Sunday Poster Session
Category: Biliary/Pancreas
P0234 - Adalimumab-Induced Necrotizing Pancreatitis Requiring Cystogastrostomy: A Rare Adverse Effect of TNF-Alpha Inhibitor Therapy
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Patt Panuncillon, DO
Ochsner Health Clinic Foundation, TX
Presenting Author(s)
Patt Panuncillon, DO1, Ruona Ebiai, MD2, Joanna Yuen, DO, MA3, Adil Memon, MD4, Anshuman Desai, MBBS2
1Ochsner Health Clinic Foundation, Pearland, TX; 2Ochsner Health Clinic Foundation, New Orleans, LA; 3Ochsner Health Clinic Foundation, Jefferson, LA; 4Ochsner Clinic Foundation, New Orleans, LA
Introduction: Necrotizing pancreatitis is a life-threatening complication of acute pancreatitis, characterized by tissue necrosis and a high risk of infection, organ failure, and mortality. While drug-induced pancreatitis is rare (1.4%-3.6% of cases), tumor necrosis factor-alpha (TNF-α) inhibitors like adalimumab have occasionally been implicated. However, progression to necrotizing pancreatitis requiring cystogastrostomy is exceedingly rare and, to our knowledge, previously unreported.
Case Description/
Methods: A 58-year-old man with psoriatic arthritis on adalimumab 40mg bi-weekly, presented with abdominal pain and fever. He had no history of alcohol use or cholelithiasis. He was diagnosed with severe acute pancreatitis and new-onset diabetes mellitus. His clinical course was complicated by Klebsiella bacteremia and persistent fevers despite broad-spectrum antibiotics. Workup for autoimmune pancreatitis, including IgG-4, was negative. Contrast-enhanced CT of the abdomen and pelvis revealed a large gas- and fluid-filled collection (15.6 × 7.2 cm) replacing the majority of the pancreatic parenchyma, consistent with necrotizing pancreatitis. General surgery recommended non-operative management. Interventional radiology placed a percutaneous drain, which cultured positive for Klebsiella. Follow-up imaging showed no improvement, with persistent walled-off necrosis replacing nearly the entire pancreas and an obliterated splenic vein. An attempt to upsize the drain was unsuccessful. Due to continued leukocytosis and fevers, the patient was transferred to our tertiary care center for advanced endoscopic management. He underwent endoscopic cystogastrostomy with placement of a lumen-apposing metal stent and required 13 serial endoscopic necrosectomies. Despite partial improvement, he ultimately required surgical intervention. He underwent exploratory laparotomy with open cystogastrostomy, externalized cyst drainage, cholecystectomy, and jejunal feeding tube placement. Serum adalimumab level was not available prior to or during admission.
Discussion: Adalimumab-induced pancreatitis is extremely rare, with most reports describing mild, self-limited cases that resolve after drug discontinuation. To date, there are no published cases of adalimumab-associated pancreatitis progressing to necrotizing pancreatitis requiring cystogastrostomy. Our case highlights a severe presentation necessitating step-up therapy including endoscopic and surgical intervention, expanding the clinical spectrum of this rare adverse effect.
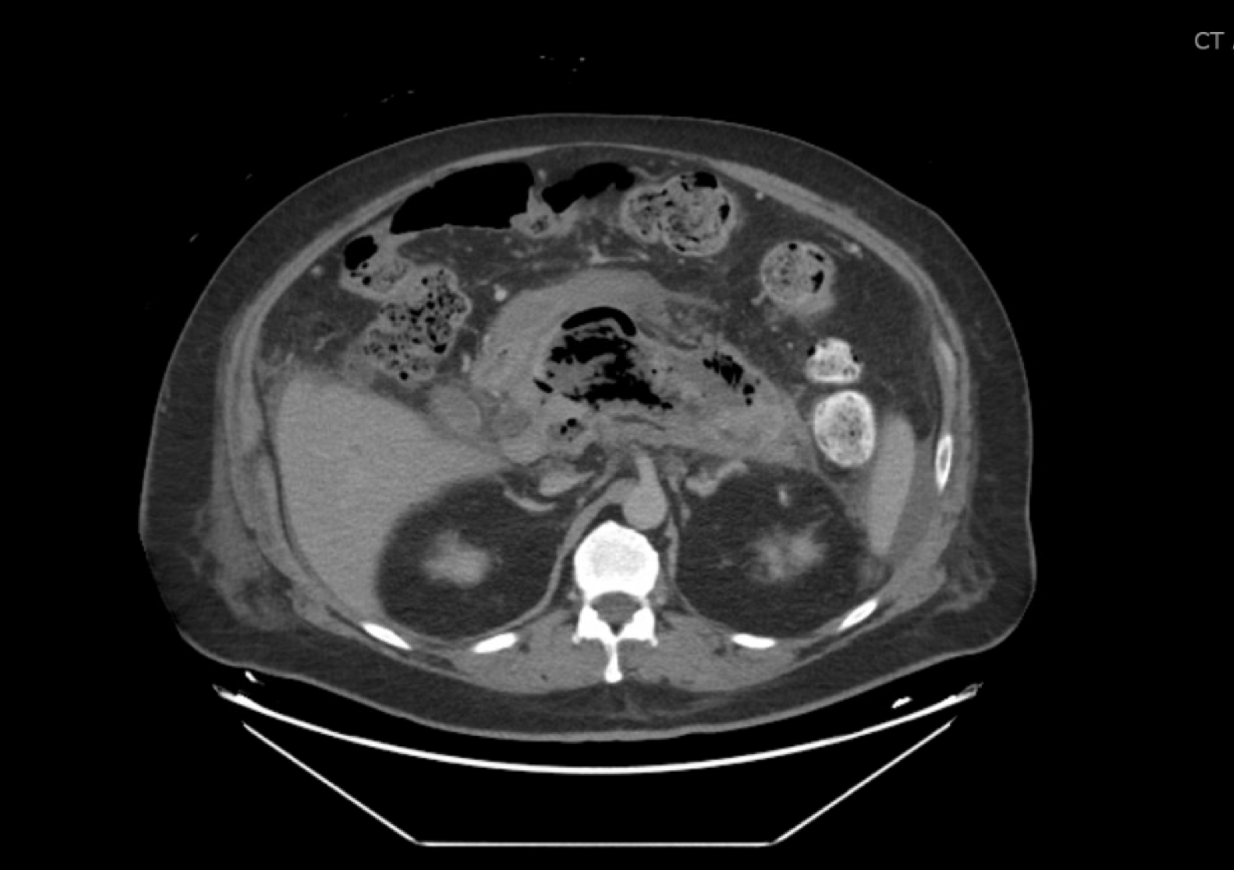
Figure: Figure 1. CTAP showing pancreatic necrosis
Disclosures:
Patt Panuncillon indicated no relevant financial relationships.
Ruona Ebiai indicated no relevant financial relationships.
Joanna Yuen indicated no relevant financial relationships.
Adil Memon indicated no relevant financial relationships.
Anshuman Desai indicated no relevant financial relationships.
Patt Panuncillon, DO1, Ruona Ebiai, MD2, Joanna Yuen, DO, MA3, Adil Memon, MD4, Anshuman Desai, MBBS2. P0234 - Adalimumab-Induced Necrotizing Pancreatitis Requiring Cystogastrostomy: A Rare Adverse Effect of TNF-Alpha Inhibitor Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Ochsner Health Clinic Foundation, Pearland, TX; 2Ochsner Health Clinic Foundation, New Orleans, LA; 3Ochsner Health Clinic Foundation, Jefferson, LA; 4Ochsner Clinic Foundation, New Orleans, LA
Introduction: Necrotizing pancreatitis is a life-threatening complication of acute pancreatitis, characterized by tissue necrosis and a high risk of infection, organ failure, and mortality. While drug-induced pancreatitis is rare (1.4%-3.6% of cases), tumor necrosis factor-alpha (TNF-α) inhibitors like adalimumab have occasionally been implicated. However, progression to necrotizing pancreatitis requiring cystogastrostomy is exceedingly rare and, to our knowledge, previously unreported.
Case Description/
Methods: A 58-year-old man with psoriatic arthritis on adalimumab 40mg bi-weekly, presented with abdominal pain and fever. He had no history of alcohol use or cholelithiasis. He was diagnosed with severe acute pancreatitis and new-onset diabetes mellitus. His clinical course was complicated by Klebsiella bacteremia and persistent fevers despite broad-spectrum antibiotics. Workup for autoimmune pancreatitis, including IgG-4, was negative. Contrast-enhanced CT of the abdomen and pelvis revealed a large gas- and fluid-filled collection (15.6 × 7.2 cm) replacing the majority of the pancreatic parenchyma, consistent with necrotizing pancreatitis. General surgery recommended non-operative management. Interventional radiology placed a percutaneous drain, which cultured positive for Klebsiella. Follow-up imaging showed no improvement, with persistent walled-off necrosis replacing nearly the entire pancreas and an obliterated splenic vein. An attempt to upsize the drain was unsuccessful. Due to continued leukocytosis and fevers, the patient was transferred to our tertiary care center for advanced endoscopic management. He underwent endoscopic cystogastrostomy with placement of a lumen-apposing metal stent and required 13 serial endoscopic necrosectomies. Despite partial improvement, he ultimately required surgical intervention. He underwent exploratory laparotomy with open cystogastrostomy, externalized cyst drainage, cholecystectomy, and jejunal feeding tube placement. Serum adalimumab level was not available prior to or during admission.
Discussion: Adalimumab-induced pancreatitis is extremely rare, with most reports describing mild, self-limited cases that resolve after drug discontinuation. To date, there are no published cases of adalimumab-associated pancreatitis progressing to necrotizing pancreatitis requiring cystogastrostomy. Our case highlights a severe presentation necessitating step-up therapy including endoscopic and surgical intervention, expanding the clinical spectrum of this rare adverse effect.
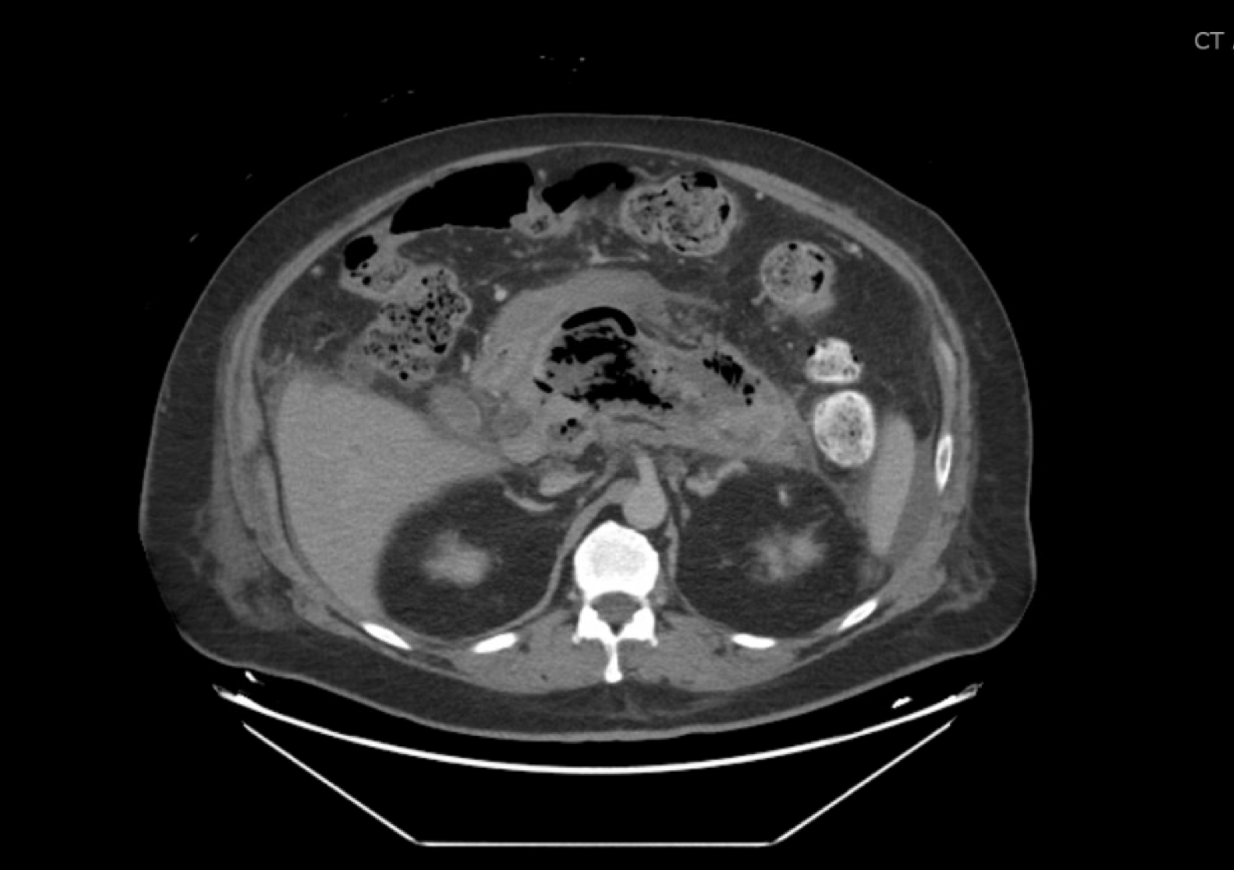
Figure: Figure 1. CTAP showing pancreatic necrosis
Disclosures:
Patt Panuncillon indicated no relevant financial relationships.
Ruona Ebiai indicated no relevant financial relationships.
Joanna Yuen indicated no relevant financial relationships.
Adil Memon indicated no relevant financial relationships.
Anshuman Desai indicated no relevant financial relationships.
Patt Panuncillon, DO1, Ruona Ebiai, MD2, Joanna Yuen, DO, MA3, Adil Memon, MD4, Anshuman Desai, MBBS2. P0234 - Adalimumab-Induced Necrotizing Pancreatitis Requiring Cystogastrostomy: A Rare Adverse Effect of TNF-Alpha Inhibitor Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
