Sunday Poster Session
Category: Biliary/Pancreas
P0196 - From Gland to Globe: A Case of Hepatic Trespass
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohamed Salih, MD
Cairo University School of Medicine
Cairo, Al Qahirah, Egypt
Presenting Author(s)
Award: ACG Presidential Poster Award
Mohamed Salih, MD1, Omar Al-Radideh, MD2, Bishal Paudel, MD3, Ahmed Al Qady, MD3, Anand Gupte, MD, MS4
1Cairo University School of Medicine, Cairo, Al Qahirah, Egypt; 2University of florida, Gainesville, FL; 3University of Florida, Gainesville, FL; 4University of Florida Health Shands Hospital, Gainesville, FL
Introduction: Intrahepatic pancreatic pseudocysts (IHPP) are exceedingly rare complications of pancreatitis, typically arising from the tracking of pancreatic enzymes into the hepatic parenchyma. This report highlights a unique case of an intrahepatic cystic lesion that demonstrated remarkable growth over a brief period, posing significant diagnostic and management challenges.
Case Description/
Methods: A 57-year-old male with recurrent alcoholic pancreatitis, under surveillance for a resolving pancreatic pseudocyst, presented to ED with progressive abdominal distension. Two months prior, MRI had shown near-resolution of a left upper quadrant pseudocyst and an incidental 1 cm lesion in the left hepatic lobe. On current presentation, CT revealed a large 15 cm unilocular cyst in the left hepatic lobe. (Figure 1)
MRI with MRCP confirmed a large non-enhancing cyst without septations, nodularity, or biliary communication. Blood tests for parasitic, neoplastic, and infectious causes were negative. Prior to planned surgical fenestration for large symptomatic hepatic cyst, Endoscopic ultrasound (EUS) with FNA revealed thick, yellow-brown fluid, and amylase levels >7500 U/L, confirming an IHPP diagnosis. The patient subsequently underwent drainage with endoscopic transmural stent placement with subsequent resolution of symptoms. (Figure 2)
Discussion: IHPPs are rare complications of pancreatitis with no established management guidelines. Their atypical location, varied presentation, and limited data make diagnosis and treatment challenging. Reported strategies include surgery, image-guided drainage, and endoscopic retrograde cholangiopancreatography (ERCP)-guided transpapillary drainage.
The most comprehensive review to date, by Demeusy et al. (2016), analyzed 54 cases of IHPPs, nearly all of which required active intervention. Percutaneous drainage, often combined with pancreatic duct stenting, was the most frequently employed approach. Notably, EUS-guided drainage was not utilized in any of the cases reviewed.
To our knowledge, this is the first reported case of successful EUS-guided transgastric cystogastrostomy for IHPP, with resolution both clinically and radiologically. This novel approach offers a less invasive option and expands the therapeutic landscape.
This case underscores the diagnostic uncertainty and management complexity of IHPPs, highlighting the need for individualized, multidisciplinary care and illustrating the expanding role of EUS in managing complex pancreatic fluid collections.
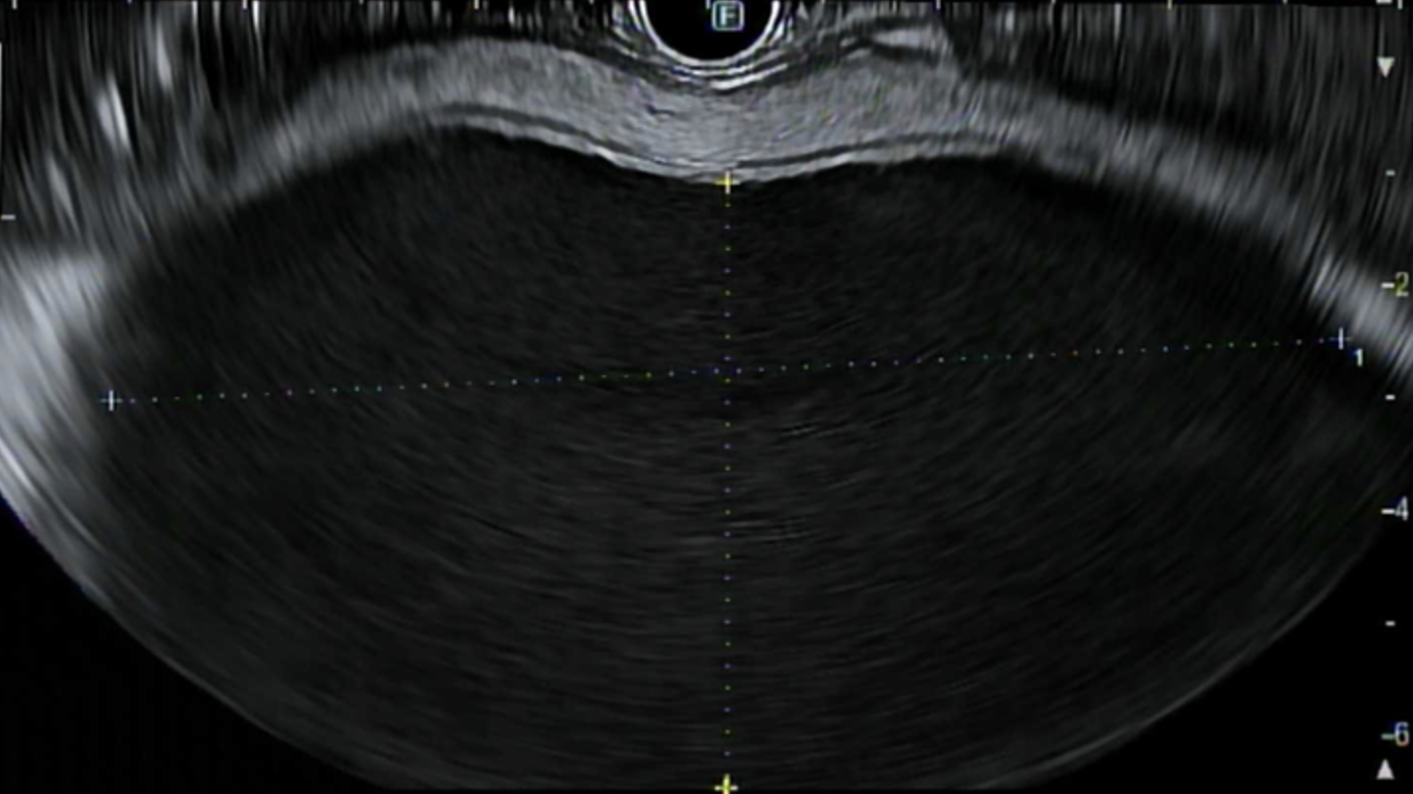
Figure: Figure 1. EUS image showing an IHPP
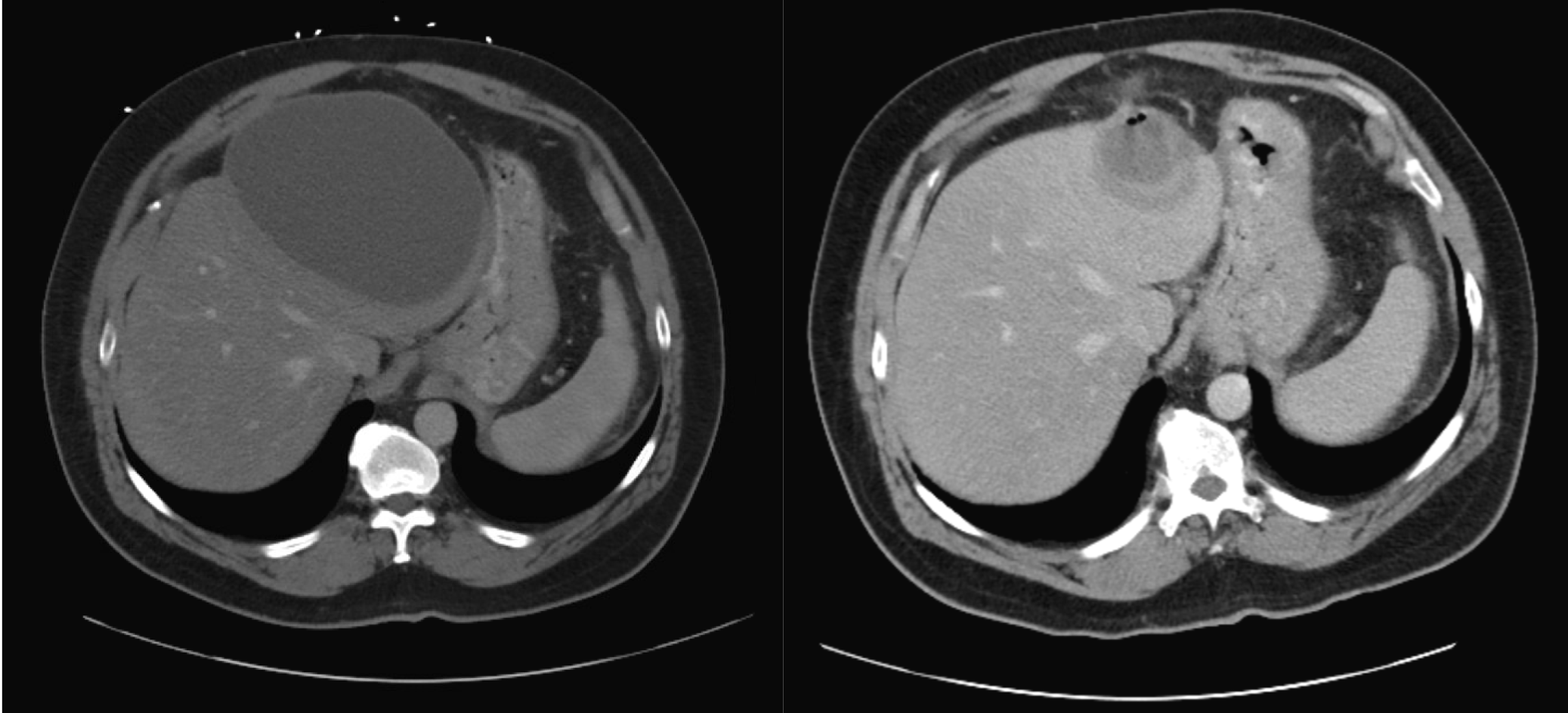
Figure: Figure 2. CT scans of IHPP pre- and post-EUS drainage. Left: pre-drainage showing the intrahepatic pseudocyst. Right: post-drainage showing resolution of the pseudocyst.
Disclosures:
Mohamed Salih indicated no relevant financial relationships.
Omar Al-Radideh indicated no relevant financial relationships.
Bishal Paudel indicated no relevant financial relationships.
Ahmed Al Qady indicated no relevant financial relationships.
Anand Gupte indicated no relevant financial relationships.
Mohamed Salih, MD1, Omar Al-Radideh, MD2, Bishal Paudel, MD3, Ahmed Al Qady, MD3, Anand Gupte, MD, MS4. P0196 - From Gland to Globe: A Case of Hepatic Trespass, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mohamed Salih, MD1, Omar Al-Radideh, MD2, Bishal Paudel, MD3, Ahmed Al Qady, MD3, Anand Gupte, MD, MS4
1Cairo University School of Medicine, Cairo, Al Qahirah, Egypt; 2University of florida, Gainesville, FL; 3University of Florida, Gainesville, FL; 4University of Florida Health Shands Hospital, Gainesville, FL
Introduction: Intrahepatic pancreatic pseudocysts (IHPP) are exceedingly rare complications of pancreatitis, typically arising from the tracking of pancreatic enzymes into the hepatic parenchyma. This report highlights a unique case of an intrahepatic cystic lesion that demonstrated remarkable growth over a brief period, posing significant diagnostic and management challenges.
Case Description/
Methods: A 57-year-old male with recurrent alcoholic pancreatitis, under surveillance for a resolving pancreatic pseudocyst, presented to ED with progressive abdominal distension. Two months prior, MRI had shown near-resolution of a left upper quadrant pseudocyst and an incidental 1 cm lesion in the left hepatic lobe. On current presentation, CT revealed a large 15 cm unilocular cyst in the left hepatic lobe. (Figure 1)
MRI with MRCP confirmed a large non-enhancing cyst without septations, nodularity, or biliary communication. Blood tests for parasitic, neoplastic, and infectious causes were negative. Prior to planned surgical fenestration for large symptomatic hepatic cyst, Endoscopic ultrasound (EUS) with FNA revealed thick, yellow-brown fluid, and amylase levels >7500 U/L, confirming an IHPP diagnosis. The patient subsequently underwent drainage with endoscopic transmural stent placement with subsequent resolution of symptoms. (Figure 2)
Discussion: IHPPs are rare complications of pancreatitis with no established management guidelines. Their atypical location, varied presentation, and limited data make diagnosis and treatment challenging. Reported strategies include surgery, image-guided drainage, and endoscopic retrograde cholangiopancreatography (ERCP)-guided transpapillary drainage.
The most comprehensive review to date, by Demeusy et al. (2016), analyzed 54 cases of IHPPs, nearly all of which required active intervention. Percutaneous drainage, often combined with pancreatic duct stenting, was the most frequently employed approach. Notably, EUS-guided drainage was not utilized in any of the cases reviewed.
To our knowledge, this is the first reported case of successful EUS-guided transgastric cystogastrostomy for IHPP, with resolution both clinically and radiologically. This novel approach offers a less invasive option and expands the therapeutic landscape.
This case underscores the diagnostic uncertainty and management complexity of IHPPs, highlighting the need for individualized, multidisciplinary care and illustrating the expanding role of EUS in managing complex pancreatic fluid collections.
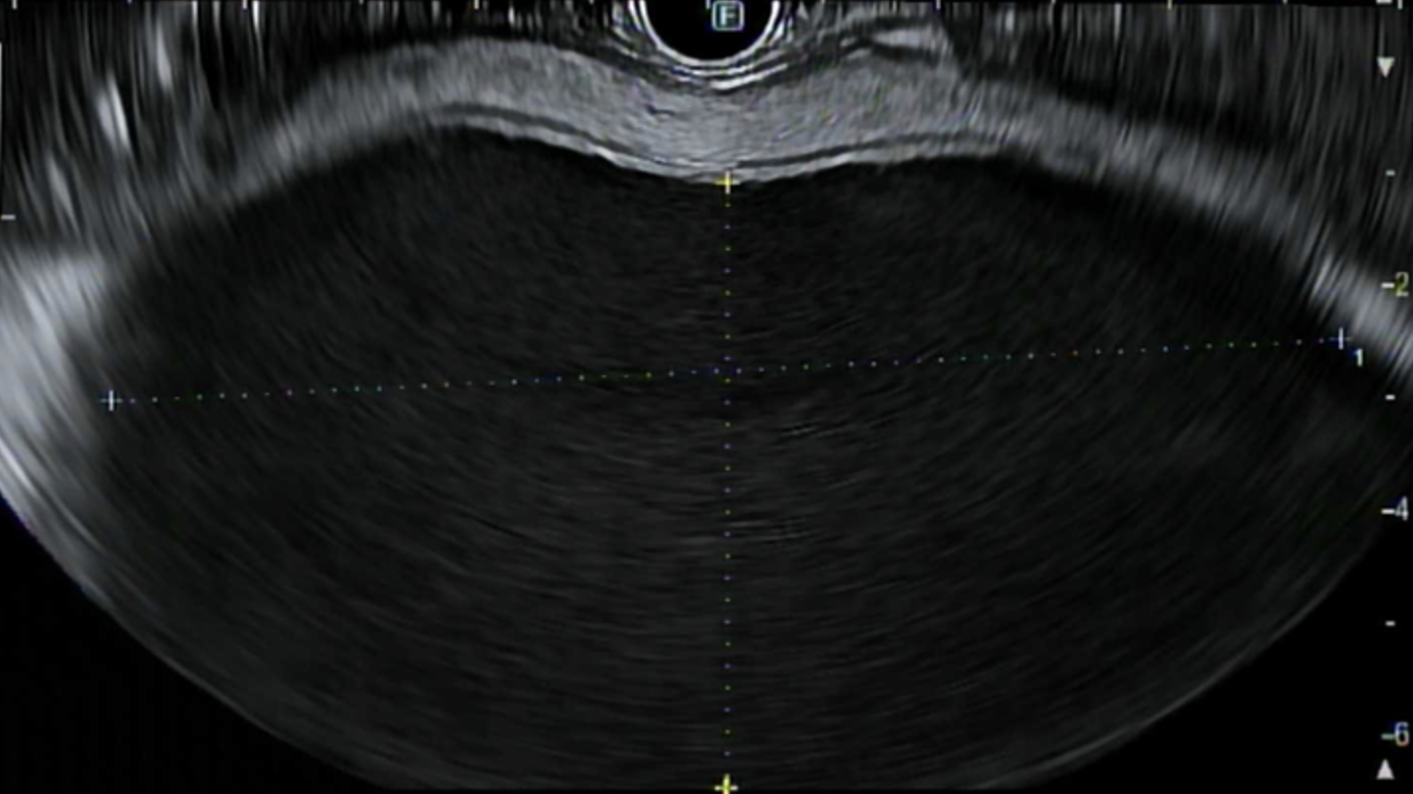
Figure: Figure 1. EUS image showing an IHPP
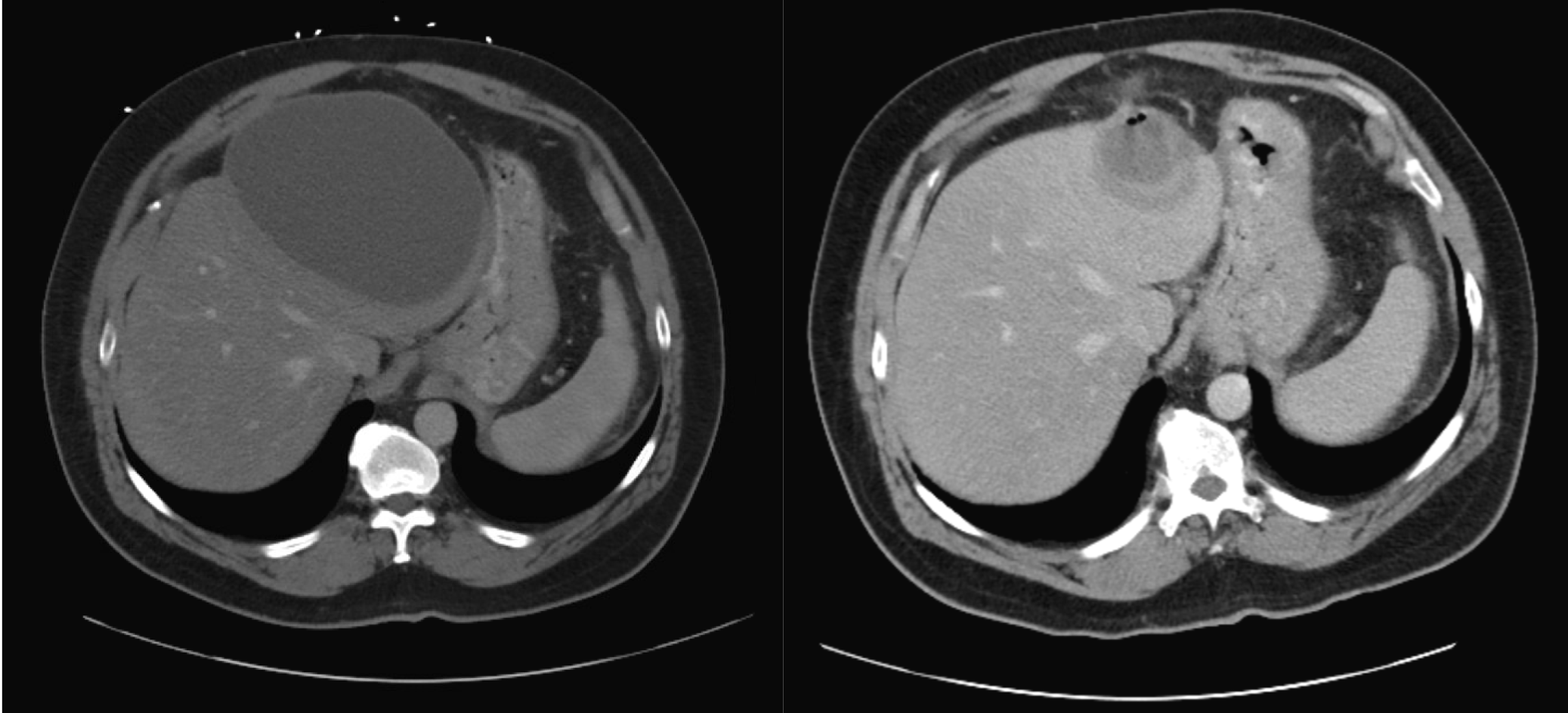
Figure: Figure 2. CT scans of IHPP pre- and post-EUS drainage. Left: pre-drainage showing the intrahepatic pseudocyst. Right: post-drainage showing resolution of the pseudocyst.
Disclosures:
Mohamed Salih indicated no relevant financial relationships.
Omar Al-Radideh indicated no relevant financial relationships.
Bishal Paudel indicated no relevant financial relationships.
Ahmed Al Qady indicated no relevant financial relationships.
Anand Gupte indicated no relevant financial relationships.
Mohamed Salih, MD1, Omar Al-Radideh, MD2, Bishal Paudel, MD3, Ahmed Al Qady, MD3, Anand Gupte, MD, MS4. P0196 - From Gland to Globe: A Case of Hepatic Trespass, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

