Sunday Poster Session
Category: Biliary/Pancreas
P0199 - Type III Mirizzi Syndrome: A Case of Diagnostic Challenge and Surgical Management
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rishika Trivedi, MD
DHR Health
McAllen, TX
Presenting Author(s)
Rishika Trivedi, MD1, Mahmoud Barbarawi, MD1, Prince Shah-Riar, MD2, Tapan Patel, MD3, Asif Zamir, MD, FACG4, Murthy Badiga, MD, FACG3
1DHR Health, McAllen, TX; 2DHR Health, Edinburg, Tx, McAllen, TX; 3DHR Health Gastroenterology, McAllen, TX; 4DHR Health Gastroenterology, Edinburg, TX
Introduction: Mirizzi syndrome is an uncommon cause of obstructive jaundice due to extrinsic compression of the common bile duct (CBD) by an impacted stone in the cystic duct or gallbladder infundibulum. Type III Mirizzi syndrome is rare, accounting for less than 0.1-0.5% of all cases of gallstone-related surgeries. Diagnosis can be inconclusive, often requiring multiple imaging modalities and invasive interventions. We present a case of type III Mirizzi syndrome requiring multiple ERCPs and surgical exploration for diagnosis and treatment.
Case Description/
Methods: A 65-year-old female with a history of fatty liver presented with two weeks of epigastric pain, jaundice, pruritus, and decreased appetite. She was hemodynamically stable but icteric. Labs showed AST 111, ALT 207, ALP 459, total bilirubin 13.4, and direct bilirubin 11.36, consistent with a cholestatic pattern. Ultrasound revealed a dilated CBD. ERCP demonstrated CBD dilation with extrinsic compression, but no visible stones. A biliary sphincterotomy was performed. Persistent jaundice and elevated liver enzymes led to an MRCP, which showed a filling defect at the cystic duct-CBD junction. A second ERCP with Spyglass cholangioscopy identified a large, impacted stone at the cystic duct origin, compressing the CBD. Electrohydraulic lithotripsy was performed, and multiple stone fragments were removed (Figure 1A–D). Despite initial improvement, definitive diagnosis remained uncertain. The patient underwent surgical exploration by the hepatobiliary team. Intraoperative findings revealed an intrahepatic gallbladder with a large stone eroding into the bile duct wall, consistent with type III Mirrizi syndrome. A cholecystobiliary fistula and partial destruction of the CBD were identified. The bile duct was resected, and Roux-en-Y hepaticojejunostomy was performed. The patient recovered well and was discharged with follow-up.
Discussion: This case highlights the diagnostic complexity of type III Mirizzi syndrome, a rare entity that is both clinically and radiographically challenging to diagnose. Initial ERCP and MRCP may be inconclusive. Advanced cholangioscopy and surgical exploration are often required. A multi-disciplinary approach must be considered for diagnosis and treatment.
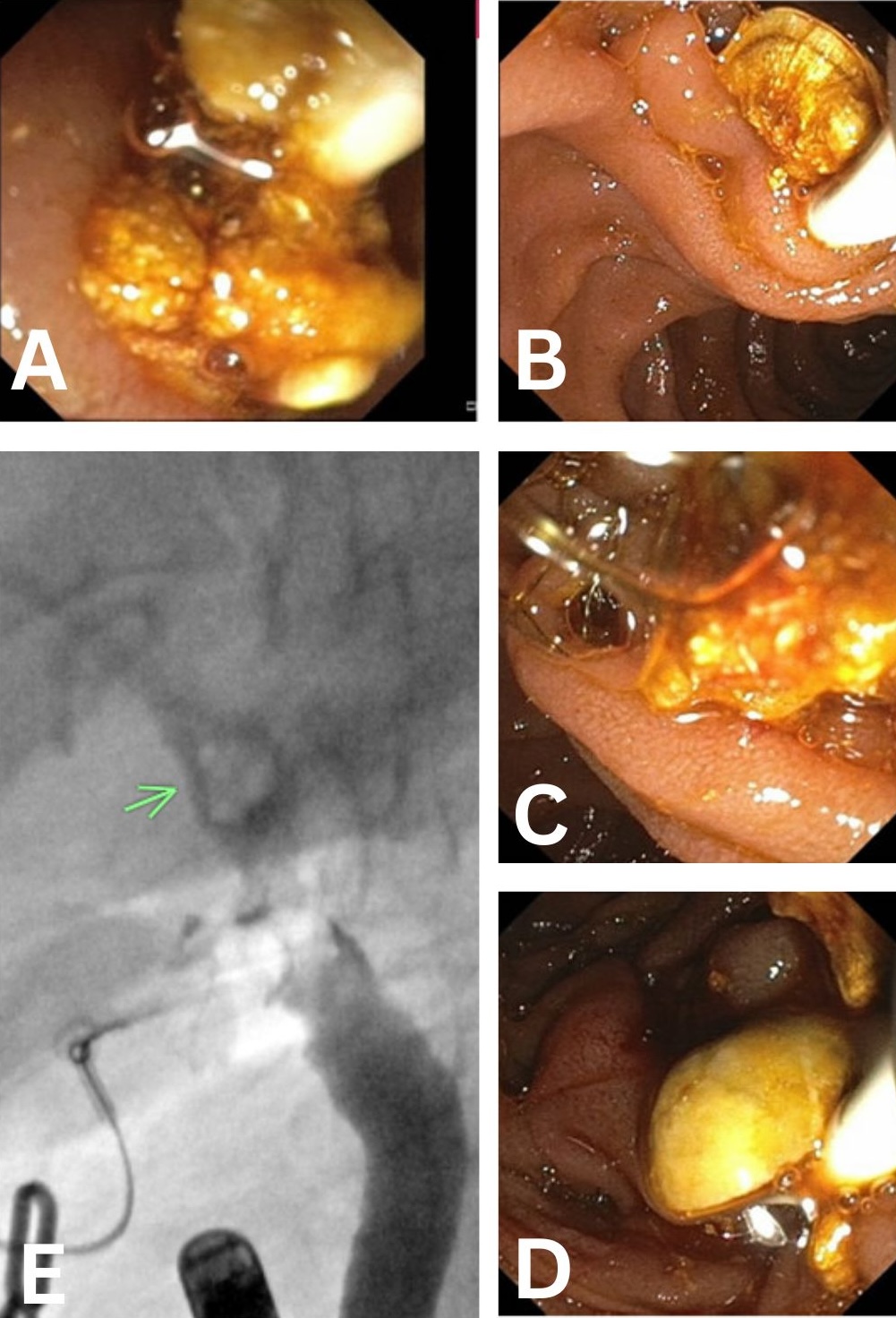
Figure: Endoscopic and fluoroscopic evaluation revealed a large, impacted stone at the cystic duct take-off causing biliary dilation, consistent with Mirizzi syndrome (Figure 1A–D).
Disclosures:
Rishika Trivedi indicated no relevant financial relationships.
Mahmoud Barbarawi indicated no relevant financial relationships.
Prince Shah-Riar indicated no relevant financial relationships.
Tapan Patel indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Murthy Badiga indicated no relevant financial relationships.
Rishika Trivedi, MD1, Mahmoud Barbarawi, MD1, Prince Shah-Riar, MD2, Tapan Patel, MD3, Asif Zamir, MD, FACG4, Murthy Badiga, MD, FACG3. P0199 - Type III Mirizzi Syndrome: A Case of Diagnostic Challenge and Surgical Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1DHR Health, McAllen, TX; 2DHR Health, Edinburg, Tx, McAllen, TX; 3DHR Health Gastroenterology, McAllen, TX; 4DHR Health Gastroenterology, Edinburg, TX
Introduction: Mirizzi syndrome is an uncommon cause of obstructive jaundice due to extrinsic compression of the common bile duct (CBD) by an impacted stone in the cystic duct or gallbladder infundibulum. Type III Mirizzi syndrome is rare, accounting for less than 0.1-0.5% of all cases of gallstone-related surgeries. Diagnosis can be inconclusive, often requiring multiple imaging modalities and invasive interventions. We present a case of type III Mirizzi syndrome requiring multiple ERCPs and surgical exploration for diagnosis and treatment.
Case Description/
Methods: A 65-year-old female with a history of fatty liver presented with two weeks of epigastric pain, jaundice, pruritus, and decreased appetite. She was hemodynamically stable but icteric. Labs showed AST 111, ALT 207, ALP 459, total bilirubin 13.4, and direct bilirubin 11.36, consistent with a cholestatic pattern. Ultrasound revealed a dilated CBD. ERCP demonstrated CBD dilation with extrinsic compression, but no visible stones. A biliary sphincterotomy was performed. Persistent jaundice and elevated liver enzymes led to an MRCP, which showed a filling defect at the cystic duct-CBD junction. A second ERCP with Spyglass cholangioscopy identified a large, impacted stone at the cystic duct origin, compressing the CBD. Electrohydraulic lithotripsy was performed, and multiple stone fragments were removed (Figure 1A–D). Despite initial improvement, definitive diagnosis remained uncertain. The patient underwent surgical exploration by the hepatobiliary team. Intraoperative findings revealed an intrahepatic gallbladder with a large stone eroding into the bile duct wall, consistent with type III Mirrizi syndrome. A cholecystobiliary fistula and partial destruction of the CBD were identified. The bile duct was resected, and Roux-en-Y hepaticojejunostomy was performed. The patient recovered well and was discharged with follow-up.
Discussion: This case highlights the diagnostic complexity of type III Mirizzi syndrome, a rare entity that is both clinically and radiographically challenging to diagnose. Initial ERCP and MRCP may be inconclusive. Advanced cholangioscopy and surgical exploration are often required. A multi-disciplinary approach must be considered for diagnosis and treatment.
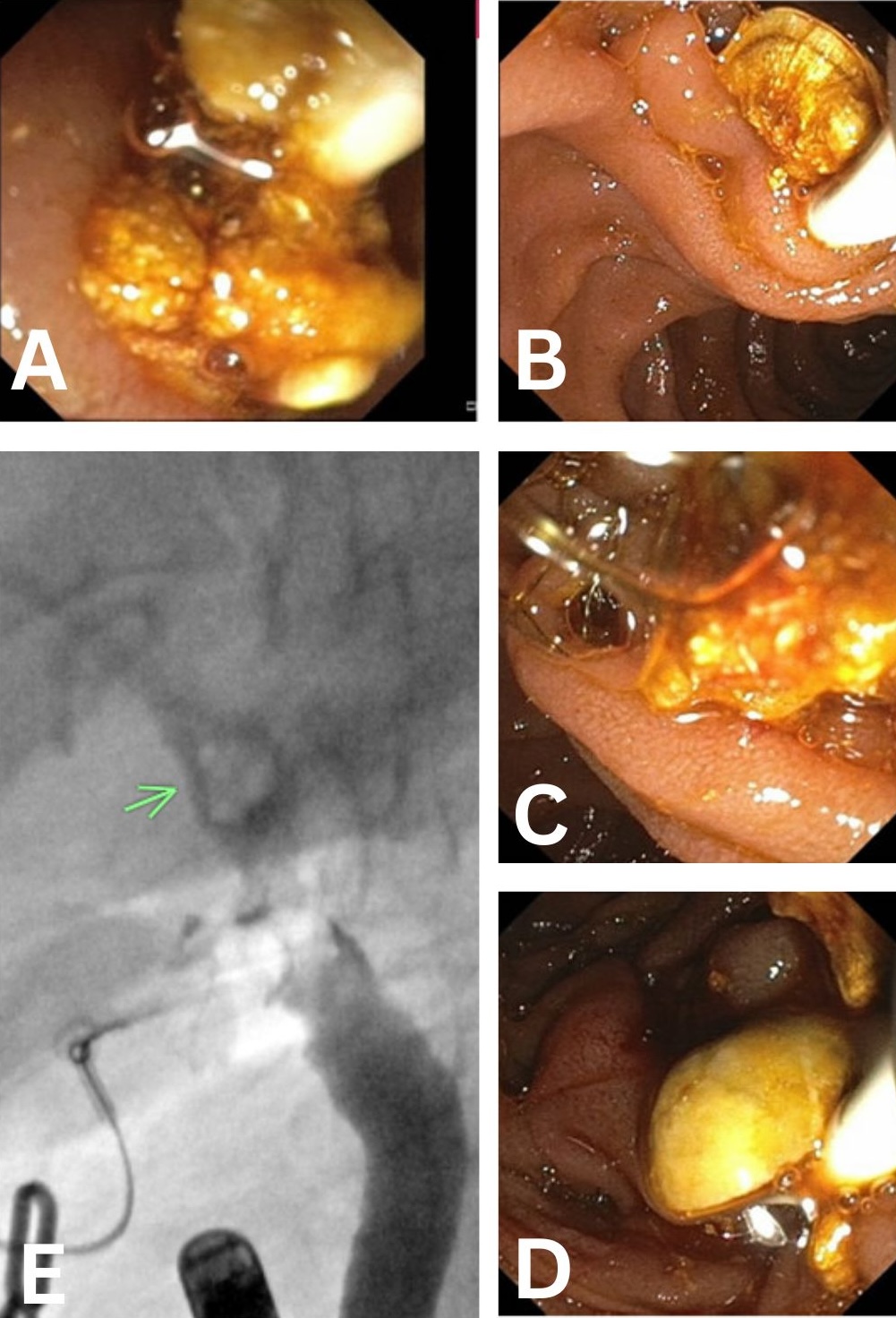
Figure: Endoscopic and fluoroscopic evaluation revealed a large, impacted stone at the cystic duct take-off causing biliary dilation, consistent with Mirizzi syndrome (Figure 1A–D).
Disclosures:
Rishika Trivedi indicated no relevant financial relationships.
Mahmoud Barbarawi indicated no relevant financial relationships.
Prince Shah-Riar indicated no relevant financial relationships.
Tapan Patel indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Murthy Badiga indicated no relevant financial relationships.
Rishika Trivedi, MD1, Mahmoud Barbarawi, MD1, Prince Shah-Riar, MD2, Tapan Patel, MD3, Asif Zamir, MD, FACG4, Murthy Badiga, MD, FACG3. P0199 - Type III Mirizzi Syndrome: A Case of Diagnostic Challenge and Surgical Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

