Sunday Poster Session
Category: Biliary/Pancreas
P0200 - Always Look Both Ways When Crossing the Street: The Importance of Pancreatic Imaging During EUS When Evaluating an Intrahepatic Mass
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Benjamin M. Berg
Touro University of California
Vallejo, CA
Presenting Author(s)
Benjamin M. Berg, 1, Russell Hollis, MD, MBA2, Noah Storch, 3, Ian Storch, DO, FACG4
1Touro University of California, Vallejo, CA; 2North Shore University Hospital - Northwell Health, Manhasset, NY; 3Syosset High School, Woodbury, NY; 4Gastroenterology Consultants of Long Island, Woodbury, NY
Introduction: Intrahepatic Cholangiocarcinoma (IC) carries a poor prognosis, making early detection and resection crucial. Benign conditions, however, such as immunoglobulin G4-associated cholangitis (IAC), related to autoimmune pancreatitis (AIP), may present with a similar-appearing liver lesion and are treated medically. This case illustrates the importance of carefully examining the pancreas during endoscopic ultrasound (EUS) of presumed IC.
Case Description/
Methods: A 65-year-old hispanic woman with a history of cholecystectomy presented with epigastric pain. Her physical exam was unrevealing, and labs displayed mildly elevated AST (85), ALT (59), and ALP (158) with normal bilirubin. Upper endoscopy was normal, but transabdominal ultrasound revealed a medial lobe liver lesion (3.3 x 1.7 x 3.2 cm) and a 1 cm common bile duct. Magnetic resonance cholangiopancreatography (MRI/MRCP) revealed features concerning for cholangiocarcinoma with possible portal vein invasion. Although serum CA 19-9 was within normal limits, the patient was referred to a surgeon who determined that the lesion was resectable and recommended preoperative Endoscopic Ultrasound (EUS) to better characterize the lesion. EUS visualized the mass but also revealed a heterogeneous, hyperechoic pancreas suggestive of AIP. Fine-needle aspiration (FNA) of both the pancreas and liver lesion showed benign cells with IgG4-positive lymphocytes. Serum IgG4 levels were significantly elevated. After one month on prednisone, the serum IgG4 levels declined, and the liver lesion decreased in size. Mercaptopurine was started, and at three months, IgG4 levels normalized with complete resolution of the liver mass.
Discussion: IgG4-related disease (IgG4-RD) is a systemic condition affecting multiple organs. Rarely, IAC can present as a “pseudo tumorous mass” and can mimic IC. The HISORt criteria for IAC require histology, imaging, serology, other organ involvement (commonly the pancreas), and response to steroids. CA 19-9 and IgG4 levels lack specificity, complicating the diagnosis. Prompt diagnosis is crucial, as delay in treatment of IAC can be fatal. In this case, pancreatic abnormalities on EUS prompted further investigation, confirming AIP and IAC, helping to substantiate the diagnosis and leading to immunosuppressive treatment instead of surgery. This case highlights the importance of evaluating not only the hepatic pathology but also the pancreas during EUS in patients with suspected IC, potentially preventing unnecessary surgical intervention.
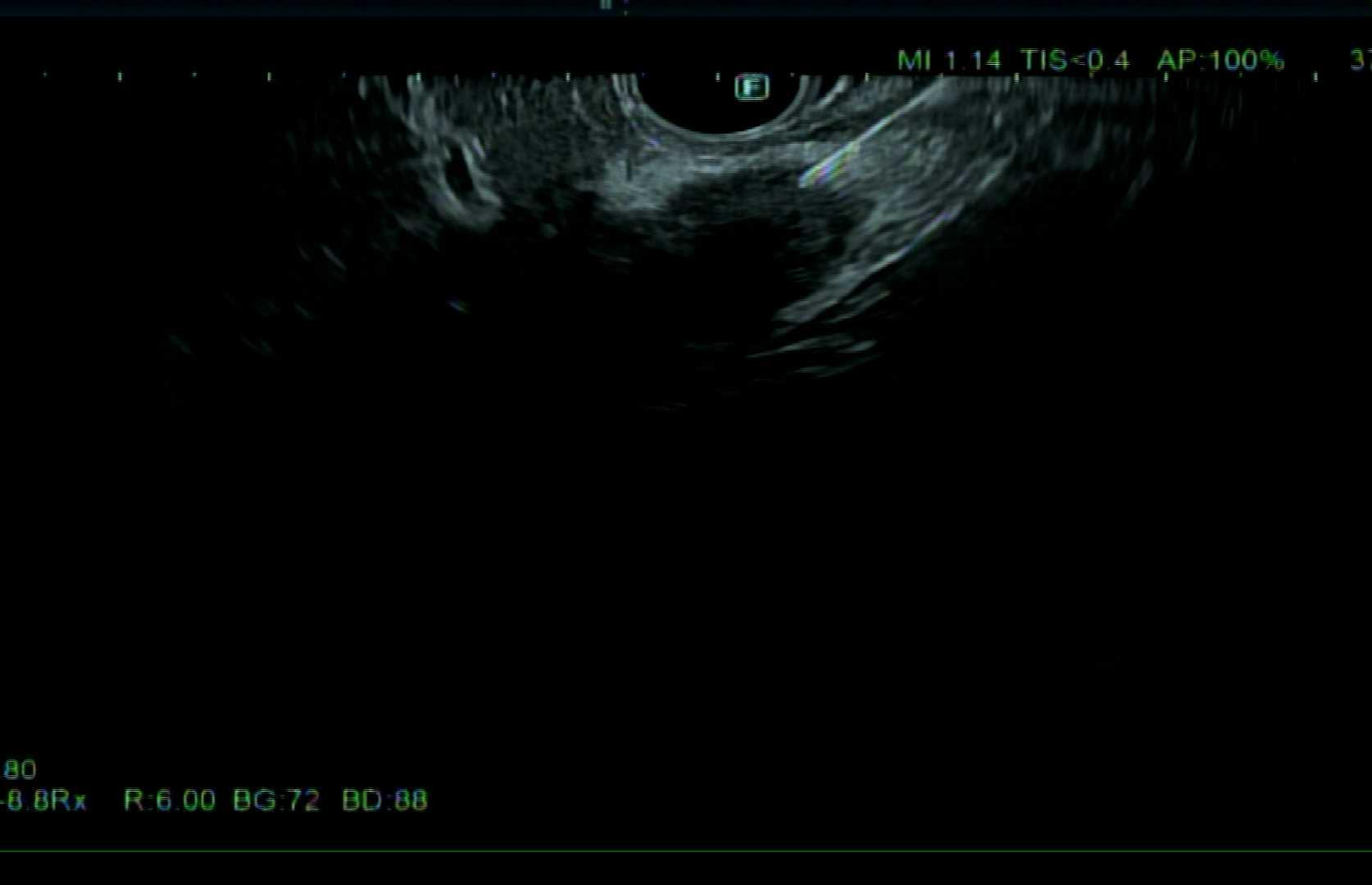
Figure: Body of pancreas with findings consistent with autoimmune pancreatitis

Figure: Intrahepatic Cholangiocarinoma with fine needle aspirate
Disclosures:
Benjamin Berg indicated no relevant financial relationships.
Russell Hollis indicated no relevant financial relationships.
Noah Storch indicated no relevant financial relationships.
Ian Storch: CasoVision Inc. – Consultant, Owner/Ownership Interest.
Benjamin M. Berg, 1, Russell Hollis, MD, MBA2, Noah Storch, 3, Ian Storch, DO, FACG4. P0200 - Always Look Both Ways When Crossing the Street: The Importance of Pancreatic Imaging During EUS When Evaluating an Intrahepatic Mass, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Touro University of California, Vallejo, CA; 2North Shore University Hospital - Northwell Health, Manhasset, NY; 3Syosset High School, Woodbury, NY; 4Gastroenterology Consultants of Long Island, Woodbury, NY
Introduction: Intrahepatic Cholangiocarcinoma (IC) carries a poor prognosis, making early detection and resection crucial. Benign conditions, however, such as immunoglobulin G4-associated cholangitis (IAC), related to autoimmune pancreatitis (AIP), may present with a similar-appearing liver lesion and are treated medically. This case illustrates the importance of carefully examining the pancreas during endoscopic ultrasound (EUS) of presumed IC.
Case Description/
Methods: A 65-year-old hispanic woman with a history of cholecystectomy presented with epigastric pain. Her physical exam was unrevealing, and labs displayed mildly elevated AST (85), ALT (59), and ALP (158) with normal bilirubin. Upper endoscopy was normal, but transabdominal ultrasound revealed a medial lobe liver lesion (3.3 x 1.7 x 3.2 cm) and a 1 cm common bile duct. Magnetic resonance cholangiopancreatography (MRI/MRCP) revealed features concerning for cholangiocarcinoma with possible portal vein invasion. Although serum CA 19-9 was within normal limits, the patient was referred to a surgeon who determined that the lesion was resectable and recommended preoperative Endoscopic Ultrasound (EUS) to better characterize the lesion. EUS visualized the mass but also revealed a heterogeneous, hyperechoic pancreas suggestive of AIP. Fine-needle aspiration (FNA) of both the pancreas and liver lesion showed benign cells with IgG4-positive lymphocytes. Serum IgG4 levels were significantly elevated. After one month on prednisone, the serum IgG4 levels declined, and the liver lesion decreased in size. Mercaptopurine was started, and at three months, IgG4 levels normalized with complete resolution of the liver mass.
Discussion: IgG4-related disease (IgG4-RD) is a systemic condition affecting multiple organs. Rarely, IAC can present as a “pseudo tumorous mass” and can mimic IC. The HISORt criteria for IAC require histology, imaging, serology, other organ involvement (commonly the pancreas), and response to steroids. CA 19-9 and IgG4 levels lack specificity, complicating the diagnosis. Prompt diagnosis is crucial, as delay in treatment of IAC can be fatal. In this case, pancreatic abnormalities on EUS prompted further investigation, confirming AIP and IAC, helping to substantiate the diagnosis and leading to immunosuppressive treatment instead of surgery. This case highlights the importance of evaluating not only the hepatic pathology but also the pancreas during EUS in patients with suspected IC, potentially preventing unnecessary surgical intervention.
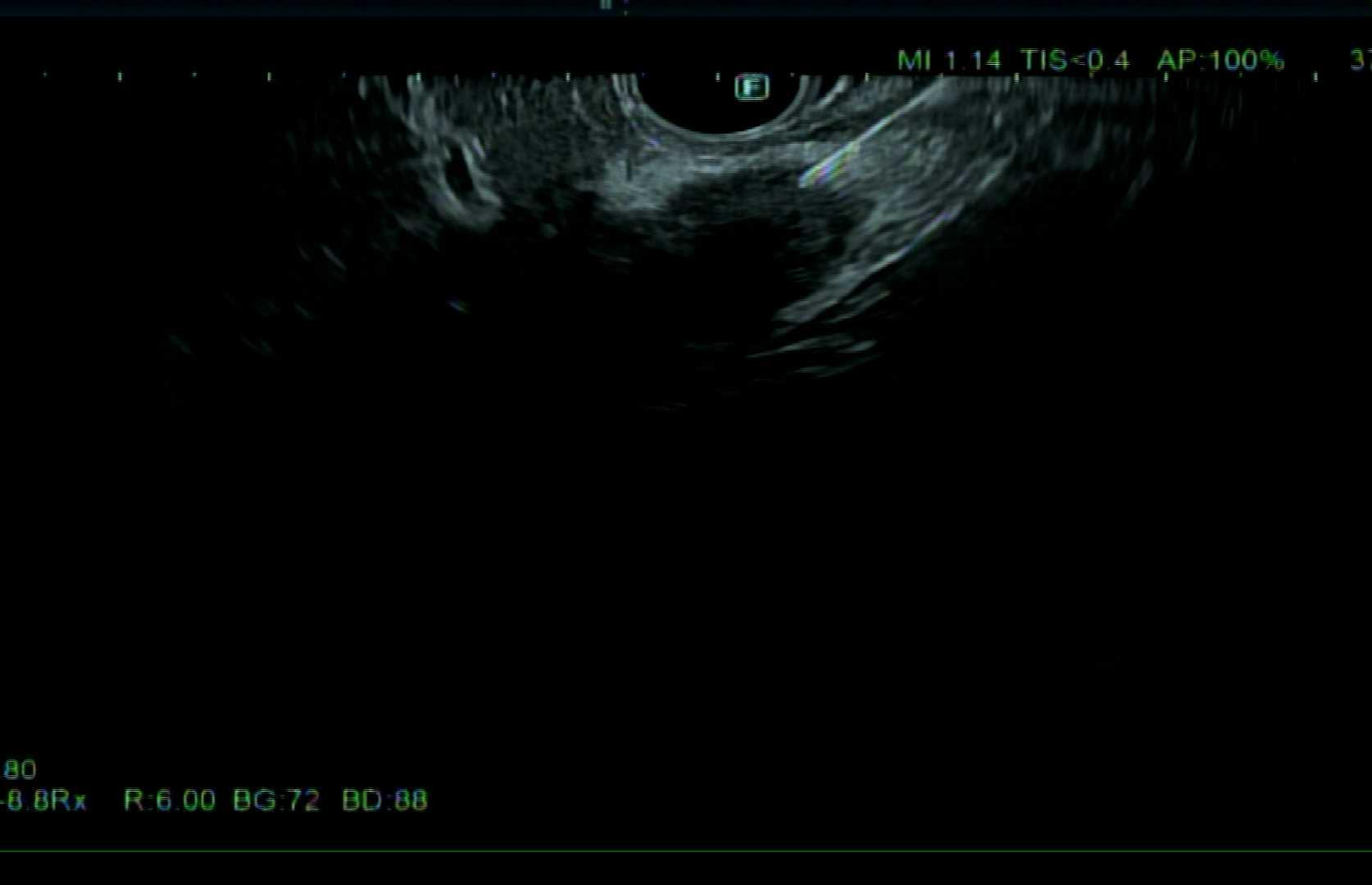
Figure: Body of pancreas with findings consistent with autoimmune pancreatitis

Figure: Intrahepatic Cholangiocarinoma with fine needle aspirate
Disclosures:
Benjamin Berg indicated no relevant financial relationships.
Russell Hollis indicated no relevant financial relationships.
Noah Storch indicated no relevant financial relationships.
Ian Storch: CasoVision Inc. – Consultant, Owner/Ownership Interest.
Benjamin M. Berg, 1, Russell Hollis, MD, MBA2, Noah Storch, 3, Ian Storch, DO, FACG4. P0200 - Always Look Both Ways When Crossing the Street: The Importance of Pancreatic Imaging During EUS When Evaluating an Intrahepatic Mass, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
