Sunday Poster Session
Category: Biliary/Pancreas
P0233 - Beyond Gallstones: A Rare Case of Pancreatitis From Lemmel Syndrome
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Maria J. Cornier Martinez, MD, MPH (she/her/hers)
VA Caribbean Healthcare System
San Juan, PR
Presenting Author(s)
Maria J. Cornier Martinez, MD, MPH, Juan G. Feliciano-Figueroa, MD, Pamela A. Merheb Finianos, MD, Loscar Santiago-Rivera, MD
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Duodenal diverticula are mostly asymptomatic; however, in ~5% of cases, periampullary diverticula (located 2–3 cm from the ampulla of Vater) can compress the common bile duct or pancreatic duct, leading to ductal dilation and obstruction — a condition known as Lemmel Syndrome. Due to its rarity, no standardized approach exists for diagnosis or treatment, but it is crucial to include it in the differential diagnosis for biliary obstruction or pancreatitis without gallstones.
Case Description/
Methods: We present a 79-year-old male with a history of type 2 diabetes, hypertension, and dysphagia, transferred to our emergency department for presumed pancreatitis. He reported sudden-onset epigastric pain after breakfast, without radiation to the back, chest, or neck, accompanied by nausea and vomiting. He denied any other symptoms.
Laboratory results revealed markedly elevated lipase ( >3000 U/L), amylase (3423 U/L), AST (343 U/L), ALT (297 U/L), and total bilirubin (5.94 mg/dL, direct predominance). Abdominal-pelvic CT with contrast showed peripancreatic fat stranding and fluid consistent with pancreatitis, biliary ductal dilation, and a duodenal diverticulum. Abdominal ultrasound confirmed absence of gallstones. MRI/MRCP revealed biliary dilation without choledochal filling defects and a prominent duodenal diverticulum near the ampulla.
The patient was not on medications known to induce pancreatitis, and his triglyceride level was normal (88 mg/dL). Given these findings, the diagnosis of Lemmel Syndrome was made, where the periampullary diverticulum caused biliary obstruction leading to pancreatitis. Considering the patient’s age and comorbidities, a conservative (non-surgical) management approach was taken, leading to full recovery.
Discussion: This case highlights the importance of considering rare causes of biliary obstruction, such as Lemmel Syndrome, particularly in the absence of gallstones or other common etiologies. Multiple imaging modalities (CT, ultrasound, MRCP) were essential for reaching the correct diagnosis. Management strategies should be individualized, balancing risks and benefits based on the patient’s overall health and clinical presentation.
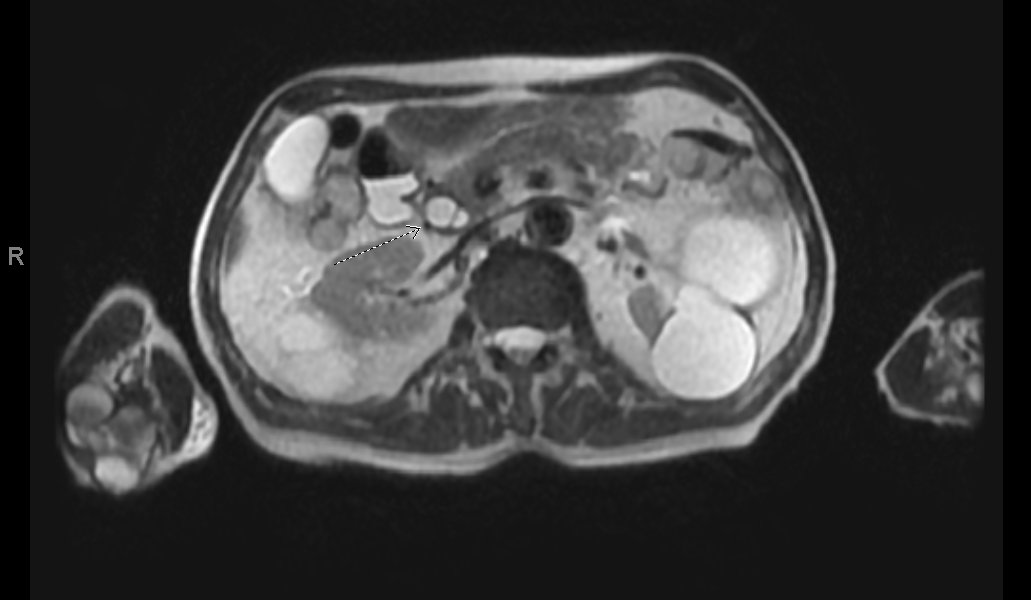
Figure: Large periampullary duodenal diverticulum seen on MRCP
Disclosures:
Maria Cornier Martinez indicated no relevant financial relationships.
Juan G. Feliciano-Figueroa indicated no relevant financial relationships.
Pamela Merheb Finianos indicated no relevant financial relationships.
Loscar Santiago-Rivera indicated no relevant financial relationships.
Maria J. Cornier Martinez, MD, MPH, Juan G. Feliciano-Figueroa, MD, Pamela A. Merheb Finianos, MD, Loscar Santiago-Rivera, MD. P0233 - Beyond Gallstones: A Rare Case of Pancreatitis From Lemmel Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Duodenal diverticula are mostly asymptomatic; however, in ~5% of cases, periampullary diverticula (located 2–3 cm from the ampulla of Vater) can compress the common bile duct or pancreatic duct, leading to ductal dilation and obstruction — a condition known as Lemmel Syndrome. Due to its rarity, no standardized approach exists for diagnosis or treatment, but it is crucial to include it in the differential diagnosis for biliary obstruction or pancreatitis without gallstones.
Case Description/
Methods: We present a 79-year-old male with a history of type 2 diabetes, hypertension, and dysphagia, transferred to our emergency department for presumed pancreatitis. He reported sudden-onset epigastric pain after breakfast, without radiation to the back, chest, or neck, accompanied by nausea and vomiting. He denied any other symptoms.
Laboratory results revealed markedly elevated lipase ( >3000 U/L), amylase (3423 U/L), AST (343 U/L), ALT (297 U/L), and total bilirubin (5.94 mg/dL, direct predominance). Abdominal-pelvic CT with contrast showed peripancreatic fat stranding and fluid consistent with pancreatitis, biliary ductal dilation, and a duodenal diverticulum. Abdominal ultrasound confirmed absence of gallstones. MRI/MRCP revealed biliary dilation without choledochal filling defects and a prominent duodenal diverticulum near the ampulla.
The patient was not on medications known to induce pancreatitis, and his triglyceride level was normal (88 mg/dL). Given these findings, the diagnosis of Lemmel Syndrome was made, where the periampullary diverticulum caused biliary obstruction leading to pancreatitis. Considering the patient’s age and comorbidities, a conservative (non-surgical) management approach was taken, leading to full recovery.
Discussion: This case highlights the importance of considering rare causes of biliary obstruction, such as Lemmel Syndrome, particularly in the absence of gallstones or other common etiologies. Multiple imaging modalities (CT, ultrasound, MRCP) were essential for reaching the correct diagnosis. Management strategies should be individualized, balancing risks and benefits based on the patient’s overall health and clinical presentation.
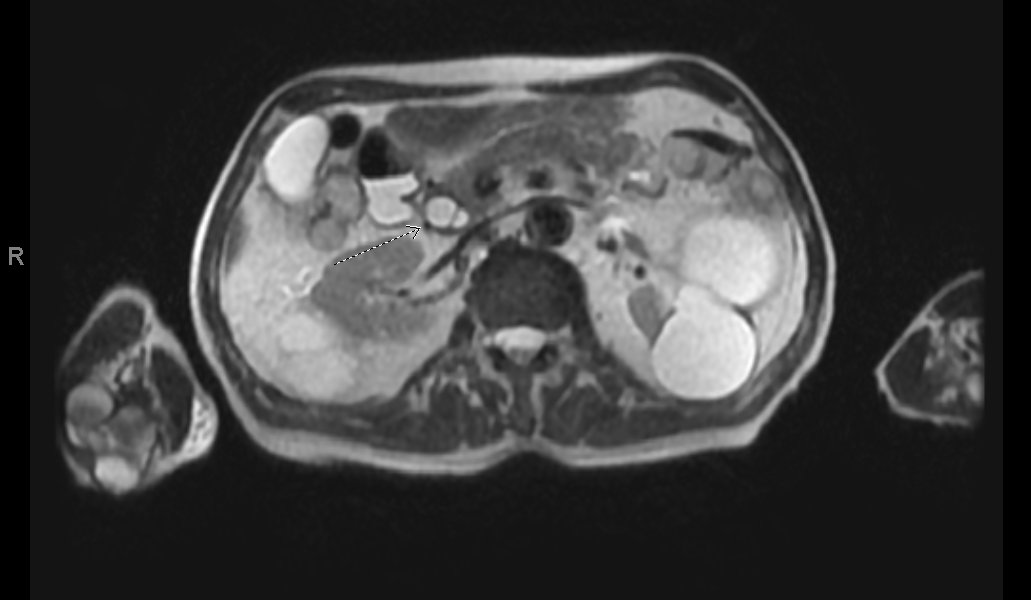
Figure: Large periampullary duodenal diverticulum seen on MRCP
Disclosures:
Maria Cornier Martinez indicated no relevant financial relationships.
Juan G. Feliciano-Figueroa indicated no relevant financial relationships.
Pamela Merheb Finianos indicated no relevant financial relationships.
Loscar Santiago-Rivera indicated no relevant financial relationships.
Maria J. Cornier Martinez, MD, MPH, Juan G. Feliciano-Figueroa, MD, Pamela A. Merheb Finianos, MD, Loscar Santiago-Rivera, MD. P0233 - Beyond Gallstones: A Rare Case of Pancreatitis From Lemmel Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
