Sunday Poster Session
Category: Biliary/Pancreas
P0235 - Triple the Trouble: Unraveling the Mystery of PPP Syndrome (Pancreatitis, Panniculitis, and Polyarthritis) - A Case Report
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- MB
Mohannad Bitar, MD
Jamaica Hospital Medical Center
Jamaica, NY
Presenting Author(s)
Mohannad Bitar, MD1, Mushfiqur Siddique, MD1, Sajieh Naddaf, MD1, Hasan Al-Obaidi, MD2, Hayder Alamily, MD3
1Jamaica Hospital Medical Center, Jamaica, NY; 2University of Toledo College of Medicine and Life Sciences, Toledo, OH; 3University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: PPP syndrome (Pancreatitis, Panniculitis, Polyarthritis) is a rare disorder with fewer than
70 cases reported. It presents as a triad of polyarthritis with intraosseous fat necrosis,
lobular panniculitis, and pancreatitis (acute, chronic, or malignant). It results from systemic
release of pancreatic enzymes, particularly lipase, leading to fat necrosis and inflammation
in joints and subcutaneous tissues. Most patients are males in their 40s–70s with a history
of alcohol use and pancreatitis. The condition carries high morbidity and mortality,
particularly when associated with pancreatic malignancy.
Case Description/
Methods: A 72M with chronic pancreatitis, EtOH use disorder, and prostate cancer presented with acute pancreatitis, confirmed by elevated lipase and CT showing a pancreatic duct stone. He improved with IV fluids and was discharged. Weeks later, he returned with severe toe/knee pain, swelling, and nodular skin lesions. Rheumatology was consulted for concern of inflammatory arthritis and panniculitis. Arthrocentesis showed mildly inflammatory fluid without crystals. Migratory polyarthritis, nodules, and pancreatic disease raised concern for PPP syndrome. Imaging showed necrotic collections and pseudocysts. IV steroids were started; endoscopic drainage and stenting were performed. He developed complications, including infection, C. difficile colitis, and sepsis, requiring antibiotics, antifungals, and TPN. Despite temporary improvement, he had worsening peripancreatic collections with fistula and abscess formation, leading to septic shock and encephalopathy. Care was transitioned to comfort measures, and he ultimately passed away.
Discussion: PPP syndrome is a severe and underrecognized complication of pancreatic disease.
Diagnosis is clinical, supported by the classic triad and exclusion of other causes. In this
case, the syndrome was diagnosed based on characteristic joint, skin, and pancreatic
involvement, alongside supportive lab and imaging findings. Conservative management
often fails; surgical intervention may be curative if anatomical defects like fistulas are
identified. Early recognition and targeted treatment are critical, but even then, outcomes
remain poor. This case highlights the need for vigilance in patients with pancreatitis
presenting with systemic inflammatory symptoms.
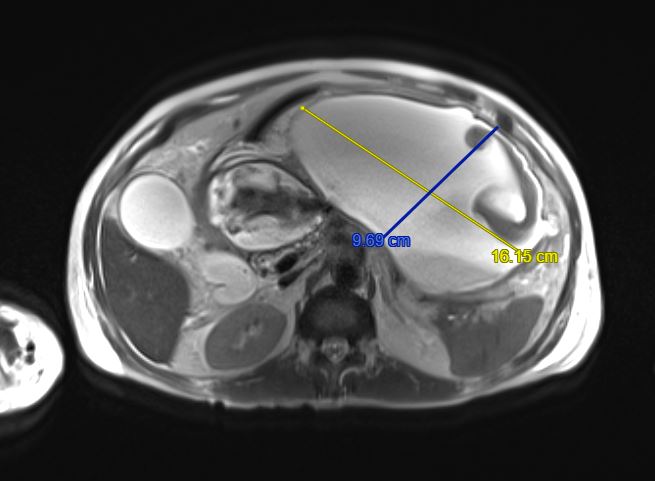
Figure: 16.2 cm peripancreatic fluid collection secondary to chronic pancreatitis
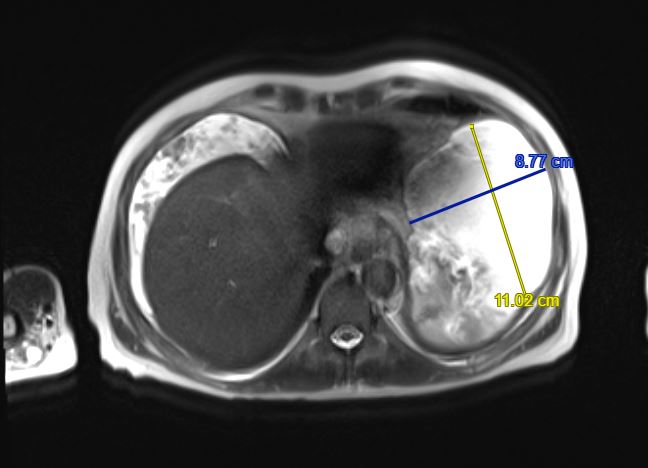
Figure: 11 cm peripancreatic fluid collection secondary to chronic pancreatitis
Disclosures:
Mohannad Bitar indicated no relevant financial relationships.
Mushfiqur Siddique indicated no relevant financial relationships.
Sajieh Naddaf indicated no relevant financial relationships.
Hasan Al-Obaidi indicated no relevant financial relationships.
Hayder Alamily indicated no relevant financial relationships.
Mohannad Bitar, MD1, Mushfiqur Siddique, MD1, Sajieh Naddaf, MD1, Hasan Al-Obaidi, MD2, Hayder Alamily, MD3. P0235 - Triple the Trouble: Unraveling the Mystery of PPP Syndrome (Pancreatitis, Panniculitis, and Polyarthritis) - A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Jamaica Hospital Medical Center, Jamaica, NY; 2University of Toledo College of Medicine and Life Sciences, Toledo, OH; 3University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: PPP syndrome (Pancreatitis, Panniculitis, Polyarthritis) is a rare disorder with fewer than
70 cases reported. It presents as a triad of polyarthritis with intraosseous fat necrosis,
lobular panniculitis, and pancreatitis (acute, chronic, or malignant). It results from systemic
release of pancreatic enzymes, particularly lipase, leading to fat necrosis and inflammation
in joints and subcutaneous tissues. Most patients are males in their 40s–70s with a history
of alcohol use and pancreatitis. The condition carries high morbidity and mortality,
particularly when associated with pancreatic malignancy.
Case Description/
Methods: A 72M with chronic pancreatitis, EtOH use disorder, and prostate cancer presented with acute pancreatitis, confirmed by elevated lipase and CT showing a pancreatic duct stone. He improved with IV fluids and was discharged. Weeks later, he returned with severe toe/knee pain, swelling, and nodular skin lesions. Rheumatology was consulted for concern of inflammatory arthritis and panniculitis. Arthrocentesis showed mildly inflammatory fluid without crystals. Migratory polyarthritis, nodules, and pancreatic disease raised concern for PPP syndrome. Imaging showed necrotic collections and pseudocysts. IV steroids were started; endoscopic drainage and stenting were performed. He developed complications, including infection, C. difficile colitis, and sepsis, requiring antibiotics, antifungals, and TPN. Despite temporary improvement, he had worsening peripancreatic collections with fistula and abscess formation, leading to septic shock and encephalopathy. Care was transitioned to comfort measures, and he ultimately passed away.
Discussion: PPP syndrome is a severe and underrecognized complication of pancreatic disease.
Diagnosis is clinical, supported by the classic triad and exclusion of other causes. In this
case, the syndrome was diagnosed based on characteristic joint, skin, and pancreatic
involvement, alongside supportive lab and imaging findings. Conservative management
often fails; surgical intervention may be curative if anatomical defects like fistulas are
identified. Early recognition and targeted treatment are critical, but even then, outcomes
remain poor. This case highlights the need for vigilance in patients with pancreatitis
presenting with systemic inflammatory symptoms.
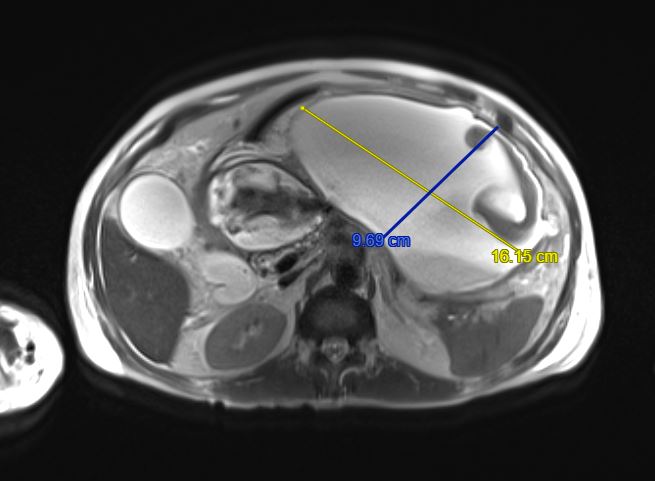
Figure: 16.2 cm peripancreatic fluid collection secondary to chronic pancreatitis
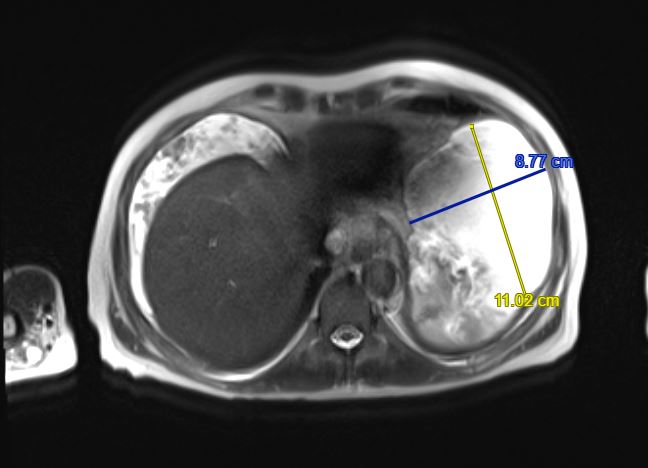
Figure: 11 cm peripancreatic fluid collection secondary to chronic pancreatitis
Disclosures:
Mohannad Bitar indicated no relevant financial relationships.
Mushfiqur Siddique indicated no relevant financial relationships.
Sajieh Naddaf indicated no relevant financial relationships.
Hasan Al-Obaidi indicated no relevant financial relationships.
Hayder Alamily indicated no relevant financial relationships.
Mohannad Bitar, MD1, Mushfiqur Siddique, MD1, Sajieh Naddaf, MD1, Hasan Al-Obaidi, MD2, Hayder Alamily, MD3. P0235 - Triple the Trouble: Unraveling the Mystery of PPP Syndrome (Pancreatitis, Panniculitis, and Polyarthritis) - A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
