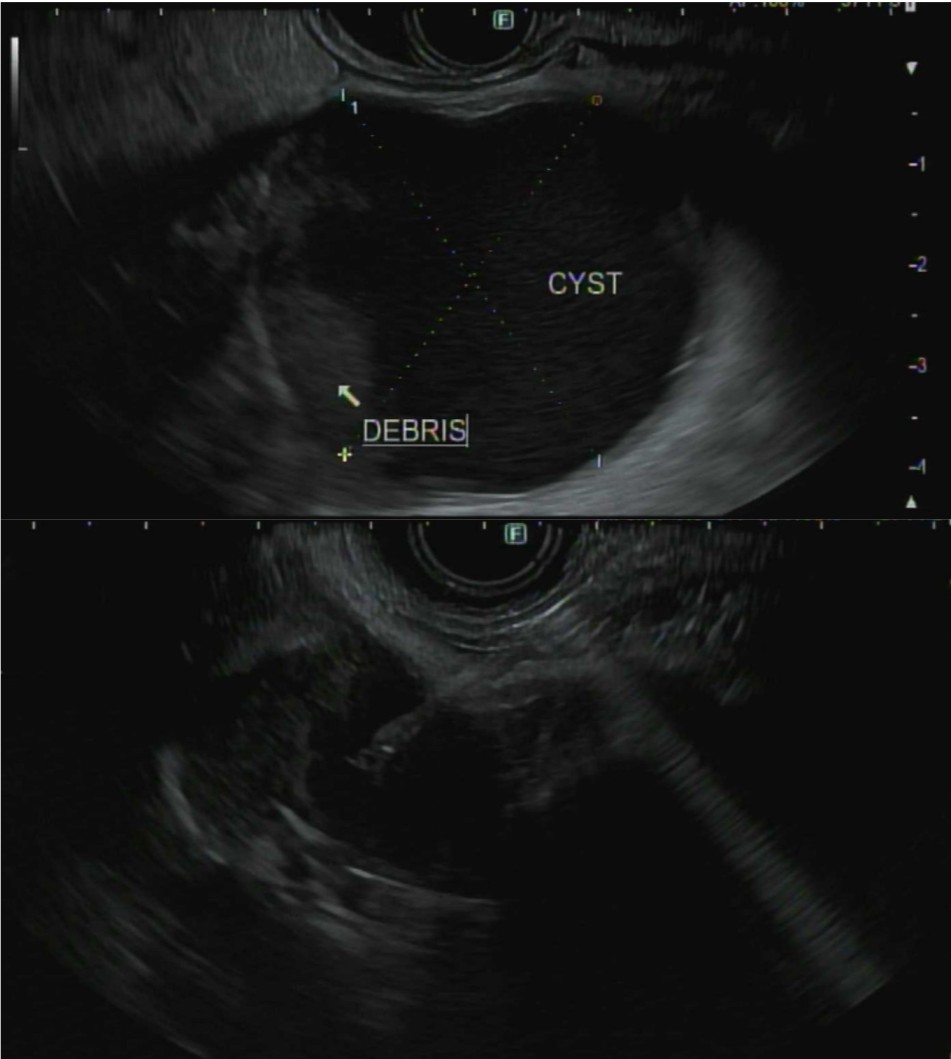
Figure: FIGURE 2A: 42 m cyst with debris, FIGURE 2B cyst fluid aspiration
Disclosures:
Qusai AlMasad indicated no relevant financial relationships.
Zaid Ansari indicated no relevant financial relationships.
Akram Ahmad indicated no relevant financial relationships.
Tilak Shah: Steris – Consultant.
Qusai AlMasad, MD1, Zaid Ansari, MD2, Akram Ahmad, MD2, Tilak Shah, MD2. P0239 - Evolution From a Large Intraductal Papillary Mucinous Neoplasm to Pseudocyst After Endoscopic Ultrasound-Guided Chemoablation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
