Sunday Poster Session
Category: Biliary/Pancreas
P0195 - Multidisciplinary Management of a Pancreatic Mucinous Cystic Neoplasm During Pregnancy: A Gastroenterologist’s Role in Diagnosis and Guidance
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Meagan H. Phox, DO (she/her/hers)
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Meagan H. Phox, DO, John Thesing, DO, Nathan Tofteland, MD
University of Kansas School of Medicine, Wichita, KS
Introduction: Mucinous cystic neoplasms (MCNs) of the pancreas are rare, typically arising in women around the age of 40 and seldom encountered during pregnancy. These cystic tumors are defined by the presence of ovarian-type stroma and usually occur in the pancreatic body or tail without ductal communication. Unique challenges arise when MCNs are discovered in pregnancy due to diagnostic uncertainty, fetal considerations, and timing of surgical intervention.
Case Description/
Methods: We report the case of a 25-year-old primigravida at 19.3 weeks gestation who was found to have a large mixed cystic and solid mass initially presumed to be of ovarian origin. Exploratory laparotomy revealed the mass to originate from the left upper retroperitoneum, prompting further evaluation with magnetic resonance imaging (MRI), which suggested a solid pseudopapillary neoplasm of the pancreatic body and tail (Figure 1 and 2). A multidisciplinary team, including gastroenterology, maternal-fetal medicine, and surgery, collaborated on a management plan that prioritized maternal and fetal safety. The patient underwent endoscopic ultrasound with fine-needle aspiration (EUS-FNA) at 21 weeks, yielding fluid with elevated CEA (1182 ng/mL) but no malignant cells. After extensive counseling, the patient opted for postpartum surgical resection. At one month postpartum, she underwent successful distal pancreatectomy and splenectomy. Gross pathology revealed a cystic mass measuring 19 x 16 x 15 cm. Final pathology confirmed a MCN with ovarian-type stroma and no evidence of high-grade dysplasia or malignancy.
Discussion: This case highlights the diagnostic and management complexities of pancreatic MCNs in pregnancy, including the utility of safe imaging modalities, the role of EUS-FNA in risk stratification, and the importance of individualized decision-making. Gastroenterology played a pivotal role in diagnostic clarification and therapeutic planning with EUS-FNA, providing critical data while balancing fetal safety. As pancreatic MCNs are rarely encountered in this setting, this case underscores the value of endoscopic evaluation and shared decision-making in guiding management on an individualized basis.
Factors such as cyst size, imaging characteristics, and gestational age must all be weighed when determining timing of intervention. Postpartum resection in this case led to a favorable maternal and fetal outcome, underscoring the effectiveness of a multidisciplinary, case-specific approach.
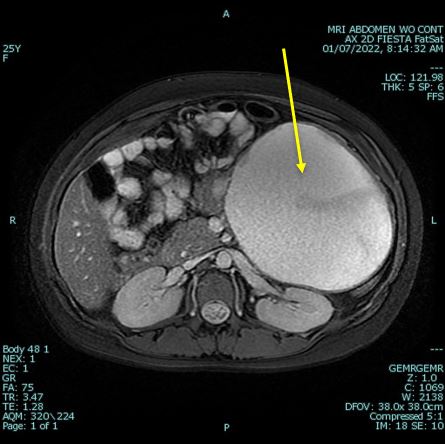
Figure: Figure 1. Axial MRI view of abdomen showing concern for solid pseudopapillary neoplasm of body/tail of pancreas (arrow).
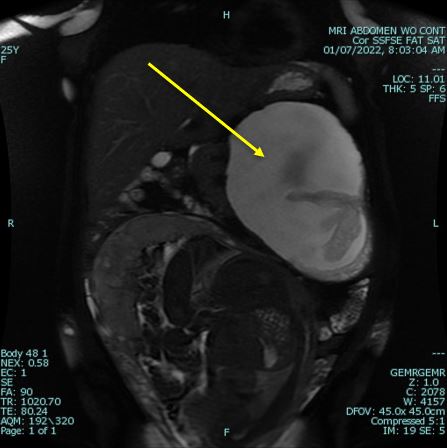
Figure: Figure 2. Coronal MRI view of abdomen showing concern for solid pseudopapillary neoplasm of body/tail of pancreas (arrow).
Disclosures:
Meagan Phox indicated no relevant financial relationships.
John Thesing indicated no relevant financial relationships.
Nathan Tofteland indicated no relevant financial relationships.
Meagan H. Phox, DO, John Thesing, DO, Nathan Tofteland, MD. P0195 - Multidisciplinary Management of a Pancreatic Mucinous Cystic Neoplasm During Pregnancy: A Gastroenterologist’s Role in Diagnosis and Guidance, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Kansas School of Medicine, Wichita, KS
Introduction: Mucinous cystic neoplasms (MCNs) of the pancreas are rare, typically arising in women around the age of 40 and seldom encountered during pregnancy. These cystic tumors are defined by the presence of ovarian-type stroma and usually occur in the pancreatic body or tail without ductal communication. Unique challenges arise when MCNs are discovered in pregnancy due to diagnostic uncertainty, fetal considerations, and timing of surgical intervention.
Case Description/
Methods: We report the case of a 25-year-old primigravida at 19.3 weeks gestation who was found to have a large mixed cystic and solid mass initially presumed to be of ovarian origin. Exploratory laparotomy revealed the mass to originate from the left upper retroperitoneum, prompting further evaluation with magnetic resonance imaging (MRI), which suggested a solid pseudopapillary neoplasm of the pancreatic body and tail (Figure 1 and 2). A multidisciplinary team, including gastroenterology, maternal-fetal medicine, and surgery, collaborated on a management plan that prioritized maternal and fetal safety. The patient underwent endoscopic ultrasound with fine-needle aspiration (EUS-FNA) at 21 weeks, yielding fluid with elevated CEA (1182 ng/mL) but no malignant cells. After extensive counseling, the patient opted for postpartum surgical resection. At one month postpartum, she underwent successful distal pancreatectomy and splenectomy. Gross pathology revealed a cystic mass measuring 19 x 16 x 15 cm. Final pathology confirmed a MCN with ovarian-type stroma and no evidence of high-grade dysplasia or malignancy.
Discussion: This case highlights the diagnostic and management complexities of pancreatic MCNs in pregnancy, including the utility of safe imaging modalities, the role of EUS-FNA in risk stratification, and the importance of individualized decision-making. Gastroenterology played a pivotal role in diagnostic clarification and therapeutic planning with EUS-FNA, providing critical data while balancing fetal safety. As pancreatic MCNs are rarely encountered in this setting, this case underscores the value of endoscopic evaluation and shared decision-making in guiding management on an individualized basis.
Factors such as cyst size, imaging characteristics, and gestational age must all be weighed when determining timing of intervention. Postpartum resection in this case led to a favorable maternal and fetal outcome, underscoring the effectiveness of a multidisciplinary, case-specific approach.
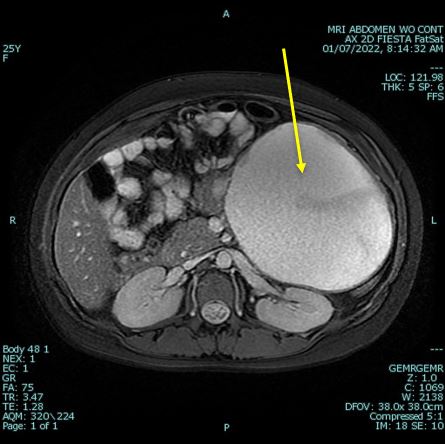
Figure: Figure 1. Axial MRI view of abdomen showing concern for solid pseudopapillary neoplasm of body/tail of pancreas (arrow).
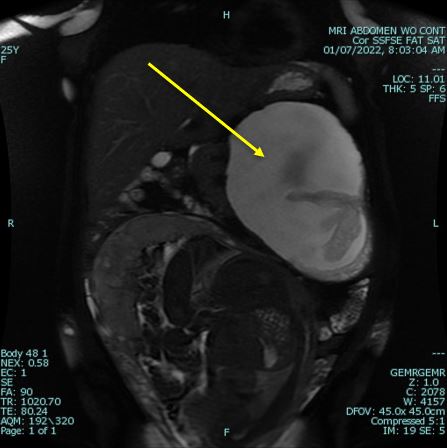
Figure: Figure 2. Coronal MRI view of abdomen showing concern for solid pseudopapillary neoplasm of body/tail of pancreas (arrow).
Disclosures:
Meagan Phox indicated no relevant financial relationships.
John Thesing indicated no relevant financial relationships.
Nathan Tofteland indicated no relevant financial relationships.
Meagan H. Phox, DO, John Thesing, DO, Nathan Tofteland, MD. P0195 - Multidisciplinary Management of a Pancreatic Mucinous Cystic Neoplasm During Pregnancy: A Gastroenterologist’s Role in Diagnosis and Guidance, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

